Scapular fractures
Injury mechanism and associated injuries
Classification of scapular fractures
INTRODUCTION
Unlike most other fractures in the elderly, scapular fractures are not typically associated with osteoporosis. According to the reported data, scapular fractures account for only 3–5% of all injuries to the shoulder girdle and for about 1% of all fractures.1 The reason is that the scapula is well protected by a thick muscular envelope, is highly mobile and is located on the elastic chest wall. Scapular fractures result mostly from high-energy trauma and therefore are often found in younger patients.
EPIDEMIOLOGY
There are no detailed epidemiological studies of scapular fractures and the data indicating their proportion of the total number of fractures are almost 80 years out of date.1,2 Until now, most authors have used data on patient age, the male–female ratio and the distribution of types of fractures from older studies. However, a detailed analysis of those studies shows that they cannot be considered representative. Their main drawbacks are small numbers of patients and a questionable diagnosis of individual fracture patterns, based on radiographs without CT data.3 Therefore, the epidemiological data presented here are based on an analysis of our own group of 250 patients with scapular fractures.
The group comprised 199 men (80%) and 51 women (20%). The average age of the whole group was 45 years (range: 15–92 years), with the average age of men 43.5 years and that of women 52.4 years. CT examination was used in 204 patients and 100 patients underwent surgical fixation. When the whole cohort was subdivided into two subgroups of patients under and over the age of 60 years based on our experience in previous epidemiological studies, particularly of proximal femoral fractures,4 the basic characteristics of each subgroup changed. In the group of patients under 60 years of age, the male–female ratio was 84:16, while in the group of patients older than 60 years, it was 64:36 (Table 18.1).
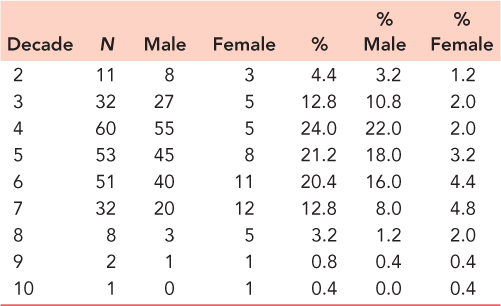
Patients older than 60 years accounted for 17% of the whole group. They constituted 12% of the men and up to 38% of the women in the whole group. The peak incidence of fractures in men was between the fourth and sixth decades, while in women it was between fifth and seventh decades (Table 18.2 and Figure 18.1).
Overall, 52% were fractures of the scapular body, 29% were fractures of the glenoid, 11% were fractures of the processes and 8% were fractures of the scapular neck. In patients older than 60 years, a slight increase was noted in the proportions of fractures of the glenoid and the processes, but no fracture of the scapular neck was recorded (Table 18.3). At the same time, the number of associated fractures of the proximal humerus was significantly higher, probably due to progressing osteoporosis.
Comparison of our groups of patients with a fracture of the scapula, the ankle, the distal radius, the proximal humerus or the proximal femur shows that the group with a scapular fracture had the lowest average age and the highest proportion of men versus women (Table 18.4). With advancing age, the proportion of women rose and, ultimately, in the eighth decade, exceeded that of men. For these reasons scapular fractures cannot logically be considered as osteoporotic injuries.
Table 18.1 Group of patients
Group of patients | All patients | Male (N) | Female (N) | Male:Female ratio |
|---|---|---|---|---|
Under 60 years | 204 | 171 | 33 | 84:16 |
Over 60 years | 46 | 28 | 18 | 64:36 |
All patients | 250 | 199 | 51 | 80:20 |
Table 18.2 Age distribution of scapular fractures
ANATOMY
The scapula is part of the shoulder girdle. It is attached to the axial skeleton by the clavicle via the acromioclavicular (AC) and sternoclavicular (SC) joints. This articulation chain maintains a constant distance between the scapula and the sternum. The scapula is located on the posterior chest wall between the second and seventh ribs and is held in this position by the tone of the attached muscles, mainly the upper part of the trapezius and the levator scapulae. The angle between the scapula and the frontal plane is approximately 30 degrees. The scapula is primarily responsible for providing efficient support to the humeral head in all positions of the arm. Smooth motion of the scapula over the chest wall is possible thanks to the gliding fibro-fatty tissue that fills the space between the muscles covering the anterior surface of the scapula and those of the chest wall.
Bone anatomy
The scapula is a flat triangular bone, defined by the superior, medial and lateral borders and three angles, including two flat angles: the superior and inferior angles, and the lateral angle, a three-dimensional structure formed by the scapular neck and the glenoid. On the posterior surface of the scapula, the division between the scapular body and neck is marked by the spinoglenoid notch. The anterosuperior surface of the scapular neck bears the origin of the coracoid process. The glenoid has a pear-shaped articular surface with a prominent ring of fibrocartilage at its wider end – the glenoid labrum. The anterior surface of the scapula is concave. The posterior surface of the scapula is divided by a bony ridge – the scapular spine – into the supra- and infraspinous fossae. In its lateral extent, the scapular spine becomes more elevated and ends in a robust bony process – the acromion – which is flattened and curves forward.
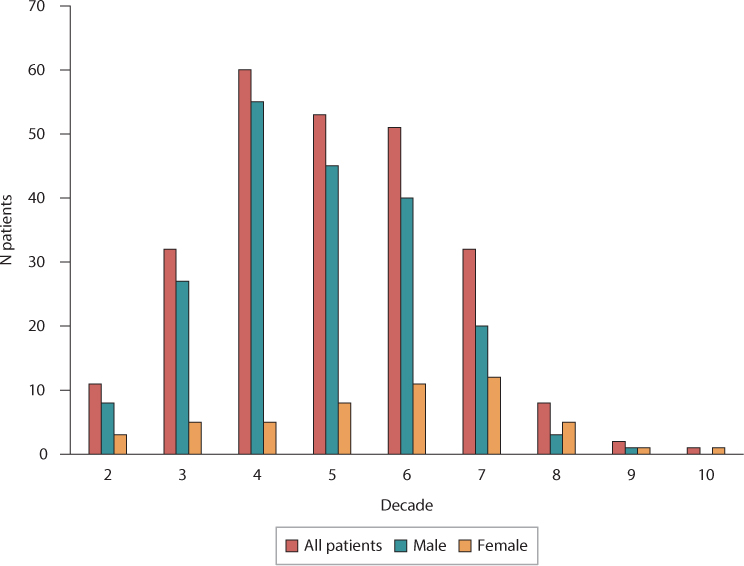
Figure 18.1 Age distribution of scapular fractures.
Table 18.3 Types of scapular fractures
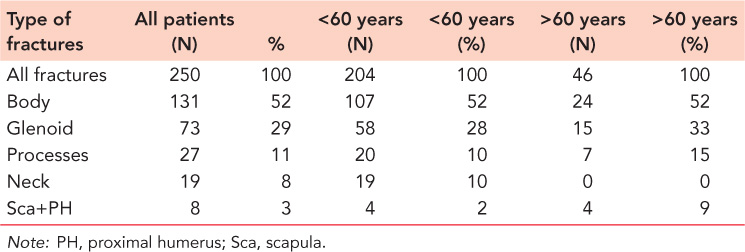
Table 18.4 Comparison of our groups of patients with a fracture of the scapula, the ankle, the distal radius, the proximal humerus or the proximal femur
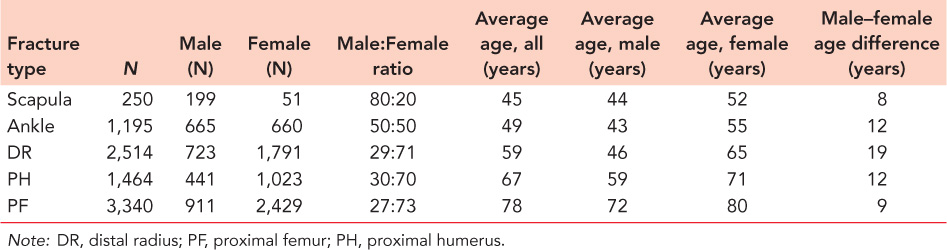
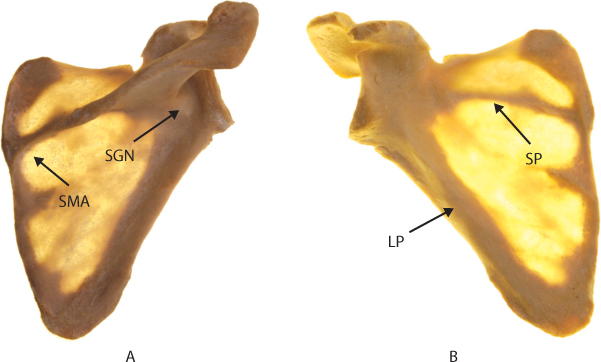
Figure 18.2 Anatomy of the scapula. (a) Anterior view, (b) posterior view. LP, lateral pillar; SGN, spino-glenoidal notch; SMA, spino-medial angle; SP, spinous pillar.
The distribution of the bony mass of the scapula is very uneven. When held up to the light, the scapula shows the highest concentration of bony mass in the glenoid, the scapular neck, including the base of the coracoid process, and the lateral border of the scapular spine. Cancellous bone is to be found only in the region of the lateral angle of the scapula.
Two bony pillars, which pass from the glenoid to the scapular body, transmit compression forces from the glenoid fossa. The lateral pillar is identical with the lateral border of the scapular body and connects the inferior border of the glenoid with the inferior angle. The spinal pillar arises from the central part of the glenoid and continues medially to become part of the base of the scapular spine. Its course can be seen better by viewing the scapula from the front against the light (Figure 18.2). The spinal pillar and the medial border of the scapular body form an open spino-medial angle. From the posterior view, it is evident that the two pillars and their connection via the markedly thinner medial border of the scapular body constitute the basic, triangular load-bearing structure of the scapular body. This triangle is effectively the biomechanical body of the scapula, as the superior angle and the adjacent part of the supraspinous fossa form merely an appendage, which serves as a surface for the insertion, or origin, of muscles, but does not transmit compressive forces from the glenoid. For this reason, it is necessary to distinguish between the anatomical and biomechanical bodies of the scapula.
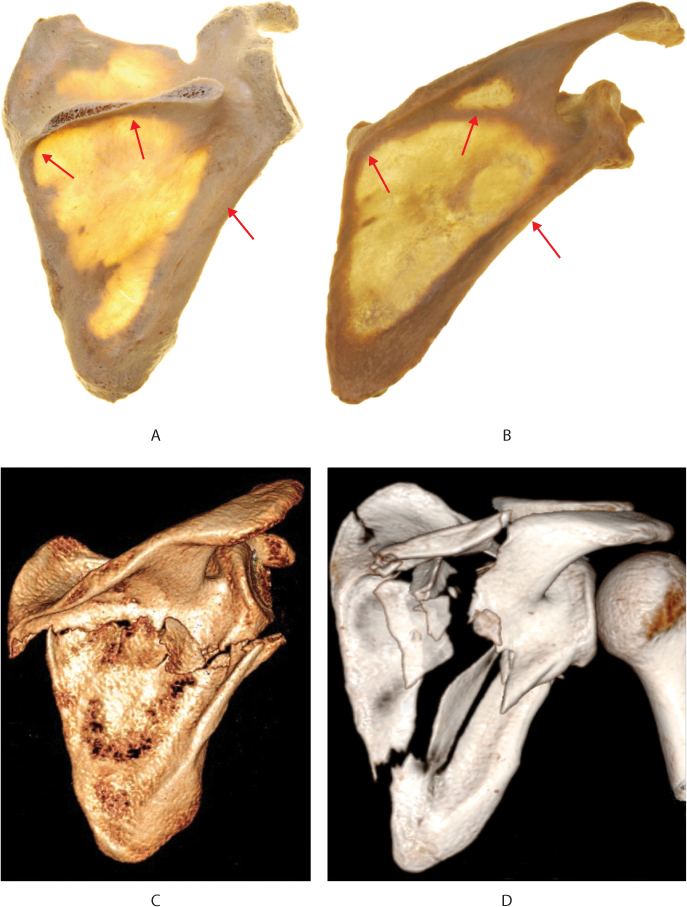
Figure 18.3 Critical zones of bony architecture of the scapula (red arrows). (a,b) Spino-medial angle, central scapular spine, lateral border, (c) two part fractures of the scapular (biomechanical) body, the fracture line passes from the lateral border into the spino-medial angle, (d) comminuted fracture of the scapular (anatomical) body, fracture lines pass through the lateral body, spino-medial angle and central scapular spine.
The weak areas of the scapula are mainly the central parts of the supra- and infraspinous fossae, where the bone is only a few millimetres thick. The weakest area of the circumference of the biomechanical body of the scapula is the spino-medial angle which is demonstrated by the fact that in the majority of scapular body fractures one of the main fracture lines passes through this region. Another area of weak bone is in the central part of the scapular spine where, quite often, fracture lines can also be seen, as shown by analysis of the course of fracture lines5 (Figure 18.3).
Muscles
The muscles of the scapula may be divided into two systems. The first, the scapulo-axial system connects the scapula with the axial skeleton, the spine and the chest wall in particular. This system is responsible for movement of the scapula over the chest wall. The other, the scapulo-brachial system, is formed by the muscles arising from the scapula and attaching to the bones of the free part of the upper limb, more specifically to the humerus, the proximal radius and the proximal ulna. Its role is to control movement between the scapula and the free part of the upper limb, that is, control of the motion in the glenohumeral joint and, to a small extent, the elbow.
In total, 18 muscles are attached to the scapula. Only three of them, namely the subscapularis, supraspinatus and infraspinatus, originate from the broad surface of the scapula in their respective fossae; the rest of them are attached to the borders of the scapula or its processes. Other muscles reinforce individual borders, angles and processes by their attachments, namely the levator scapulae at the superior angle, the rhomboid minor at the medial border at the level of the scapular spine posteriorly, the rhomboid major located directly inferior to it, and the latissimus dorsi at the inferior angle. From the same angle and partially from the lateral border of the scapula there originates the teres major and in the upper half of the lateral border, the teres minor. The serratus anterior inserts along the entire anterior length of the medial border of the scapula; the trapezius is attached to the scapular spine and the anterior rim of the acromion; the deltoid muscle arises from the distal border of the scapular spine and subsequently from the posterior rim of the acromion. The long head of biceps originates above the superior rim and the long head of triceps from below the inferior rim of the glenoid. Attached to the central part of the coracoid process is the pectoralis minor and from the apex of the coracoid there arise the coracobrachialis and the short head of biceps.
Nerves and blood vessels
The suprascapular nerve passes under the superior transverse scapular ligament, and travels together with the suprascapular artery and vein along the supraspinous fossa. This neurovascular bundle runs under the inferior transverse scapular ligament and enters the spinoglenoid notch on the posterior surface of the scapular neck. The suprascapular nerve gives off motor branches to the supraspinatus and infraspinatus muscles. The suprascapular artery anastomoses with the scapular circumflex artery on the lateral border of the scapula, about 2–3 cm distal to the glenoid.
INJURY MECHANISM AND ASSOCIATED INJURIES
By virtue of its thick muscular envelope, its considerable mobility and its location on the elastic chest wall, the scapula is well protected against injury. A majority of scapular fractures are reported to be caused by a high-energy mechanism, but this is not entirely true.6 From the viewpoint of the energy of the injury mechanism, the patients may be divided into three groups.
The first group comprises those with high-energy injuries, sustained mostly during a traffic accident, by a fall from height or by a heavy object falling onto the patient. They are found mostly in polytrauma patients with a range of injuries to individual organ systems, particularly to the chest (ribs, lungs), head, spine and abdomen. Injuries to the scapula are often discovered coincidentally, towards the end of the diagnostic and therapeutic process.
The second group comprises patients with medium-energy trauma caused usually by a fall from a bicycle or a slowly travelling motorcycle. The injury to the scapula and the shoulder girdle usually dominates, associated sometimes with cerebral contusion or another injury (e.g. tibial fracture).
The third group comprises mostly elderly patients who sustained a scapular fracture in a simple fall from standing height, down stairs or even as a result of a smaller object falling onto the scapula. In the majority of these patients it is an isolated injury to the shoulder girdle.
Scapular fractures are caused by exogenous and endogenous mechanisms. With the exogenous (external) mechanism, the impact acts directly on individual parts of the scapula, or is transmitted through the humeral head. In cases of direct impact, the scapula hits surrounding objects (e.g. when the chest hits the car body) or vice versa, when for instance a heavy object hits the scapula. The result is most often a fracture of the scapular body or scapular processes. In cases of transmitted forces, the impactor is the humeral head. The fracture pattern depends on the position of the arm at the time of injury. With the arm in abduction, the humeral head is driven against the inferior glenoid, which separates off, often together with a part of the lateral border of the scapula. With the arm in adduction, a blow on the elbow along the axis of the humeral shaft proximally dislocates the humeral head, which hits the acromion or the coracoid. Anterior or posterior dislocation of the humeral head may result in a fracture of the respective rim of the glenoid. The endogenous cause of scapular fractures is most frequently a violent muscle contracture as the result of an electrical injury or an epileptic seizure.
Pathological scapular fractures (e.g. bone cyst, osteodystrophy and tumour metastasis) are rare.6,7 Fatigue fractures of the scapular spine and the acromion have been reported in cases of insufficiency of the rotator cuff.8 A specific group are periprosthetic scapular fractures in patients following shoulder arthroplasty.
Our patients older than 60 years most often sustained a scapular fracture in a fall from standing height, on stairs or from a bicycle. We have recorded one fracture in a tumour metastasis. None of our patients older than 60 years was classified as a polytrauma patient.
DIAGNOSTICS
The diagnostic procedure in patients with scapular injuries depends on their general condition. In polytrauma patients, the priority is to save life. The treatment of a scapular fracture, even if detected during primary examination, may be postponed to a later time, except for an open scapular fracture. In a number of polytrauma patients, scapular fractures are often found coincidentally, for example, on a radiograph of lungs or a CT scan of chest.
Clinical examination
Patients in a less severe general condition, who are able to communicate, may undergo standard clinical examination. Scapular fractures are often associated with other injuries and, therefore, it is essential first to conduct a thorough and comprehensive examination of the patient before focusing on the shoulder. If one fracture of a shoulder girdle is found (e.g. of the clavicle), it is necessary to exclude other potential injuries.
PATIENT’S MEDICAL HISTORY
Knowledge of the exact mechanism of the injury and the patient’s subjective complaints are essential to a proper diagnosis. Elderly patients are asked about any past problems with the shoulder (rotator cuff lesion, osteoarthritis) or other systemic diseases (tumours, metabolic disease).
VISUAL ASSESSMENT
Careful examination of the shoulder and the entire chest, including the axilla, is performed. The shoulder may be deformed by a clavicular fracture, acromioclavicular dislocation, humeral head dislocation, by a markedly displaced scapular fracture or significant swelling. Examination of the integrity of the skin cover is important as a skin abrasion may indicate a site of impact.
PALPATION
A large part of the skeleton of the shoulder girdle may be examined by palpation, that is, the clavicle, sternoclavicular joint, acromioclavicular joint, the scapular spine and acromion, the tip of the coracoid and the humeral head; in the elderly who tend to be less muscular, the inferior angle and medial border of the scapula are also accessible. Palpation may reveal crepitus or pathological mobility. It is also important to palpate the axilla and the adjacent chest wall, and to identify the pulse of the axillary artery. As the fracture may be combined with a lesion of the brachial plexus, sensation in the upper limb should be examined to exclude an injury to the brachial plexus.
RANGE OF MOTION
Examination of the range of motion, mainly active motion, in scapular fractures is significantly limited by pain. If possible, passive motion in the glenohumeral joint is carefully examined.
PERIPHERY
It is also important to thoroughly assess other parts of the ipsilateral extremity including its peripheral innervation and vascularity in order to exclude associated injuries.
Imaging methods
Radiological examination is essential to the diagnosis of scapular fractures, the determination of the fracture patterns and the treatment procedure. Other imaging methods may include MRI and ultrasound scanning, although they are indicated only exceptionally and their contribution is limited.6,7,9 When scapular fractures occur in polytrauma patients or in the elderly, the radiodiagnostic algorithm described below has to be adjusted to the patient’s general condition.
RADIOLOGY
Part of the basic examination is a general radiograph of the entire shoulder girdle covering the whole scapula, the proximal humerus and the whole clavicle, including acromioclavicular and sternoclavicular joints. Scapular fractures are often associated with a clavicular fracture or acromioclavicular dislocation and, in the elderly, with a proximal humeral fracture. In cases with a suspected or detected scapula fracture, it should be combined with both Neer projections, if allowed by the patient’s general condition (Figure 18.4).
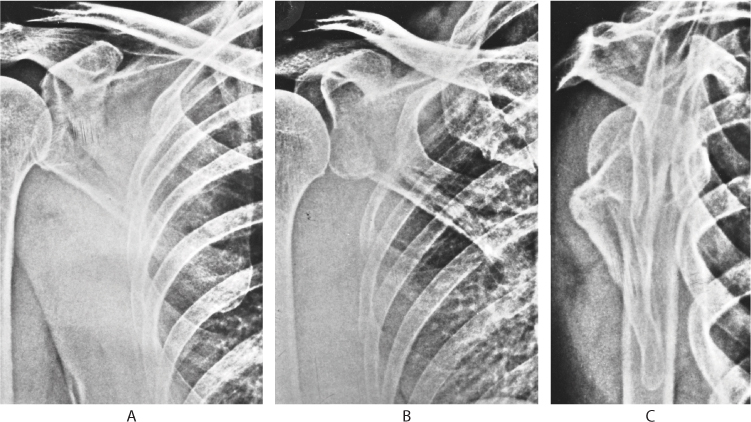
Figure 18.4 Radiological examination of scapular fractures. (a) Anteroposterior (AP) shoulder view, (b) Neer I view, (c) Neer II view.
Neer I projection, or the true anteroposterior radiograph of the scapula, is used to assess the glenohumeral joint space, displacement of the glenoid in relation to the lateral border of the scapula and to measure the glenopolar angle (GPA). In this projection, the scapular plane is parallel to the X-ray cassette. This may be achieved by rotating the patient with his/her back to the X-ray cassette by 30 degrees towards the affected side.
Neer II projection, also called Y-view, is a true lateral scapular projection. In this projection the scapular plane is perpendicular to the X-ray cassette. This may be achieved by rotating the patient, facing the X-ray cassette, by 60 degrees towards the affected side. The Y-view projection allows assessment of scapular body fractures in terms of translation, angulation and overlap of fragments, particularly of the lateral border. In addition, it displays clearly the relationships between the coracoid, the acromion and the lateral clavicle, as well as the acromioclavicular joint. It can be used to identify any avulsion of the anterior rim of the glenoid.
General radiograph of the chest, indicated to examine the lungs, heart and chest wall, in polytrauma patients often provides the first clue leading to a diagnosis of a scapular fracture. It is important mostly for assessment of the position of both scapulae in relation to the spine (scapulothoracic dissociation).
Other special projections, axillary in particular, are recommended by some authors as complementary views, to diagnose fractures of the glenoid, acromion and coracoid. However, axillary projection is, for most patients with a scapular or rib fracture, highly unpleasant and should not be used as a substitute for CT examination.
The complicated shape of the scapula and its position on the chest makes an unambiguous interpretation of findings and determination of the fracture pattern with the use of radiographic projections alone often very difficult or even impossible, For this reason, CT examination is very important.7,9
CT EXAMINATION
CT examination has fundamentally changed the radiodiagnostics of scapular fractures. It is always indicated when radiographic examination cannot reveal the exact fracture pattern, involvement of the articular surface or displacement of fragments.
CT transverse sections are valuable in the assessment of the condition of the glenoid fossa. They also help to detect undisplaced fractures of the scapular processes, especially those of the coracoid and the acromion. However, they do not provide a three-dimensional image of the fracture anatomy.
Two-dimensional CT reconstructions (2D CT), mainly in the sagittal plane, are used to assess the articular surface, especially in fractures of the base of the coracoid process involving the glenoid fossa.
Three-dimensional CT reconstructions (3D CT) are the only way to determine reliably the exact fracture pattern, particularly in fractures of the scapular body and neck, although they do not show fine fracture lines, especially in minimally displaced fragments. Reconstructions should be made in three basic views (Figure 18.5), with subtraction of ribs, clavicle and proximal humerus.10
The posterior view allows assessment of the course of fracture lines with regard to the scapular spine. It is important that it covers the entire infraspinous and also part of the supraspinous fossa.
The anterior view is essential in fractures of the scapular neck. This view helps to identify different courses of fracture lines in fractures of the anatomical and surgical necks of the scapula.
Glenoid fractures require a lateral view, always with subtraction of the humeral head. This is the only way to get exact information about the number of fragments and the course of fracture lines involving the glenoid. In fractures of the lateral border of the scapular body, this lateral view helps to assess its shortening, angulation and translation, or the shape and displacement of small intermediate fragments.
In certain fracture patterns it may be useful to obtain other views in order to assess the course of the fracture line, for example, a view of the supraspinous fossa, the spinoglenoid notch or a medial view.
CLASSIFICATION OF SCAPULAR FRACTURES
All classification systems published in the literature have one common drawback: they have been developed only on the basis of radiographs, often taken in a non-standard way.3,11,12 A number of fracture patterns previously proposed do not, in fact, correspond to the reality. In spite of this, they may persist in the newly developed classifications.13
Based on the analysis of our own group of 250 scapulae, with 3D CT reconstruction in 204 of them and 100 of them treated surgically, we have divided scapular fractures into five basic groups.7,14,15
Fractures of scapular processes
Fractures of scapular processes account for 11% of all scapular fractures in our group and for 15% of those in patients over 60 years of age (Table 18.3). They include fractures of the superior angle and the upper border of the scapula, fractures of and in the acromion and the scapular spine, and coracoid fractures. These fractures result from a direct blow to the upper part of the scapula, the pull of muscles and ligaments or impact by the displaced humeral head (Figure 18.6).
Fractures of the scapular body
Fractures of the scapular body account approximately for 52% of all scapular fractures in both the older and younger groups. We divide them into two basic groups, namely fractures of the biomechanical and of the anatomical bodies (Figure 18.7). The decisive criterion is the course of fracture lines in relation to the scapular spine.5,14
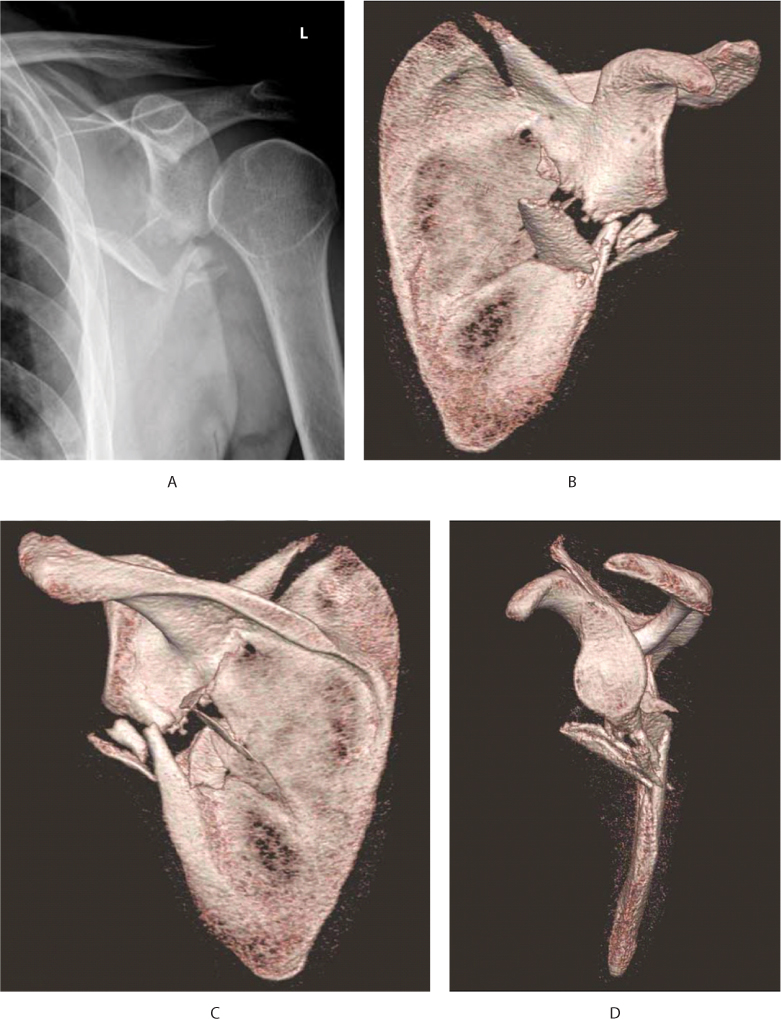
Figure 18.5 Standardized CT 3D views for scapular fractures: transspinous neck fracture. (a) Anteroposterior (AP) shoulder radiograph, (b) anterior 3D CT view, (c) posterior 3D CT view, (d) lateral 3D CT view.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








