Tibia and fibula diaphyseal fractures
Management of insufficiency fractures
Management of periprosthetic fractures
INTRODUCTION
Many fractures are increasing in incidence because of an expanding population and a higher proportion of elderly people in the population. This, however, is not true of fractures of the tibia and fibula. In 2000 Court-Brown and Caesar1 recorded that tibial diaphyseal fractures accounted for 1.9% of all adult fractures in a defined population in the United Kingdom. However, between 2010 and 2011 tibial fractures only accounted for 1% of fractures in the same population.2
The relatively rapid decline in the prevalence of tibial fractures together with an increased interest in fragility fractures, such as those of the proximal femur, proximal humerus and distal radius, has meant that the literature dealing with tibial fractures in the elderly is somewhat deficient. There are virtually no papers discussing the management of tibial fractures in the elderly, and to allow us to write this chapter we have used data from three databases constructed over a 13–15-year period in Edinburgh, Scotland. The first is a consecutive series of 187 tibial fractures, in patients aged ≥65 years, collected over a 13-year period. This database has been used to establish the type of fracture presenting to surgeons and their reasons for the choice of treatment method. The second database was one of 233 patients used by Clement et al.3 to identify the complications of tibial fractures in the elderly and the reasons for their occurrence, and the third database consisted of 484 consecutive open fractures in the elderly, collected over a 15-year period,4 from which we were able to study the characteristics of open tibial fractures in the elderly. During this 15-year period there were 48 open tibial fractures in patients ≥65 years of age.
Tibial fractures have always interested orthopaedic surgeons. The older arguments promoting non-operative management have largely disappeared5 and most surgeons now use surgical management, usually intramedullary nailing.6,7 The high prevalence of open fractures and high energy fractures in the elderly means that treatment can be difficult and there is a relatively high complication rate. In this chapter we will analyse the epidemiology of tibial fractures in the elderly aged ≥65 years and the super-elderly aged ≥80 years. We will also analyse why surgeons choose particular treatment methods and how successful these methods are. In addition we will also present a brief section on fibular fractures in the elderly that are not associated with proximal tibial or ankle fractures.
EPIDEMIOLOGY
There is no doubt that fragility fractures such as proximal humeral fractures and distal radial fractures are increasing in incidence in elderly patients,2 but fractures of the tibial diaphysis are decreasing in incidence. A review of the tibial diaphyseal fractures treated in the Royal Infirmary of Edinburgh in 1991 showed that the incidence was 24.4/105/year. This fell to 13.5/105/year in 2010/2011. The incidence in males fell from 37.2/105/year to 20.1/105/year and in females it fell from 13.5/105/year to 7.3/105/year.2 This is shown in Figure 40.1.
One might expect the incidence in younger patients to fall because of improved industrial and workplace safety legislation and drink driving laws. However, a review of the incidence of tibial diaphyseal fractures in the ≥65-year-old group and ≥80-year-old group shows that the overall incidence of tibial diaphyseal fractures has declined. This is mainly seen in women (Figure 40.1). Figure 40.1 shows that the incidence in males is essentially unchanged, but this is not the case in women. In 1991 the incidence in ≥65-year-old women was 56.1/105/year. This declined to 27.5/105/year in 2000 and to 6/105/year in 2010/2011.2 The equivalent figures for the ≥80-year-old population were 97.9/105/year, 47.4/105/year and 13.5/105/year. In ≥80-year-old men there were no fractures in 1991 and the incidences in 2000 and 2010/2011 were very similar at 13.7/105/year and 10.5/105/year.2
The question arises as to why tibial diaphyseal fractures in the elderly are declining in incidence. Chapter 1 (Table 1.6) shows that tibial diaphyseal fractures in the elderly are usually caused by a standing fall or are high energy injuries caused by road traffic accidents. It shows that more tibial diaphyseal fractures are caused by high energy injuries than any other fracture in the elderly. This does not appear to have changed in the last 20 years. Analysis of tibial diaphyseal fractures in the elderly in 1991 shows that 34.5% were caused by road traffic accidents and that 90% of these were in pedestrians. A further 58.6% were caused by falls, which is similar to the 68.8% seen in 2010/2011.2 It would seem that while the incidence of tibial diaphyseal fractures in the elderly has reduced considerably, particularly in women, the prevalence of the two main causes of fractures has not changed very much. One might postulate that improved road safety measures have caused fewer elderly women to be struck by cars, but there would seem to be no good reason for the decline in fall related fractures when this is not the case in other fractures.
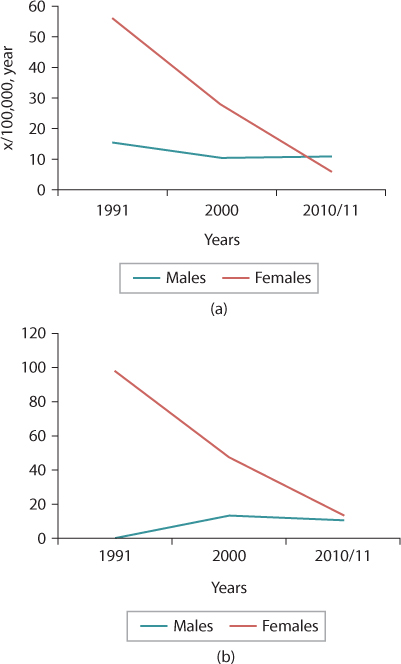
Figure 40.1 Incidence of tibial diaphyseal fractures over a 20-year period in patients aged ≥65 years (a) and ≥80 years (b).
However, increased frailty is obviously a factor as fracture incidence is greater in ≥80-year-old women than in ≥65-year-old women (Chapter 1 and Table 1.5). It should be remembered that tibial diaphyseal fractures are not fragility fractures1 and if an elderly person falls he or she is more likely to sustain a proximal femoral, proximal humeral or distal radial fracture. It may be that the falls that cause tibial diaphyseal fractures are somewhat different. There may be more energy involved in these falls, but we think it likely that the fall often involves a rotational force on the tibial diaphysis which causes the spiral fractures that are commonly seen in the elderly.
Open fractures
Open tibial fractures are very common in the elderly. Table 1.6 in Chapter 1 shows that in a recent 2-year study period 43.8% of the fractures in the ≥65-year-old group were open. One might expect that the open fractures would be caused by high energy injuries, but 36.4% of the fall related fractures were open, highlighting the problems associated with the poor quality soft tissues in the elderly and the subcutaneous location of the tibia. Tables 1.7 and 1.8 in Chapter 1 also show that the problems related to poor soft tissues are more common in women. In the 15-year analysis of open fractures, 48.6% of open tibial fractures in women aged ≥65 years were Gustilo8,9 type III in severity. Women aged ≥80 years had a similar prevalence of Gustilo type III fractures, but in men aged ≥65 years the prevalence of Gustilo type III fractures was only 7.7% and there were no Gustilo type III fractures in men aged ≥80 years. This suggests increasing male frailty, as presumably men ≥80 years of age are less active than women.
Tables 1.7 and 1.8 in Chapter 1 give the combined incidences of open fractures of the tibia and fibula, expressed as x/106/year, but analysis shows that of the 48 open fractures of the tibia and fibula treated in the 15-year period, 46 were open tibial fractures and two were isolated open fibular fractures.4 This indicates an incidence of open tibial fractures of 3.1/105/year in ≥65-year-old patients and 4.4/105/year in ≥80-year-old patients. The equivalent figures for open fibular fractures are 0.1/106/year and 0.2/106/ year, confirming their rarity.
Of the 48 patients who presented with an open tibial or fibular fracture, 25 (52.1%) were isolated injuries. In the remaining 23 (47.9%) patients the average Injury Severity Score (ISS) was 18 and altogether 8 (16.7%) had an ISS ≥16. All of these patients were pedestrians struck by a motor vehicle. Open fractures are discussed in Chapter 13.
Insufficiency fractures
Insufficiency fractures occur as a result of repetitive normal loading on abnormal bone that has decreased resistance. Obviously all osteopenic and osteoporotic fractures can be considered to be insufficiency fractures, but these fractures usually require a defined injury mechanism, this commonly being a fall. In a number of fractures in the elderly there is no causative mechanism and we have referred to these as insufficiency fractures. An analysis of the 187 consecutive elderly tibial fractures in patients ≥65 years of age showed that eight (4.3%) were insufficiency fractures. All of these fractures occurred in women and the average age was 72.5 years. The incidence of tibial insufficiency fractures in ≥65-year-old women was 1.1/105/year and in ≥80-year-old women it was 0.4/105/year. An example of a tibial insufficiency fracture is shown in Figure 40.2.
By far the most common site of insufficiency fractures in elderly patients is the thoracolumbar spine and studies have shown that 25–30% of post-menopausal women have insufficiency fractures.10,11 A study from France showed that pelvic and sacral insufficiency fractures are relatively common.12 The investigators also found that insufficiency fractures occurred in the tibia (Figure 40.2), femoral head, femoral neck and femoral diaphysis. A review of the location of the fractures in the tibia showed that the majority were transverse distal diaphyseal fractures, but the authors also reported a tibial plateau fracture, a proximal tibial diaphyseal fracture (Figure 40.2) and four longitudinal insufficiency fractures. A recent case report has shown that, like femoral insufficiency fractures, tibial insufficiency fractures can follow the use of bisphosphonate therapy.13
Metastatic fractures
Metastatic fractures of the tibia in the elderly population are rare and only two (1.1%) occurred in the 13-year study, giving an overall incidence of about 0.2/105/year in the ≥65-year-old group. One was caused by a metastasis from an adenocarcinoma and the other by a metastasis from a malignant melanoma. Metastatic fractures are discussed in detail in Chapter 16.
Periprosthetic fractures
In the study of 187 patients aged ≥65 years there were three periprosthetic tibial fractures (Figure 40.3) with an average age of 69.7 years. This indicates that the incidence of periprosthetic tibial fractures is about 0.2/105/year. The rarity of tibial periprosthetic fractures means that there is very little information about them in the literature. In a series of 102 fractures from the Mayo Clinic14 it was estimated that 0.4% of the knee arthroplasties undertaken in a 25-year period in the Mayo Clinic developed a periprosthetic tibial fracture. Periprosthetic fractures are discussed in Chapter 17.
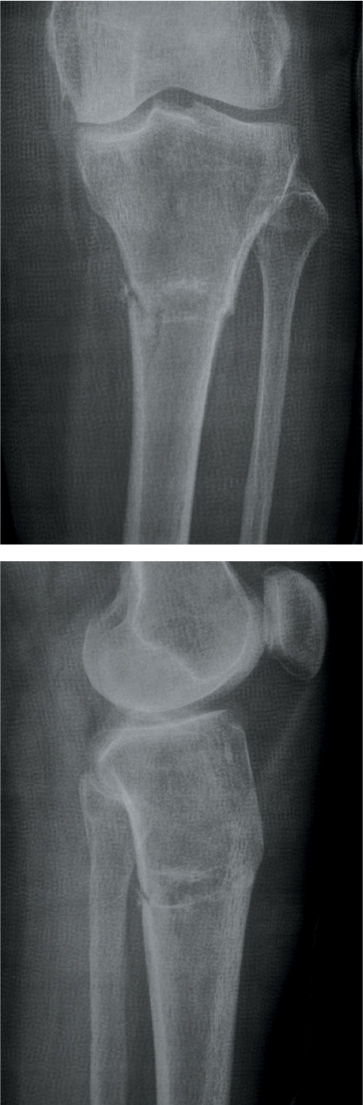
Figure 40.2 A proximal tibial diaphyseal insufficiency fracture.
CLASSIFICATION
The classification system most commonly used for tibial diaphyseal fractures is the AO/OTA15 system. The basic fracture types delineated by this classification system are shown in Figure 40.4. Type A fractures are simple fractures with A1 fractures being spiral fractures, A2 fractures being oblique fractures with an angle ≥30 degrees and A3 fractures being oblique fractures with an angle of <30 degrees. Type B fractures are wedge fractures with B1 fractures having a spiral wedge, B2 fractures a bending wedge and B3 fractures a fragmented wedge. Type C fractures are complex fractures with C1 fractures having a spiral morphology. C2 fractures are segmental fractures and C3 fractures are irregular, comminuted fractures. The suffix .X is used to define an associated fibular fracture in type A and B fractures. Thus .1 means that the fibula is intact, .2 means that the fibular fracture is not at the same level as the tibial fracture and .3 means that it is at the same level. In type C fractures the suffixes .1, .2, and .3 detail the amount of damage to the diaphysis.

Figure 40.3 A periprosthetic tibial diaphyseal fracture after a knee arthroplasty.
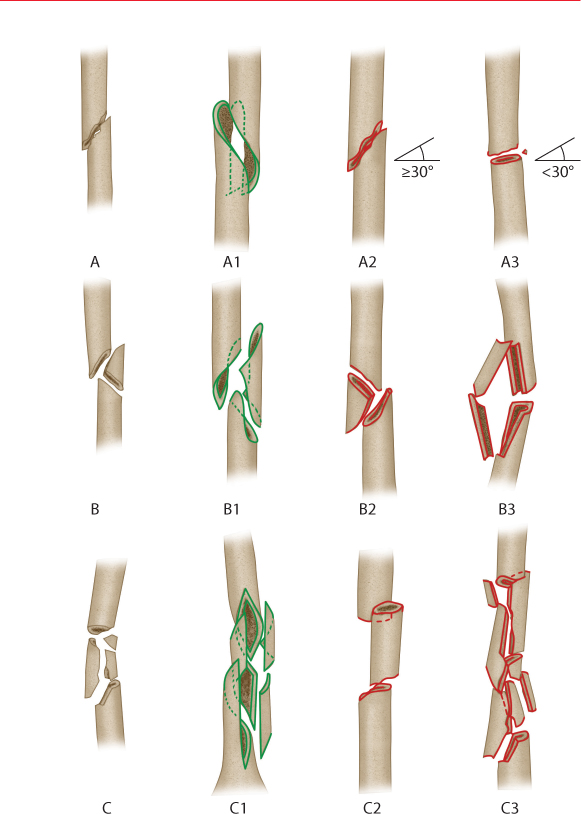
Figure 40.4 The AO/OTA classification of tibial diaphyseal fractures. (Redrawn from J Orthop Trauma 1996;10(Suppl):1–154.)
FRACTURE MORPHOLOGY
Analysis of the fracture morphology in the ≥65-year-old group shows that 64.4% were AO/OTA15 type A fractures, 15.6% were type B and 20% were type C fractures. The equivalent figures in the ≥80-year-old group were 58.8%, 11.8% and 29.4%. With increased aging and increased frailty the prevalence of more severe fractures increases. However, further analysis shows that 53.3% of tibial fractures have an A1 or B1 morphology and that 91.7% of these fractures followed a fall. This strongly suggests a rotational component to the force that causes a fall related tibial diaphyseal fracture.
TREATMENT
As with all tibial diaphyseal fractures, the treatment methods most commonly used by the majority of surgeons treating the elderly are non-operative management, intramedullary nailing, external fixation and plating. Occasionally a primary amputation may be undertaken.
In recent years most surgeons have moved from non-operative management of tibial diaphyseal fractures to operative treatment with intramedullary nailing being the preferred method for closed fractures6 and most open fractures.7 Plating has become less popular, particularly in the elderly, as in the past plates were associated with relatively high rates of implant failure, non-union and infection. Recently monoaxial and polyaxial locking plates have been introduced and many surgeons are now using minimally invasive plating techniques to try to minimize these complications. As yet there is no information about how useful monoaxial or polyaxial locking plating techniques are in elderly patients with tibial diaphyseal fractures.
To try to determine the reason for undertaking a particular treatment method in the elderly, we analysed the reasons for selection of the different treatment methods used in the 187 patients that have already been detailed. We found that 64.7% of the patients were treated with intramedullary nailing, 20.3% were treated non-operatively, 12.8% were treated with external fixation and 1.1% had a primary amputation. One patient (0.5%) was treated with a dynamic compression plate and one patient died prior to treatment.
Intramedullary nailing
Over the past 20–25 years intramedullary nailing has become the standard method of treating closed tibial fractures and most open fractures in adults.5,6 and 7 The results are better than achieved with other methods of treatment. We believe that it is the preferred technique for treating tibial diaphyseal fractures in the elderly. It is a relatively simple treatment that allows the patients to mobilize fully weight bearing, as they are able to do so. Clearly in elderly patients, it is very important to facilitate mobilization by allowing patients to weight bear as soon as possible.
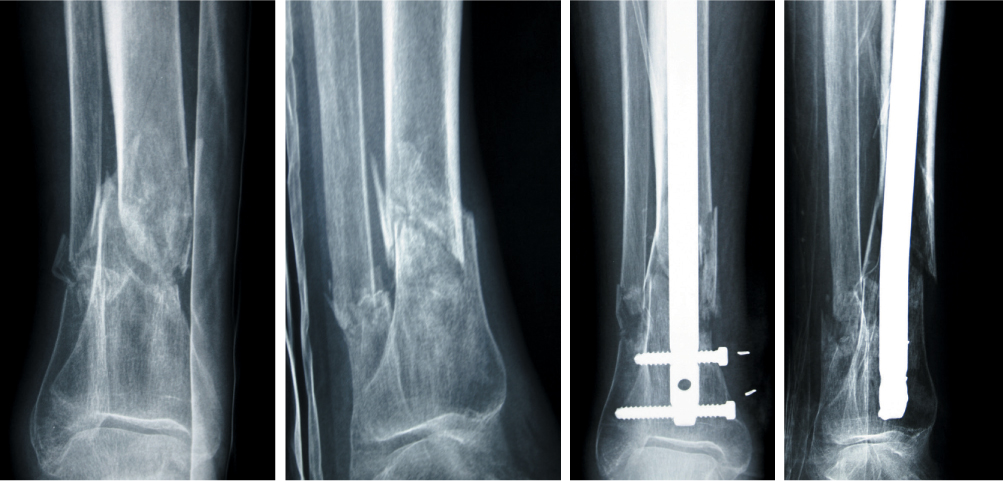
Figure 40.5 Intramedullary nailing of a tibial diaphyseal fracture in a 76-year-old woman.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








