Fig. 9.1
Hara test scoring sheet
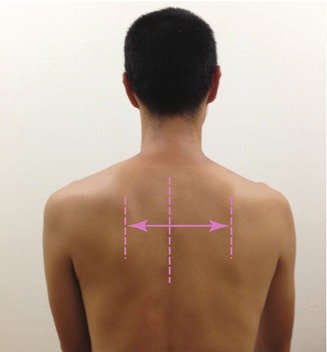
Fig. 9.2
In the scapula–spine distance test, the distance from the medial edge of the scapular spine to the spinous process of the thoracic spine is measured with the arms at the sides. The reference point on the thoracic spine is defined as the nearest spinous process. A difference of more than 1.0 cm between the left and right sides is considered abnormal

Fig. 9.3
Elbow extension test for assessment of scapular stability. The elbow extension test is performed with the shoulders in 90° of forward flexion. The subject extends the elbow joint from 90° of flexion with maximum force while the examiner holds the subject’s forearm to resist his extension force. The test is considered abnormal when the muscle strength on the dominant side is less than that on the nondominant side

Fig. 9.4
Elbow push test for assessment of scapular stability. The elbow push test is performed with the shoulders in 90° of forward flexion. While grasping the contralateral elbow with each hand, the subject pushes each elbow in turn anteriorly with maximum force. The examiner resists this pushing by holding the elbow. The test is considered to be abnormal when the muscle strength on the dominant side is less than that on the nondominant side

Fig. 9.5
Combined abduction test for assessment of posterior shoulder tightness. The examiner completely prevents any movement of the scapula by holding it. The humerus is passively abducted in the coronal plane. This test is considered abnormal when the upper arm fails to touch the head during glenohumeral abduction with a fixed scapula. Left: intact; right: abnormal
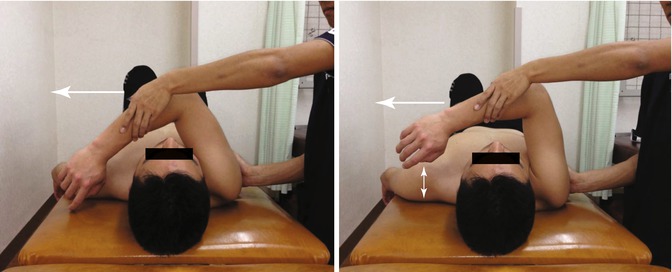
Fig. 9.6
Horizontal flexion test for assessment of posterior shoulder tightness. The examiner completely prevents any movement of the scapula by holding it and horizontally flexes the humerus. This test is considered to be abnormal when, during shoulder horizontal flexion with a fixed scapula, the subject is unable to reach around the other shoulder to touch the bed. Left: intact; right: abnormal

Fig. 9.7
The hyper-external rotation test, which evaluates peel back of the superior labrum and pathological internal impingement, is performed in 90° of shoulder abduction with the elbow flexed at 90° in the supine position. The test is considered abnormal when the subject feels pain as the examiner applies external rotation torque beyond the maximum external rotation position
The scapula–spine distance, elbow extension test, elbow push test, subacromial impingement tests, and manual muscle tests of shoulder abduction, external rotation, and internal rotation are assessed while the subject is sitting. Patients are supine for the combined abduction test, horizontal flexion test, capsular laxity tests, and hyper-external rotation test.
In the scapula–spine distance test, the distance from the medial edge of the scapular spine to the spinous process of the thoracic spine is measured with the arms at the sides (Fig. 9.2). The reference point on the thoracic spine is defined as the nearest spinous process. A difference of more than 1.0 cm between the left and right sides is considered abnormal. To assess the scapular stabilizers, the elbow extension test and elbow push test are performed with the shoulders in 90° of forward flexion (Figs. 9.3 and 9.4). For the elbow extension test, the subject extends the elbow joint from 90° of flexion by using maximum force, while the examiner holds the subject’s forearm to resist his extension force (Fig. 9.3). For the elbow push test, while grabbing the contralateral elbow with each hand, the subject pushes each elbow in turn anteriorly with maximum force as the examiner resists his pushing by holding the elbow (Fig. 9.4). Muscle strength is evaluated by manual muscle testing on a scale of 0–5. We assess the muscle strength of shoulder abduction with the subject’s thumb up; this is known as the “full can position” [20, 25]. We measure external rotation strength with the subject’s arm at his side [9]. To assess internal rotation strength, we record the subject’s strength in lifting his hand off his back [12]. We consider the results of the elbow extension test, elbow push test, and manual muscle tests of abduction, external rotation, and internal rotation to be abnormal when the muscle strength on the dominant side is less than that on the nondominant side. To assess the posterior tightness of the shoulder joint, subjects perform the combined abduction test and horizontal flexion test while the examiner fix the scapula and prevent it from moving by holding it. The humerus is passively abducted in the coronal plane for the combined abduction test (Fig. 9.5) and horizontally flexed for the horizontal flexion test (Fig. 9.6). If the subject’s upper arm fails to touch his head during glenohumeral abduction with a fixed scapula, the combined abduction test is graded as abnormal. The horizontal flexion test is considered abnormal when the subject is unable to reach around the other shoulder to touch the bed during horizontal flexion with a fixed scapula. Capsular laxity is evaluated by load-and-shift testing in the anterior, posterior, and inferior directions; anterior apprehension and relocation tests are also done. When the dominant side shows increased laxity or when the subject feels that the shoulder is unstable during any test, capsular laxity is considered abnormal. To evaluate subacromial impingement, we perform the Neer [31], Hawkins [14], and Yocum tests [24]. If the subject feels shoulder pain during any of these tests, subacromial impingement testing is graded as abnormal. The hyper-external rotation test (Fig. 9.7), which evaluates peel back of the superior labrum [4, 27, 28] and pathologic internal impingement [18, 26, 47], is performed in 90° of shoulder abduction with the elbow flexed at 90° in the supine position. The test is considered to be abnormal when a subject feels pain as the examiner applied external rotation torque beyond the maximum external rotation position. The number of “intact” results among the 11 physical examinations is recorded as the total Hara test score for each subject. The maximum total score (11 points) represents all “intact” results (i.e., no abnormality found) for all tests; subjects with lower scores are considered likely to have a problem in the upper-extremity kinetic chain.
9.4 Essential Radiology
We prefer to use magnetic resonance arthrography to evaluate capsular laxity and labral injuries, as well as articular-sided partial-thickness rotator cuff tears (Fig. 9.8). Stress x-rays are also useful for assessing shoulder laxity. Bony deformities or defects in the glenoid or humeral head can be assessed accurately by using three-dimensional computed tomography.


Fig. 9.8
Magnetic resonance arthrography of partial-thickness articular-sided rotator cuff tear (black arrow) and SLAP lesion (white arrow)
9.5 Disease-Specific Clinical and Arthroscopic Pathology
The main clinical symptom of articular-sided partial-thickness rotator cuff tears in throwing athletes is shoulder pain during sport. The shoulder pain is related to scapular dyskinesis, muscle imbalance (including imbalance of the rotator cuff muscles), posterior capsule tightness, and excessive anterior capsular laxity, as well as to the rotator cuff tear itself. In most patients with articular-sided partial-thickness rotator cuff tears (Fig. 9.9), a middle glenohumeral ligament tear (Fig. 9.10) or elongation and tearing of the anterior inferior glenohumeral ligament (Fig. 9.11) as well as a SLAP (superior labral tear from anterior to posterior) lesion (Fig. 9.12) and a thickened posterior capsule can be found during arthroscopy.
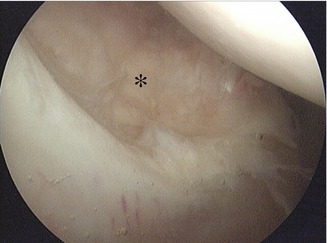
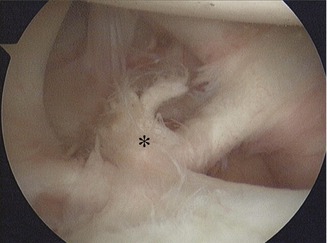
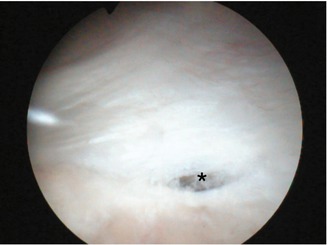

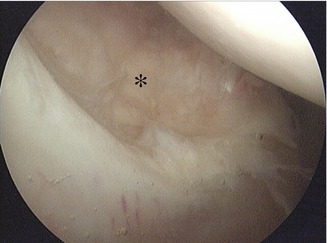
Fig. 9.9
Arthroscopic findings in partial-thickness articular-sided rotator cuff tear (*)
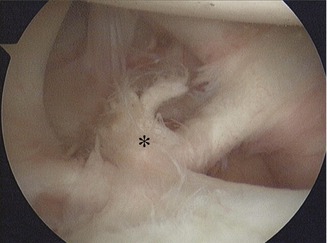
Fig. 9.10
Arthroscopic findings in middle glenohumeral ligament tear (*)
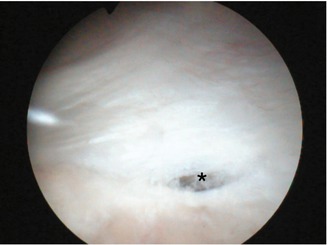
Fig. 9.11
Arthroscopic findings in tear and elongation of the anterior band of the inferior glenohumeral ligament (*)

Fig. 9.12
Arthroscopic findings in a type II SLAP lesion (*)
9.6 Treatment Options
Physical therapy is effective in most throwing athletes with articular-sided partial-thickness rotator cuff tears. When the scapular dyskinesis, muscle imbalance, posterior tightness, and increased anterior laxity are ameliorated with physical therapy, shoulder pain during throwing decreases or disappears in most cases. If physical therapy fails, surgical treatment typically is indicated. Various approaches, including debridement of partial-thickness tears with or without acromioplasty [3, 8, 21, 35, 38, 41], trans-tendon repair [6, 11, 15, 22, 39, 42, 46], or conversion to a full-thickness tear followed by repair [10, 11, 19, 37, 39], have been reported.
9.6.1 Debridement with or Without Acromioplasty
The superior shoulder capsule and undersurface of the supraspinatus and infraspinatus tendon insertions are evaluated for degenerative changes and debrided with a shaver until normal tendon is reached. Anterior acromioplasty and release of the coracoacromial ligament with debridement may be added. In patients with pathological shoulder laxity, which can cause shoulder symptoms, debridement alone is not a good option because it does not change shoulder laxity. However, for some throwing athletes who have no symptoms of pain associated with their pathological shoulder laxity or instability, debridement is a good surgical treatment and carries a low risk of postoperative shoulder stiffness.
9.6.2 Trans-tendon Repair
Snyder [40] proposed the use of an arthroscopic trans-tendon technique to treat partial-thickness articular-sided rotator cuff tears with the intention of restoring the medial footprint but preserving the tendon fibers remaining on the bursal side. Biomechanical studies have shown that trans-tendon repair results in higher footprint contact pressure and higher ultimate failure load compared with completion of the tear followed by repair [36]. Nevertheless, most clinical studies show that arthroscopic trans-tendon repair has a good outcome in terms of pain relief and shoulder score [6, 11, 15, 39, 42, 46].
9.6.2.1 Operative Technique
The frayed parts of the torn tendon are removed to expose good-quality tendon tissue. The footprint of the greater tuberosity is debrided to bleeding bone. A subacromial bursectomy is then performed to expose the bursal side of the torn tendon. The arthroscope is returned to the glenohumeral joint through the posterior portal, and a working portal is made anteriorly through the rotator interval. A spinal needle is passed percutaneously through the partial-thickness rotator cuff tear to identify the location for anchor insertion. One or two 4.5-mm suture anchors are then passed through the partial-thickness rotator cuff tear and screwed into the greater tuberosity under visualization from the glenohumeral joint. (In case of a longitudinal tear, a side-to-side suture repair is performed without using any suture anchor.) One suture limb is retrieved through the anterior portal. A 16-gauge spinal needle is passed through the anterolateral portal 5 mm medial to the intact margin of the torn rotator cuff tendon to guide the suture limb and one suture limb from the anterior portal pulled through the intact healthy portion of the rotator cuff. The other limb is passed through 5–10 mm posterior to the first suture limb in the same fashion to make a mattress stitch. The suture limbs are tied by using a non-sliding rotator cuff knot [29]. If a second anchor is used, its sutures are passed through and tied in the same fashion.
9.6.3 Conversion to Full-Thickness Tear Followed by Repair
Clinical studies have shown that repair of articular-sided partial-thickness rotator cuff tears after tear completion has a good outcome. Itoi and Tabata investigated the clinical results of 38 shoulders in 36 patients with incomplete rotator cuff tears that were repaired after tear completion [17]. The overall results were satisfactory in 31 shoulders (82 %). Deutsch prospectively evaluated the clinical outcomes in 41 patients who underwent arthroscopic repair after completion of partial-thickness supraspinatus tears [10]. Significant improvements were demonstrated in terms of American Shoulder and Elbow Surgeons scores, pain relief, and satisfaction. Forty patients (98 %) were satisfied with their outcomes. Kamath et al. also reported a high rate of patient satisfaction with arthroscopic repair after conversion to full-thickness tears [19]. Thirty-seven of 42 shoulders (88 %) had intact rotator cuffs (as seen on postoperative ultrasound), with improved American Shoulder and Elbow Surgeons scores and a 93 % patient satisfaction rate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








