Fig. 20.1
Jerk test: (a) With the patient seated, the examiner stabilizes the shoulder girdle by grasping the scapular spine and clavicle with one hand. The other hand holds the patient’s flexed elbow and with the arm in 90° of abduction and internal rotation. (b) The arm is then moved horizontally across the chest while applying an axial load through the elbow. A sudden clunk or “jerk” often associated with pain occurs in a positive test as the humeral head subluxates posteriorly over the glenoid rim. Maintaining this load, the arm is moved back to its starting position, and a second jerk may be appreciated as the humeral head relocates back into the glenoid fossa
Fig. 20.2
Posterior stress test: With the patient in the seated position, the examiner immobilizes the shoulder by grasping the scapular spine and clavicle with one hand. The other hand is used to apply a posterior force to the arm held in 90° of forward flexion, adduction, and internal rotation. A positive test is determined when subluxation combined with pain/apprehension is present
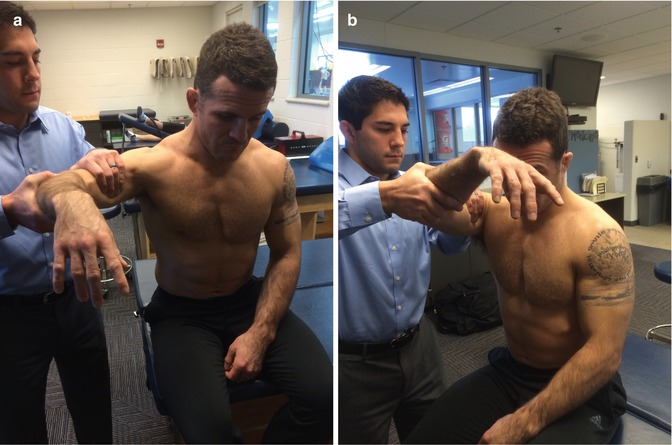
Fig. 20.3
Kim test: (a) The patient is seated and the arm is positioned in 90° of abduction. (b) The arm is then passively elevated an additional 45° while the examiner applies an axial load through the elbow and a downward and posteriorly directed load through the proximal arm. Posterior subluxation with pain signifies a positive test

Fig. 20.4
Posterior load and shift test (or posterior drawer test): With the patient in the supine position, the shoulder girdle is stabilized with one hand, while the other hand holds the proximal arm and loads the humeral head medially into the center of the glenoid to confirm neutral joint position. A posterior stress is then applied to the arm to evaluate excessive posterior translation
20.4 Essential Radiology
Athletes presenting with shoulder pain and instability should be sent for a 3-view radiographic series to include an anterior-posterior view, axillary (or West Point) view, and supraspinatus outlet (or apical oblique) view. Radiographs are frequently normal; however, this combination of views is necessary to accurately assess the athlete’s shoulder for bony pathology including reverse Hill-Sachs lesions (Fig. 20.5), reverse bony Bankart avulsions (Fig. 20.6), glenoid rim abnormalities, glenoid dysplasia, or lesser tuberosity fractures that are often considered pathognomonic for previous posterior shoulder dislocations. Some studies have described stress radiography, where posterior loads are applied to the shoulder to assess posterior translation, but this is not typically performed.

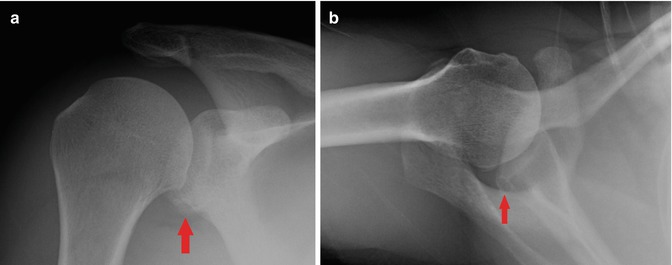

Fig. 20.5
Radiograph demonstrating large reverse Hill-Sachs lesion
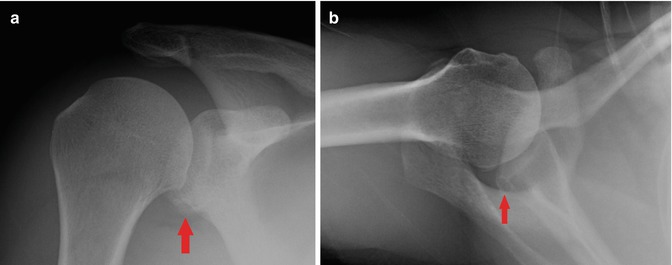
Fig. 20.6
AP (a) and Axillary (b) radiographs of the glenohumeral joint demonstrating a reverse bony Bankart lesion (red arrows)
Although plain radiographs are a good starting point and may be helpful to rule out any obvious bony defects, they are frequently negative, and magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) provided much more useful information regarding the integrity of soft tissue structures that are more typically involved in the pathogenesis. Specifically, MRI provides visualization of posterior capsulolabral structures, biceps anchor, rotator cuff, and the rotator interval (Fig. 20.7). An MRA is helpful in detecting a Kim lesion, or a marginal labral tear, that may be missed with standard MRI.
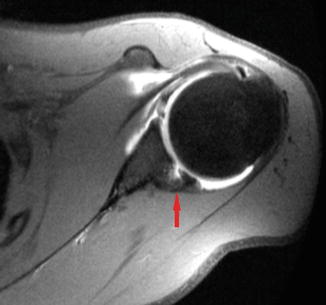
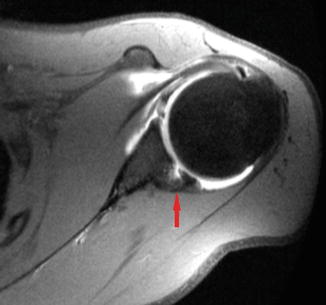
Fig. 20.7
MRI demonstrating a reverse Bankart lesion (arrow)
If a bony abnormality is suspected based on plain films, computer tomography (CT) may be utilized to better evaluate the defect. CT is the best imaging modality available for evaluating the size of reverse Hill-Sachs lesions or glenoid pathology as it allows the surgeon to determine what percentage of the humeral or glenoid articular cartilage is involved.
Dynamic ultrasound is another modality that has been described in the literature as a fast and inexpensive tool to objectively quantify glenohumeral laxity; however, it is not commonly used in the clinical setting due to the difficulty involved in interpreting the ultrasound imaging by most orthopedic surgeons [15].
20.5 Treatment Options
An initial course of conservative management involving at least 6 months of activity modification (or rest) with physical therapy focused on strengthening the dynamic muscular stabilizers is generally recommended, although high-profile athletes are often treated more aggressively to limit time away from competition. Currently, there is no clear evidence in the literature supporting the use of bracing or taping to help stabilize the shoulder. Conservative treatment has been shown to have successful outcomes in certain patients with posterior instability [2, 5, 16, 17]. In particular, athletes who have developed posterior instability from repetitive microtrauma as opposed to a single macrotraumatic event generally tend to do better with conservative management. Burkhead and Rockwood demonstrated success rates of approximately 80 % in patients with a history of atraumatic instability, compared to a success rate of just 16 % in patients who experienced posterior instability after a traumatic event [17].
Surgical management is generally considered after conservative management has failed but can usually be delayed until the off-season. Surgical techniques can be grouped into two broad categories: correction of soft tissue defects (more common) and correction of bony defects. Of course, some athletes may require correction of both soft tissue and osseous problems. Procedures involving correction of bony pathology are more commonly performed open, whereas procedures requiring soft tissue repair are generally performed arthroscopically. However, recent literature has also described arthroscopic techniques for treatment of bony defects including reverse Hill-Sachs lesions [18].
The most common soft tissue pathology associated with posterior instability is posterior capsular attenuation/redundancy with or without a reverse Bankart tear. These lesions routinely occur together. The redundancy of the posterior capsule is typically corrected arthroscopically via a vertical posterior capsular shift (i.e., capsular plication), and concomitant reverse Bankart lesions are corrected arthroscopically with suture anchors or tack fixation. Savoie et al. looked at arthroscopic management of posterior shoulder instability and found isolated reverse Bankart lesions present in 51 % of the shoulders, a stretched posterior capsule in 67 % of shoulders, and a combination of the two problems in 16 % of all shoulders [19]. They also reported the presence of several other accompanying lesions including anterior-superior labral tears and SLAP tears (20 %), superior glenohumeral ligament injury (7 %), rotator interval damage (61 %), middle glenohumeral ligament injury (38 %), anterior glenohumeral ligament injury (27 %), and an enlarged axillary pouch (20 %).
Although bony lesions including reverse Hill-Sachs and posterior glenoid defects are less common and are generally associated with macrotraumatic events or frank posterior dislocations, it is worth mentioning the commonly described treatment options for these problems. Surgical treatment is generally indicated in patients with reverse Hill-Sachs lesions involving more than 25–30 % of the humeral articular surface [20]. Both anatomic as well as nonanatomic techniques have been described to correct problems of instability caused by large reverse Hill-Sachs defects. The original McLaughlin procedure requires transfer of the subscapularis tendon into the humeral head defect, thereby preventing the edge of the defect from dislocating and locking behind the posterior glenoid [21]. The Neer modification of the McLaughlin procedure involves transferring the subscapularis tendon along with an osteotomized lesser tuberosity [22]. This modification can be very helpful when an associated lesser tuberosity fracture is present with a reverse Hill-Sachs lesion.
Anatomic reconstruction of a reverse Hill-Sachs lesion can be accomplished by filling the defect with bone graft. The decision to use autograft versus allograft is determined preoperatively depending on the size of the defect. For small reverse Hill-Sachs lesions where approximately 25 % or less of the articular surface is involved, autograft is generally recommended; however, osteochondral allograft is more commonly used for larger defects involving greater than 25 % of the surface [22]. Specifically, we recommend performing humeral head osteoarticular allograft transplantation for these larger defects [23, 24].
Posterior instability resulting from posterior glenoid deficiencies may be corrected using either a posterior iliac bone block or by performing a posterior glenoid opening wedge osteotomy. In addition, Skendzel and Sekiya described a novel technique of arthroscopic glenoid reconstruction using glenoid osteochondral allograft [25]. These posterior glenoplasty procedures are generally indicated in patients with osseous defects as their primary cause of instability; however, they may also be performed in patients who have failed previous posterior capsulorrhaphy.
20.6 Author’s Preferred Treatment
We recommend that patients undergo physical examination under anesthesia prior to beginning surgery. The patient should be positioning in the lateral decubitus position with the affected shoulder facing superiorly and the table in a slight reverse Trendelenburg position. The placement of an axillary role under the adducted operative arm can help to better visualize the glenohumeral joint.
We prefer the use of both an anterior and posterior portals providing improved visualization of the posterior labrum and glenoid for precise placement of capsular plication sutures. Bony landmarks should be marked prior to posterior portal placement 1–2 cm distal and medial to the posterolateral edge of the acromion. The anterior portal should be created at a level just superior to the subscapularis and lateral to the coracoid, at a 5 o’clock position. A diagnostic arthroscopy should be performed prior to repair to determine if there is any preoperatively unrecognized pathology contributing to the instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








