Fig. 17.1
Arthroscopic view of a left shoulder through a posterior portal. This patient has sustained more than 50 subluxations. The axillary nerve is clearly identifiable (white asterisk). There is no more capsule or inferior glenohumeral ligament, and the subscapularis muscle is hardly recognizable
Arthroscopic shoulder techniques have conferred significant advantages on open techniques. Visualization is improved, allowing easier identification and treatment of associated intra-articular pathology, such as humeral avulsion of the glenohumeral ligament (HAGL) or superior labrum anteroposterior (SLAP) lesions. Moreover, an arthroscopic approach reduces surgical trauma, particularly the need to detach subscapularis tendon. With these advantages, arthroscopic stabilization has become a viable and frequently used procedure to address anterior instability [10–13].
Chapters 1, 2, and 3 of this book have addressed shoulder anatomy, biomechanics, epidemiology, and physical examination, respectively. This chapter will therefore focus on the pathology, classification, and natural history and treatment of primary traumatic anterior shoulder instability. We subsequently present our current therapeutic techniques and provide a stepwise approach to this condition that is frequently encountered by the orthopedic surgeon.
17.2 Pathoanatomy, Biomechanics, and Preferred Classification
Traumatic anterior shoulder instability in the athlete usually occurs with an anteriorly directed force applied to an abducted and externally rotated arm, or from a direct blow. During a traumatic anterior dislocation, many of the passive and active stabilizers may be damaged. The glenoid labrum, the glenohumeral ligaments, and the glenohumeral joint capsule representing the soft tissue passive stabilizers will be injured; an avulsion of the anterior labrum, the classic Bankart lesion (Fig. 17.2) or its variations (glenolabral articular disruption (GLAD), Perthes, anterior labroligamentous periosteal sleeve avulsion (ALPSA)), is almost invariably present [14–16] although it does not produce instability in isolation [17]. The anteroinferior glenohumeral ligaments and the capsule can be detached from the glenoid rim, and a plastic deformation of the glenohumeral ligaments and an HAGL lesion [18] (Fig. 17.3) are other common features. The plastic deformation of these structures becomes progressively more severe with subsequent episodes [19–21]. The middle glenohumeral ligament functions to limit both anterior and posterior translation of the arm at 45° of abduction and 45° of external rotation, whereas the inferior glenohumeral ligament resists translation of the arm in greater degrees of abduction [22].
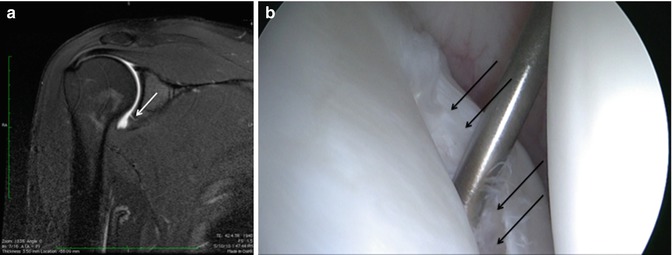
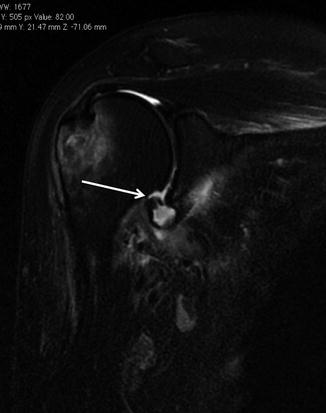
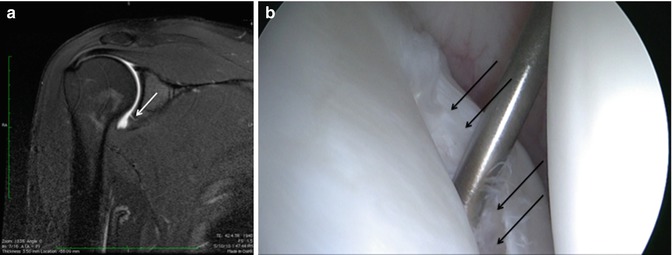
Fig. 17.2
(a) Coronal MRI of a right shoulder showing disruption of the anteroinferior glenoid labrum (white arrow). (b) Arthroscopic image confirming discontinuity of the glenoid surface and redundant anterior labrum (black arrows)
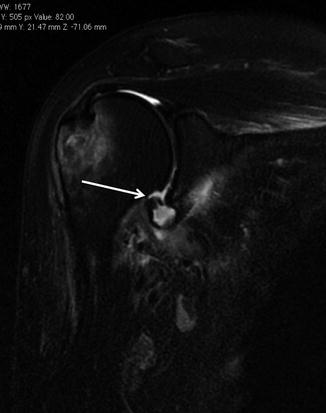
Fig. 17.3
Coronal T2 MRI of a right shoulder. The white arrow highlights an HAGL lesion. This lesion must be recognized as an isolated retensioning of the inferior glenohumeral ligament will lead to recurrent instability
In addition to progressive soft tissue injury, recurrent dislocations can facilitate bony injury [23, 24]. Bony lesions are frequent in recurrent cases and may include defects of the glenoid (bony Bankart or bevelling of the anterior glenoid resulting in loss of glenoid concavity), impaction of the posterolateral humeral head (Hill-Sachs lesion), or even coracoid or proximal humerus fractures (Fig. 17.4) [5]. Given that the average glenoid diameter is about 24 mm, a 6-mm-wide or larger fragment of the glenoid will typically equate to a 25 % or more of the articular surface and is considered a large bony fragment [25, 26]. Such significant glenoid bone loss can be viewed arthroscopically as an inverted-pear configuration. All Hill-Sachs lesions are by definition engaging lesions (since it has engaged at least once). Thus the notion of “engaging” versus “non-engaging” can lead to significant confusion. Some have proposed that the important lesions are those that engage in the 90-90 position. A more recent proposal by DiGiacomo et al. is to describe the lesions as “on-track” or “off-track” to determine the need for remplissage in addition to arthroscopic Bankart repair in the setting of glenoid bone loss of less than 25 % [27]. This view is discussed in more detail in subsequent sections.


Fig. 17.4
(a) Sagittal view of a CT arthrogram of a left shoulder demonstrates a significant Bankart fracture (white arrow) that produces an “inverted-pear” glenoid. (b) Plain anteroposterior radiograph reveals an anteroinferior glenohumeral dislocation with an “engaged” Hill-Sachs lesion of the humerus
Finally, the active restraint, mainly a lesion of the rotator cuff above the age of 40, will complete this complex situation [28, 29]. Since rotator cuff tears associated with instability usually occur in the nonathletic population, this situation is not discussed in detail in this chapter.
The degree, nature, and combination of the injury in athletes are highly variable. It would appear, therefore, that reducing the incidence of recurrent instability from a pathoanatomical viewpoint would be desirable. All the damage to the osseous and soft tissue stabilizers of the shoulder, as well as vascular and neurological impairment, must be detected and analyzed in order to offer to the patient the best treatment option.
Instability can be classified as primary or recurrent. The latter can be further classified as dislocation, subluxation, apprehension, or an unstable painful shoulder. In frank dislocation, the articular surfaces of the joint are completely separated. Subluxation is defined as symptomatic translation of the humeral head on the glenoid without complete separation of the articular surfaces. Apprehension is classically defined by fear of imminent dislocation in the 90-90 position. This could correspond to an instability phenomena or a persistent fear after a successful glenohumeral stabilization [30]. The unstable painful shoulder presents as pain only (as opposed to a sense of instability) during an apprehension maneuver at clinical examination [31, 32]. The majority of these patients have a history of trauma, but simply do not report a clear history of trauma. Careful preoperative and/or arthroscopic examination will show that the majority of these patients also have evidence of instability (i.e., labral tear, glenoid fracture, or Hill-Sachs lesion).
17.3 Clinical Presentation and Essential Physical Examination
The history should document age, hand dominance, occupation, participation in sporting activities, initial mechanism of the injury, the position of the arm (extension, abduction, and external rotation favors anterior dislocation), how long the shoulder stays out, the method of reduction, the number of recurrences (frank dislocation vs. subluxation), and the effectiveness of a previous nonoperative or operative treatment. The diagnosis of recurrent traumatic anterior glenohumeral instability is usually made easily on the basis of the history, radiographs, and a positive apprehension sign. However, when collision athletes are seen, care should be taken because they may not experience clear dislocation or subluxation and only complain of pain or weakness as discussed previously.
A comprehensive physical examination is essential. The aim is to define the direction of instability and the presence of an associated pathologic hyperlaxity and to exclude neurological and rotator cuff impairment. Passive and active glenohumeral range of motion should be assessed. Rotator cuff examination includes strength tests such as belly-press [35], bear hug [36], and Jobe [37, 38] tests and strength in external rotation against resistance. The authors do not systematically perform tests for anterior and superior labral lesions as they have a poor sensitivity and specificity [39]. The neurovascular status of the upper extremity is assessed, particularly with regard to the axillary nerve since there is a high incidence of injury to this nerve with traumatic instability.
Laxity is a normal, physiologic, and asymptomatic finding that corresponds to translation of the humeral head in any direction to the glenoid [40]. Laxity is assessed with the sulcus sign, anteroposterior drawer, hyperabduction tests, and external rotation elbow at side. The two former tests are only qualitative and are not routinely performed by the authors. Hyperlaxity is constitutional, multidirectional, bilateral, and asymptomatic. Hyperlaxity of the shoulder is probably best defined as external rotation elbow at the side equal or greater than 85 [41]. This non-pathological finding is a risk factor for instability but does not by itself demand treatment unless there is clear pathological laxity. Pathological laxity of the inferior glenohumeral ligament is observed when passive abduction in neutral rotation in the glenohumeral joint is above 105°, when there is apprehension above 90° of abduction, or if a difference of more than 20° between the two shoulders is noted [42]. For apprehension the patient is initially invited to demonstrate his or her functional problem to the examiner (no-touch examination). This examination alone, coupled with a good history, often provides the information needed. However, if the direction of the instability remains unclear, the apprehension (crank) test, an abducted and externally rotated position suggestive of anterior instability, is performed. Fear of dislocation or a feeling of anterior pain is considered positive for damage to the anterior capsulolabral complex, which should be relieved with posterior translation of the humerus (relocation maneuver). To summarize, the physical examination demonstrates instability if the apprehension test is positive, multidirectional hyperlaxity when the external rotation at side is equal or above 85°, and a pathological laxity of the inferior glenohumeral ligament if the hyperabduction test is positive.
17.4 Essential Radiology
Radiographic evaluation is based on whether the dislocation is acute or chronic.
17.4.1 Acute Dislocation
Three-view plain radiographs, including true anteroposterior of the glenohumeral joint, scapular Y (scapular lateral), and Velpeau axillary [43] views, are the mainstay of imaging in the setting of traumatic anterior instability. The latter view is crucial to obtain, as the first two alone do not allow to exclude a dislocation. The goal is to confirm the direction of dislocation and to evaluate associated lesions (Fig. 17.5). Once reduced, further imaging studies in the setting of an associated fracture (computed tomography (CT)), suspicion of rotator cuff injury (ultrasonography or MRI), or vascular impairment (injected CT) may be warranted.


Fig. 17.5
(a) Plain radiograph of a right shoulder fracture dislocation. The anterior Bankart fracture (white arrow) was overlooked at the initial management. (b) The fracture has been fixed with a plate, but the joint will remain unstable if the Bankart fracture (white arrow) is neglected
17.4.2 Recurrent Dislocation
The first step is to analyze, if available, plan radiographs with the shoulder out of joint to confirm the direction of instability. Plain radiographs including anteroposterior in neutral, internal, and external rotations, scapular Y, and Bernageau [44] views are then obtained. Bone loss, static instability, post-dislocation arthropathy, and coracoid nonunion (if a Latarjet procedure is planned) have to be estimated. Magnetic resonance imaging (MRI) arthrogram is useful to assess for an anterior labral tear and Hill-Sachs lesion which confirms the instability. Associated intra-articular pathology such as SLAP, HAGL, and rotator cuff lesions or a paralabral cyst is also assessed (Fig. 17.6) [45]. The evaluation is completed by a 3D CT arthrogram in the setting of recurrent instability in which there is primary concern for bone loss. The extent of both glenoid bone loss and Hill-Sachs lesions is best assessed by CT scan and is used to determine the need for Latarjet as opposed to arthroscopic Bankart repair (Fig. 17.7).
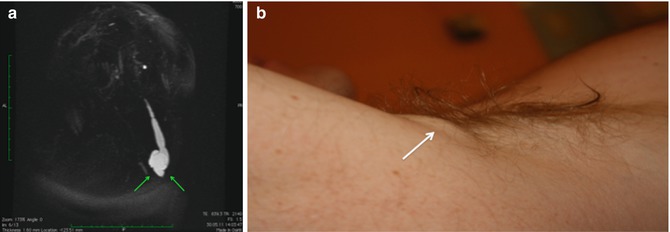
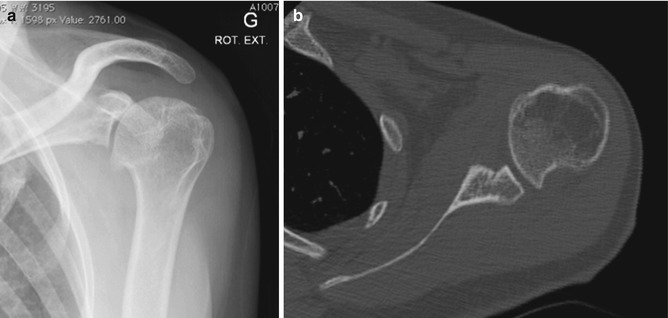
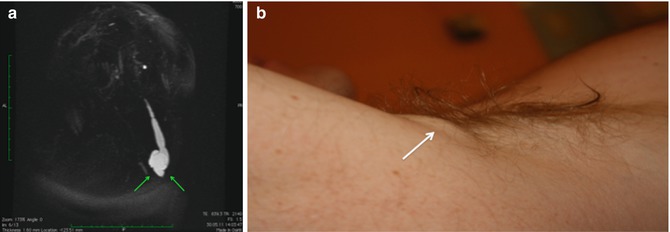
Fig. 17.6
(a) 3D maximum intensity projection reconstruction showing a remarkably voluminous cyst (green arrows) dissecting 9 cm from the glenoidal labrum through the long head of the triceps muscle (reproduced/reprinted with permission). (b) The patient complains from a lump (white arrow) in his axillary fold.
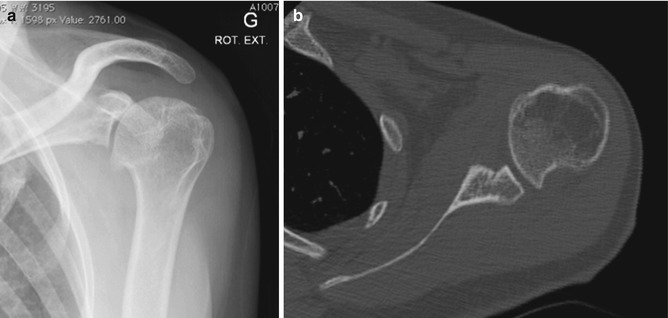
Fig. 17.7
(a) Anteroposterior plain radiographs of a left shoulder in a 32-year-old woman presenting with recurrent dislocations. Dislocation arthropathy Samilson [46] b is obvious. (b) CT scan of the same shoulder demonstrates significant glenoid and humeral bone loss
17.5 Treatment Options
17.5.1 Treatment of Acute First Traumatic Dislocations
The first step, whenever possible, is to obtain a complete set of radiographs before attempting a reduction. This will allow an assessment of the type of dislocation and associated bone injuries. Attempting to reduce a fracture dislocation can have troublesome clinical and legal consequences (Fig. 17.8). Exceptions are an impossibility to have reasonably fast access to radiology or a patient with neurological impairment. Because of the possible association of nerve injuries [47] and, to a lesser extent, vascular injuries (Fig. 17.9) [48], an essential part of the physical examination is an assessment of the neurovascular status of the upper extremity before reduction. There are numerous appropriate methods of reduction that have been described [49–58]. The second step is to use the technique of closed reduction which is mastered by the doctor who will perform the maneuver. The glenohumeral joint should be reduced as gently and expeditiously as possible. In the case of fracture dislocation, the reduction is best performed under general anesthesia to have adequate muscle relaxation. After reducing the dislocation, plain radiographs are obtained to verify the adequacy of the reduction. Results concerning conservative treatment are still debatable [59]. A stable shoulder is obtained at 10 years in only half of the patients with conservative treatment [60]. However, recurrence rate is highly dependent on age and activity of the patient; studies have reported a 72–95 % recurrence in patients under 20 years of age and 70–82 % recurrence between the ages of 20 and 30 years [61–66] and only 30 % in those over 30 years of age [67]. Many patients above the age of 30 would consequently undergo unnecessary surgery if proposed after the first dislocation. Conservative treatment after the first traumatic anterior dislocation may be thus recommended for patients who are not actively engaged in sports, above the age of 30 years old [61], with a low functional demand, with an associated humeral fracture [60], or for the athlete with an in-season shoulder dislocation [4]. For the latter situation, athletes are allowed to attempt to return to competition provided there is enough time left in the season to permit adequate rehabilitation with progression to sport-specific drills. Rehabilitation including return of range of motion and strengthening of dynamic stabilizers may facilitate return to sport within several weeks. Motion-limiting braces that prevent extreme shoulder abduction, extension, and external rotation are often prescribed as it may reduce the risk of recurrence. However, such braces are not well tolerated in patients who must complete certain overhead tasks such as throwing. Moreover, a second in-season shoulder dislocation should lead to removal from sport and proceed with stabilization so as to avoid further glenohumeral damage.
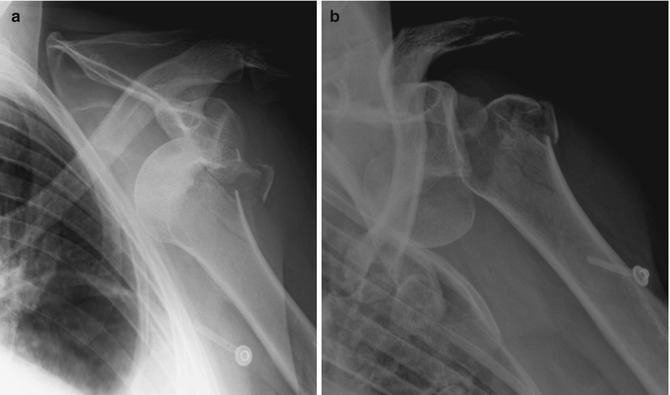
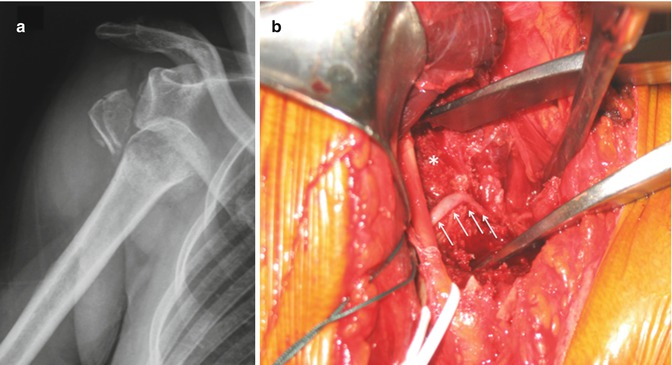
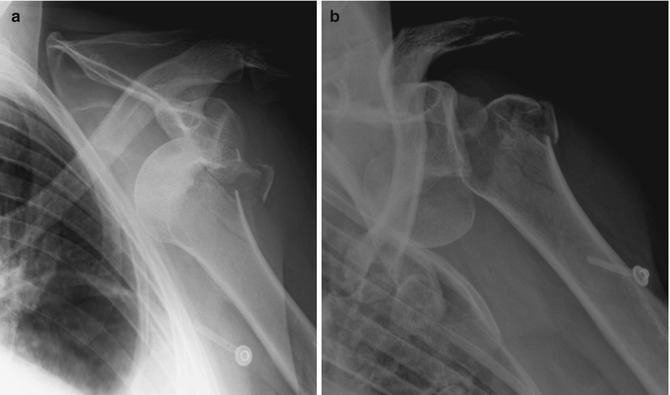
Fig. 17.8
(a) An anteroposterior plain radiograph of a left shoulder shows an anterior dislocation with a nondisplaced humeral neck fracture on the prereduction radiographs. (b) Radiographs after attempting a closed reduction without adequate muscle relaxation reveal displacement of the fracture with the humeral head remaining anteriorly
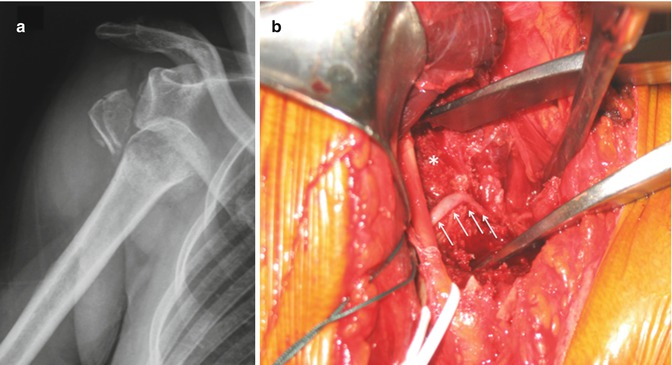
Fig. 17.9
(a) A 54-year-old patient sustained a fracture dislocation of the right shoulder. At clinical examination, no peripheral pulse was palpated. (b ) During open reduction, the axillary artery (white arrows) was found kinked around the fractured humeral head
A number of studies have compared nonoperative treatment and arthroscopic stabilization. Overall, these studies report a sevenfold reduction in the risk of recurrent instability after arthroscopic stabilization, when compared with nonoperative treatment for the first-time dislocator [59]. A Cochrane review concluded that early surgical intervention is warranted in young adults aged less than 30 years engaged in highly demanding physical activities [68]. Consequently, for patients who are actively engaging in a collision or contact or overhead sport, who risk their life in case of a new dislocation (e.g., firemen, proponents of extreme sports like base jumping and climbing), with associated glenoid fracture, static anterior subluxation, an interposed tissue, or a nonconcentric reduction, or patients with rotator cuff avulsion, conservative measures are usually inadequate and prompt surgery is indicated.
17.5.2 Surgical Treatment of Acute or Recurrence Traumatic Anterior Instability
Recurrent dislocation is not trivial. Each episode creates new lesions and increases the risk of developing dislocation arthropathy. The concept of early operative surgical management of the first-time dislocator has consequently been introduced to address the high recurrence rate in the young athletic population. A surgery should be proposed, as having the ultimate aim to achieve a pain-free stable shoulder while preserving range of motion. The surgical approach is based on the extent of bone loss and patient-specific risk factors for recurrence.
Boileau et al. proposed a simple 10-point scale scoring system (instability severity index score (ISIS)) based on factors derived from a preoperative questionnaire, physical examination, and anteroposterior radiographs to determine the risk of treatment failure following isolated arthroscopic Bankart repair (Table 17.1) [69]. In this model an ISIS of 3 or less was associated with a 5 % rate of recurrence, an ISIS of 4–6 was associated with a 10 % rate of recurrence, and an ISIS over 6 was associated with a 70 % rate of recurrence. Although it has imperfections, this score, validated since [70], has merit to easily remind the clinician of factors that are important to consider when evaluating a patient.
Table 17.1
The instability severity index score is based on a preoperative questionnaire, clinical examination, and radiographs
Prognostic factors | Points |
|---|---|
Age at surgery (years) | |
<20 | 2 |
≥20 | 0 |
Degree of sport participation (preoperative) | |
Competitive | 2 |
Recreational or none | 0 |
Type of sport (preoperative) | |
Contact or forced overhead | 2 |
Other | 0 |
Shoulder hyperlaxity | |
Shoulder hyperlaxity (anterior or inferior) | 1 |
Normal laxity | 0 |
Hill-Sachs on AP radiograph | |
Visible in external rotation | 2 |
Not visible in external rotation | 0 |
Glenoid loss of contour on AP radiograph | |
Loss of contour | 2 |
No lesion | 0 |
Total (points) | |
The aim of a Bankart repair is to restore anatomy by reattaching the labrum to the glenoid and tighten the inferior glenohumeral ligament by shifting from inferior to superior. It was previously believed that a minimum of three double-loaded suture anchors had to be used [71]. However, a recent study demonstrated that one to two anchors are enough [72]. One must take caution with the latter as the position of the anchors is probably the most important factor; in other words, the placement of three anchors likely reflects the fact that the surgeon is adequately placing inferior anchors and obtaining an inferior to superior shift of the pathological lesion. Although this surgery can be performed in an open manner, the advantage of an arthroscopic approach is that it preserves the subscapularis and allows assessment of associated pathology [73–75]. The literature demonstrates that patients with low risk of recurrence will benefit from either an anatomic open or arthroscopic repair with an acceptable rate of recurrence [76].
Remplissage has been described by Connoly [77] and may be used as an adjunct to arthroscopic Bankart repair in the setting of a large Hill-Sachs lesion with glenoid bone loss of <25 %. This technique consists of a posterior capsulodesis and infraspinatus tenodesis that fills the Hill-Sachs lesion. The purpose is to render the Hill-Sachs lesion extracapsular, avoiding its engagement. Wolf and Arianjam and Boileau et al. recently presented encouraging mid- to long-term results of arthroscopic remplissage and concomitant anterior Bankart repair [13, 78]. However, the indication for remplissage has not been well defined. Recently, DiGiacomo et al. introduced the concept of an “on-track vs. off-track” Hill-Sachs lesion [27]. This view incorporates the concept of the glenoid track by Yamamoto et al. which describes the contact of the posterior humeral head with the glenoid during abduction [79]. Based on study in normal individuals, this zone of contact or “glenoid track” averages 83 % of the glenoid width. In the proposal of DiGiacomo et al., the normal glenoid diameter is determined via CT scan of the contralateral glenoid or arthroscopic assessment (by doubling the distance from the glenoid bare area to the posterior glenoid rim). Then, the glenoid track is determined by multiplying the normal glenoid diameter by .83 and subtracting the anterior glenoid bone defect. Finally, the distance from the medial margin of the infraspinatus to the most medial aspect of the Hill-Sachs lesion (or Hill-Sachs interval) is measured. If the Hill-Sachs interval is greater than the remaining glenoid track, the lesion is considered “off-track,” and they recommend a remplissage in addition to an arthroscopic Bankart repair. However, this elegant method has to be clinically confirmed and factors like ligament status (HAGL lesions, laxity, and translation that render all Hill-Sachs lesions engaging) or ability to obtain intraoperatively reliable measures are not taken into account in the evaluation.
In the setting of glenoid bone loss ≥25 % of the glenoid diameter, an arthroscopic Bankart repair has an unacceptably high rate of recurrence. Burkhart and DeBeer reported a 4 % recurrence rate for arthroscopic Bankart repair when glenoid bone loss was <25 %. However, with glenoid bone loss ≥25 %, the recurrence rate was 67 % with an arthroscopic approach [25]. They subsequently recommended a Latarjet procedure in the population with substantial glenoid bone loss. In 1954, Latarjet reported a coracoid transfer procedure in which the inferior aspect of the coracoid was secured to the anterior glenoid. The excellent stability of this procedure is obtained by a triple effect first proposed by Patte and Debeyre [80]: (1) the sling effect of the conjoint tendon when the arm is abducted and externally rotated, (2) the “bony effect” that increases or restore the glenoid anteroposterior diameter, and (3) the retensioning of inferior capsule to the stump of coracoacromial ligament, rendering the coracoid extra-articular. The Latarjet procedure is associated with a very low recurrence rate even in the setting of substantial glenoid bone loss and has become the gold standard of treatment in such settings. In addition, this nonanatomic method of anterior glenohumeral stabilization has progressively expanded and is actually the primary technique of choice for many European surgeons, as it prevents recurrent anterior instability in approximately 95–99 % of cases [81, 82]. This procedure is also favored by some as a first choice in many contact athletes [83]. While traditionally an open procedure, the technique can now be performed arthroscopically [10, 11, 84, 85]. To date, however, there is actually no proven benefit of an arthroscopic approach to the procedure, and the risk of complication remains high with a large learning curve [86].
Finally, some authors have recommended autogenous iliac crest or tibial allograft as a means of restoring glenoid bone loss. However, it has been demonstrated that the most important effect of the Latarjet is provided by the conjoint tendon at both the end-range and the mid-range arm positions [87]. We therefore believe that the indication for iliac crest or tibial grafting should be limited to revision procedures such as following a failed Latarjet reconstruction.
17.6 Author’s Preferred Treatment
Treatment is based on patient factors and associated pathology as previously discussed. In general, for patients under the age of 30, we offer a primary stabilization following a first traumatic anterior instability episode. Such patients are counseled on the natural history or anterior instability and the potential for subsequent injury. For the majority of patients over the age of 30, nonoperative treatment is advised with standard sling immobilization for 3 weeks followed by progressive strengthening and return to activities. For such patients with persistent weakness or recurrent instability, an MRI or MRI arthrogram is obtained to evaluate for an associated rotator cuff tear, and stabilization is performed.
In most cases of glenoid bone loss <25 % (based on preoperative imaging), we perform an arthroscopic Bankart repair using anterior and posterior working portals while viewing from an anterosuperolateral portal and base our repair on the extent of the pathology usually using two to four anchors. We have recently adopted the proposal of DiGiacomo et al. for intraoperatively determining the need for remplissage [27], but as previously noted, the outcomes of this algorithm are not clearly defined.
In the setting of glenoid bone loss ≥25 % of the glenoid diameter, we perform a Latarjet reconstruction [83]. One of us (AL) has experience with an arthroscopic Latarjet and utilizes this technique frequently. We believe that the arthroscopic Latarjet, after modifications, will be safer and thus a reliable technique but cannot at the current time recommend this for widespread use given the complexity of the procedure and high learning curve.
On the basis of the aforementioned elements, we use a treatment paradigm for all patients with anterior instability (Fig. 17.10). However, if one feels that risk for recurrence is high despite the lack of substantial glenoid bone loss (e.g., young male contact athlete), we do not hesitate to recommend Latarjet reconstruction.
Fig. 17.10




Treatment paradigm proposed by the authors for patients with anterior instability
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








