Age-related changes in the elderly
Diversity of aging and functional decline
Principles of nutritional and fluid intake
Age as a risk factor for delirium
Metabolic changes (renal, liver, gut) and their impact on medication
Changes in bone metabolism – osteoporosis
INTRODUCTION
Changes associated with aging affect all organ systems and are associated with a decreased functional reserve capacity.1 The changes are physiologic and do not represent a disease process but nevertheless accompany a loss of substance or functional decline.2 The loss of functional reserve becomes particularly evident under the influence of internal and/or external stressors, leading to an increased risk of injury, such as falls and other traumas. In addition to physiologic age-related changes, many older patients have multiple comorbidities that signify an added risk for injuries, so in orthogeriatric patients, age-related changes as well as concomitant diseases play an important role in diagnosis, treatment and primary and secondary prevention. Important age-related changes in orthogeriatric patients and their consequences for patient care are discussed in this chapter.
DIVERSITY OF AGING AND FUNCTIONAL DECLINE
When people speak of older adults, they often mean a homogeneous group of individuals beyond the age of 65 years. This does not recognize the great differences between 65- and 75-year olds, and particularly those beyond the age of 80, the so-called ‘oldest old’. In addition, even within a particular chronological age cohort of older adults, there is extensive diversity due to various factors such as genetic background and preventive measures as well as the presence of mono- or multimorbidity. As a consequence, older adults need a customized diagnostic and treatment approach. This is also true for orthogeriatric patients.
Nearly all organ systems show signs of an aging process, what we usually mean by the term ‘normal aging’. The term ‘successful aging’ means that these normal declines over the lifespan do not negatively interfere with functionality and thereby independence. By accepting aging as a normal process, geriatricians therefore view the ‘anti-aging’ hype with a certain reserve, as we usually do not start to treat as long as functionality in the activities of daily living (ADL) is preserved. When treatment is required, it is often carried out by interdisciplinary teams.
Another characteristic of orthogeriatric patients is the common co-existence of various chronic diseases. These have to be taken into account when dealing with such patients as they can directly or indirectly interfere with surgical procedures. Some examples include frequent treatment with anticoagulants, arterial hypertension, diabetes mellitus and kidney dysfunction. Comorbidities may also be risk factors for perioperative complications such as delirium (detailed below).
PRINCIPLES OF NUTRITIONAL AND FLUID INTAKE
The caloric demands of older adults are around 10% less than those of younger adults and are 25–30 kcal/kg body weight per day. This demand is only lower when mobility is decreased to a significant extent. Adequate protein intake is especially important in multimorbid patients with frailty (see below) who should consume 1.0–1.2 g/kg body weight per day.3 Older persons show a good protein anabolism potential but reach an earlier ceiling effect. This means that protein intake has to be well distributed over all meals during the day. If such intake is not possible, food has to be fortified or oral protein-rich supplements given between meals.
Malnutrition is frequent in older adults, and in those admitted to hospital, the risk of overt malnutrition is above 50%. Nutritional state can be easily determined using the Mini Nutritional Assessment (MNA) instrument, the only nutritional screening tool especially developed for older adults.4
Weight reducing diets in older persons are nearly always contraindicated, as elderly individuals mainly lose muscle mass when their caloric intake is lower than their daily needs. If a diet is introduced, it must be accompanied by a physical activity program to preserve the – often already diminished – muscle mass. The loss of fat-free mass (mainly muscle) leads to sarcopenia (see below) and often causes falls with subsequent fragility fractures.
Regarding adequate fluid intake, a daily intake of 1500–2000 mL is considered necessary. A fluid intake history is important, as older women especially often do not achieve such volumes in daily life. This fluid volume includes fluid in foods. A frequent problem is the continuation of diuretic therapy which may lead to falls due to orthostatic dysregulation, as well as being an important risk factor for perioperative cognitive disturbance. This has to be balanced against the fear of cardiac decompensation due to the significant functional implications and possibilities for complications.
AGE AS A RISK FACTOR FOR DELIRIUM*
Delirium is the most frequent mental disorder in older individuals in the acute setting and the development of postoperative delirium is a common complication in geriatric patients. As age is one of the strongest risk factors for delirium, the likelihood of developing delirium increases with age. The incidence of delirium in hospitalized patients is affected by predisposing factors and the severity of the underlying cause of hospitalization. Older people undergoing surgery for a fracture are particularly prone to delirium.
Cognitive impairment and dementia are also strong risk factors for the development of delirium and present in more than 50% of surgical patients presenting with delirium. Cognitive impairment can last up to 1 year postoperatively.5,6
Delirium often shows a multifactorial causal mechanism. Several interacting biological factors result in disruption of the neuronal networks of the brain, resulting in acute cognitive dysfunction.7 Current evidence suggests that neuroinflammatory processes, changes in the balance of neurotransmitters, physiological stressors, metabolic derangements as well as electrolyte disorders and genetic factors contribute to the development of delirium.8,9
Many transmitters are implicated in disturbed neurotransmission, but cholinergic deficiency and/or dopaminergic excess are of special importance as these systems are often influenced by medications known to interfere with synaptic transmission and therefore potentially cause delirium. Cytokines, such as IL-1, IL-2, IL-6, TNFα and interferon, which influence the permeability of the blood–brain barrier, disturb the process of neurotransmission. In addition, systemic inflammatory processes, trauma, hypoxia and even surgery cause an increase in cytokine levels, resulting in activation of the microglia and presenting a risk for delirium.
Risk factors for the development of delirium in orthopaedic patients, which should be assessed routinely in every patient, are as follows:
Advanced age
Pre-existing cognitive impairment
Polypharmacy
Development of delirium during/after surgery
Small changes in fluid and food balance
Decline in sight and/or hearing
Functional impairment
Pain
Immobility
Physical restraints including bladder catheters, infusions, etc.
IDENTIFICATION OF INFECTIONS
Infections are the main cause of mortality in older hospitalized patients and are a common complication in orthogeriatric patients. This applies both to patients living in long-term care facilities and to patients who before hospitalization lived independently in their own homes. Mortality risk due to infections rises with increasing age and is strongly influenced by the presence of comorbidities, such as diabetes, circulatory disturbances or chronic heart failure.10 Immunological changes that accompany increasing age, functional impairment and changes in physiological barriers, such as the skin and the mucous membrane, favour infections in older individuals. In addition to prevention, early recognition and initiation of therapy are very important to reduce the impact of infections in geriatric patients.
Common infections in orthogeriatric patients are urinary tract infections (UTI), pneumonia, wound infections and catheter associated infections. UTIs are favoured by the presence of underlying incontinence, immobility and particularly urinary catheters. The incidence of bacteriuria due to urinary catheters is 3–10% and is considered a strong risk factor for the development of nosocomial UTIs.11 Dysuria, one of the main symptoms of UTIs in younger patients, is often missing, presenting a challenge for the treating physician to distinguish between an asymptomatic UTI and a bacteriuria. However, such differentiation is important as antibiotic treatment for a bacteriuria does not affect morbidity but often results in adverse drug events and other negative consequences. Therefore, diagnosis of a UTI requires thorough clinical evaluation and often urinary analyses and cultures.12
Pneumonia is encouraged by restricted clearing of the respiratory tract, and alterations in lung structure and respiratory mechanics.13,14 Compared with younger individuals, up to 36% of older patients with pneumonia present without cough with/without expectoration and sometimes without fever.15,16
These examples demonstrate that avoidance of diagnostic delays in older patients is often difficult as symptoms of infection are frequently atypical and non-specific and the informative value of diagnostic tools differs from that in younger patients.
Very often, a non-specific presentation, such as a fall, or acute alterations in cognitive function (delirium) and/or mobility may herald an underlying infection in old age. Weakness and fatigue are common complaints in the older person, often resulting in emergency department visits. As recent literature has shown, pneumonia and UTIs are among the most common primary diagnoses causing weakness and fatigue.17 Therefore it is vital that even subtle changes are recognized in the treatment of these vulnerable patients.
Careful interpretation of vital as well as laboratory parameters in older patients with infections reveals characteristic features that must be taken into account. Pathological results can be markedly reduced or even missing in infection.18 For example, tachycardia, one of the trigger symptoms in severe infections, can be missing in older patients due to reduced heart rate variability and polypharmacy.19
Fever, one of the cardinal symptoms in bacterial infection, is missing in up to 30% of older patients.20 This is due to a decline in basal body temperature (–0.15°C per decade), decreased thermoregulation, and reduced and inadequate production of endogenous pyrogens.21,22 The cutoff temperature for ‘fever’ is defined inconsistently in clinical guidelines as between 38.0°C and 38.3°C. As these guidelines do not take into account the special characteristics of older patients, it is assumed that lower cutoff values have to be considered when evaluating for infections in older adults. First data from the emergency department show that a cutoff tympanal temperature of 37.3°C or rectal temperature of 37.8°C should trigger further diagnostic investigation for bacterial infection.23
In addition, pathological laboratory test results, for instance indicating leucocytosis or elevated C-reactive protein (CRP), can be missing or only slightly elevated at the beginning of an infection and therefore are unreliable parameters to identify infections in older patients.16 Identification of infections without an inflammatory response is important in the treatment of older patients as it is associated with greatly increased mortality.24
Further diagnostic tools, such as chest X-rays for the identification of pneumonia, are diagnostically limited, as alterations in lung structure are often non-specific and infiltrates can persist for months.25
Identification of infections in older patients can be a big challenge. Therefore in older patients with non-specific clinical symptoms (weakness, fatigue, acute change in functional or cognitive status, falls, etc.) the diagnosis of an underlying infection should be considered even if vital or laboratory parameters are only slightly abnormal, and radiographic intervention does not show any obvious underlying causes of infection.
CHRONIC AND ACUTE PAIN
‘Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’.26 There are various definitions for the duration of chronic pain, but most describe chronic pain as lasting more than 3–6 months.
Inadequate pain management in the older patient is a common problem in both acute and chronic pain and is pronounced in cognitively impaired patients. This not only means discomfort for the patient but is also associated with negative effects on the patient’s health, impaired functional abilities and increased healthcare costs.
Previous observational studies have found that postoperative pain in older adults undergoing lower extremity orthopaedic surgery is associated with an increased risk of delirium, prolonged hospital stay and rehabilitation, higher probability of a physiotherapy session being missed or shortened, delays in ambulation postoperatively, impaired functional recovery and greater pain at 6 months after the surgery (Figure 2.1).27,28 The consequences of pain in older patients differ from those in younger patients, as functional decline is associated with diminished functional reserve (Figure 2.2).
Barriers to adequate analgesia (i.e. timely administration and effective pain control) are listed in Table 2.1. Despite these barriers there is a widespread misperception among patients and physicians that pain is a physiological consequence of aging. However, pain is not an age-related change, but an unpleasant sensory experience that has to be assessed and treated. No physiological changes in pain perception in older adults have been demonstrated, but there is evidence that older adults experience more pain than younger individuals.29
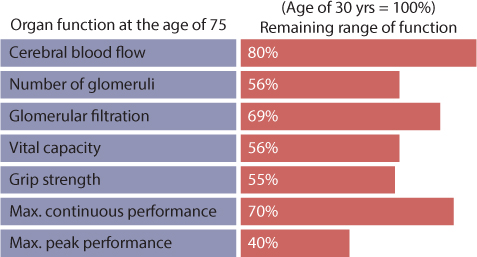
Figure 2.1 Organ function at the age of 75. (Adapted from Shock NW, et al. Normal Human Aging: Baltimore Longitudinal Study of Aging. Baltimore: NIH, 1984.)
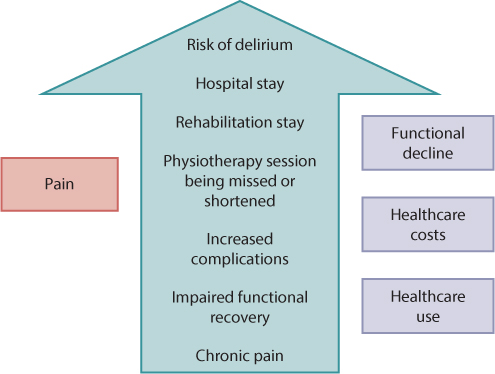
Figure 2.2 Consequences of inadequate pain management in older patients.
Table 2.1 Common causes of inadequate analgesic administration in the elderly
Under-reporting of pain |
Inadequate knowledge of pain assessment and management |
Missing pain assessment |
Concerns about the use of analgesics in older comorbid and/or cognitively impaired patients |
Underreporting of pain is also a common problem in orthogeriatric patients. In addition to the fact that pain is often assumed to be associated with aging, under-reporting is caused by communication problems (hearing loss, problems with speaking, for example dry mouth, comorbidities such as Parkinson disease, etc.), fear of addiction and the side effects of pain treatment, and the incorrect assumption that the pain is related to a comorbidity rather than a trauma. As in infections, pain, especially in patients with cognitive impairment, often presents non-specifically and atypically. Delirium, an acute decline in function or an acute reduction in nutritional intake can all be caused by pain. Therefore it is important to look for subtle changes in patient behaviour, cognitive and functional status and use a standardized pain assessment instrument regularly.
In addition, pain management requires advanced knowledge of age-related changes regarding unspecific and/or atypical presentation of pain and changes affecting pharmacokinetics and pharmacodynamics.
METABOLIC CHANGES (RENAL, LIVER, GUT) AND THEIR IMPACT ON MEDICATION
Geriatric patients are characterized by multimorbidity that often results in polypharmacy. As age-related changes affect pharmacokinetics (what the body does to the drug) and pharmacodynamics (what the drug does to the body), such changes play an important role in the medication of older patients.30 Pharmacokinetics includes the resorption, distribution, metabolism and elimination of drugs. Age-related changes are also important in the management of orthogeriatric patients, for example regarding pain medication.
Resorption
Gastric bicarbonate secretion decreases with age as does intestinal blood flow and mucosal function, while intestinal villus atrophy increases. As gastric emptying time is also increased, older patients have decreased stomach protection and an increased risk of developing intestinal ulcers and gastrointestinal bleeding while taking non-steroidal anti-inflammatory drugs (NSAIDs).
Distribution
Increasing age is associated with a significant change in drug volume and distribution. The proportion of body fat increases, while the proportion of lean body mass decreases. Consequently, the percentage of body water decreases with age (Figure 2.3). This increases the risk of dehydration and also influences the volume and distribution of hydrophilic (water soluble) and lipophilic (fat soluble) drugs. In particular, initial serum concentrations for a given dose of a water soluble drug, such as digoxin or hydrochlorothiazide, are higher than expected, while a fat soluble drug, such as amiodarone or NSAIDs, shows a longer half-life as expected due to the slow release from fatty tissue.31
Malnourished patients show reduced plasma protein levels (including albumin). This also has an impact on medication in older patients as malnutrition commonly causes increased levels of unbound drugs, as for example NSAIDs with strong protein binding.
Drug metabolism
Metabolism of medications occurs mostly in the liver. Liver size and function also decrease with age. Hepatic blood flow is reduced by up to 25%, and the number of functional hepatocytes and enzyme activity decline.32 These changes result in altered first-pass metabolism and clearance of certain drugs, for example acetaminophen. Non-synthetic hepatic biotransformation reactions (e.g. oxidative) and synthetic enzymatic reactions (e.g. conjugation) also change with aging.1 These age-related changes in hepatic metabolism and clearance are difficult to estimate.
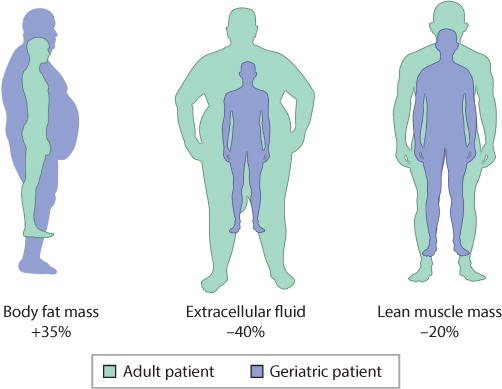
Figure 2.3 Changes in volume of distribution in old age.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








