Distal humeral fractures
INTRODUCTION
The objective of treatment for distal humerus fractures in the elderly is to restore a stable, functional and painless elbow, which will enable return to independence for activities of daily living. While the orthopaedic principles of anatomic reduction, stable fixation, preservation of soft tissues and early mobilization remain paramount in the surgical treatment of these injuries, they may often be difficult to achieve. The complex anatomy of the distal humerus, diminished bone quality, fracture comminution and articular involvement present numerous challenges to achieving a successful anatomic reconstruction.
Treatment advances for distal humerus fractures include a better appreciation of the role of non-operative management, the improved availability of computed tomography (CT) with three-dimensional reconstruction, an improved understanding of biomechanically advantageous fixation strategies, the development of periarticular precontoured locking plates and the selective use of elbow arthroplasty.
EPIDEMIOLOGY
Distal humerus fractures account for 1–2% of all fractures in adults.1 They have a bimodal age distribution with increased incidences occurring between the ages of 12 and 19 years, and in those aged 80 years and older.2 The first peak in fracture incidence typically occurs in adolescent males and is generally the result of high-energy injuries. The second peak incidence represents the fragility-type distal humerus fracture. These patients are characteristically female and the fractures usually occur as the result of low energy injuries, such as a fall from standing height.3,4
The overall incidence of elderly distal humerus fractures is increasing, in parallel to the increasing incidence of other osteoporotic fractures. An increasing activity level among the elderly population is believed to be a contributing factor to this observed trend.5 An American study performed from 1965 to 1974 identified the incidence of distal humerus fractures in patients greater than 70 years to be 20 per 100,000 persons.6 Subsequently, a Canadian study by Sheps et al.7 reported an incidence of 54 per 100,000 persons in the population 80 years or older, with females having an incidence approximately 1.5 times greater than males. A study of osteoporotic distal humerus fractures in Finnish women reported a twofold increase in the age-adjusted incidence of distal humerus fractures from 1970 (12/100,000) to 1995 (28/100,000) and predicted an additional threefold increase by 2030.8
When considering treatment options, the importance of patient functional status should be emphasized rather than chronological age. A large combined prospective and retrospective study has noted that greater than 80% of elderly patients presenting with isolated distal humerus fractures were in good general health and were living at home with reasonable independence of activities of daily living.5 Overall, 41% of men and 69% of women in the retrospective cohort portion of this study demonstrated radiographic signs of osteoporosis. Eighty-nine per cent of patients required surgical treatment and the presence of osteoporosis had a significant negative effect on clinical and radiological outcomes.
Although mortality risk following distal humerus fractures is not well established, it has not been recognized to be as substantial as that reported for other geriatric fractures such as proximal femur fractures.9,10 Nonetheless, these injuries may result in significant functional deterioration and eventually disability and loss of independence. The economic impact of these injuries may be offset by implementing treatment strategies which yield successful and timely functional outcomes with low complication rates. Furthermore, primary and secondary prevention strategies such as fall prevention and osteoporosis treatment should be implemented.
CLASSIFICATION
The most widely used classification system for distal humerus fractures is that of the AO/Orthopaedic Trauma Association (OTA).11 In this system, fractures are divided into three principle categories: type A (extra-articular), type B (partial articular) and type C (complete articular). Type A distal humerus fractures are extra-articular and may involve the epicondyles or occur at the distal humerus metaphyseal level. Type B fractures are partial articular with some degree of continuity between the humeral shaft segment and part of the articular segment. Type B fractures include unicondylar fractures and sagittal plane or coronal shear fractures of the articular surface. Type C fractures are complete articular fractures with no continuity between the humeral shaft segment and the articular segments. The AO/OTA system further subclassifies fractures based on fracture line and degree of comminution (types 1–3). Both the AO/OTA type A (extra-articular transcondylar) fractures and the AO/OTA type C fractures have been reported as the most frequent variants identified in geriatric patients.5,7
Anatomical considerations
The distal humerus can be considered as a divergent two column structure supporting the distal articular surface. The distal humeral shaft is triangular shaped in cross-section with its apex directed anteriorly. The medial column diverges approximately 45 degrees from the shaft in the coronal plane, whereas the lateral column diverges at approximately 20 degrees from the shaft.2 The trochlea connects the columns centrally and forms an articulation with the coronoid and olecranon facets of the ulna. The anatomy of the trochlea is analogous to that of a spool. The capitellum is the distal-most portion of the lateral column, which articulates with the radial head. The trochlea is more distal than the capitellum in the coronal plane, which results in a valgus alignment of 4–8 degrees. The distal articular segment of the humerus is internally rotated 3–8 degrees relative to the epicondyles and has 30–40 degrees of anterior angulation relative to the central axis of the humerus.12 The distal posterior portion of the lateral column is non-articular and permits distal placement of contoured posterolateral plates (Figure 23.1).
The lateral collateral ligament (LCL) consists of the lateral ulnar collateral ligament, the radial collateral ligament and the annular ligament. The lateral ulnar collateral ligament originates on the lateral epicondyle and inserts at the crista supinatoris of the ulna. The radial collateral ligament originates at the lateral epicondyle and merges with the annular ligament distally. The annular ligament attaches to the anterior and posterior margins of the lesser sigmoid notch of the ulna and encircles the radial head. The LCL is considered the primary soft tissue stabilizer of varus angulation and posterolateral rotation and it must be identified and protected during approaches to the radiocapitellar joint and during lateral plate application.
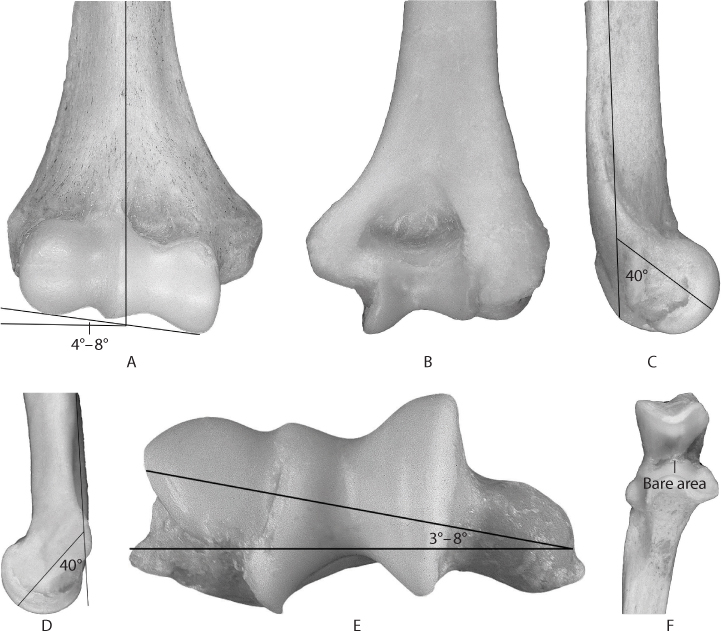
Figure 23.1 Distal humerus anatomy (a–f).
The medial collateral ligament (MCL) originates from the anteroinferior surface of the medial epicondyle and consists of three distinct bundles: anterior, posterior and transverse. The anterior bundle is considered the most important ligamentous stabilizer against valgus stress and posteromedial instability. The anterior bundle of the MCL inserts onto the sublime tubercle on the anteromedial aspect of the coronoid process.13 The fan-shaped posterior bundle attaches to the medial margin of the trochlear notch and provides secondary valgus stability at higher flexion angles.14 The medial column and medial epicondyle can accommodate medial plate placement without impinging on the MCL origin.
CLINICAL ASSESSMENT
An accurate history should define the mechanism of injury and identify any possible cardiovascular, neurologic and pharmacologic precipitants of the fall in geriatric distal humeral fractures.4 A thorough evaluation for associated injuries must be completed. The medical history should identify comorbidities and reversible illnesses that may impact treatment recommendations and perioperative risk. Patient cognitive status and ability to comply with rehabilitation, functional status, pre-existing elbow pathology and social circumstances are important treatment considerations.
The injured extremity should be examined for signs of soft tissue injury and compromise including oedema, bruising, abrasions, fracture blisters, skin tenting and open wounds. The standard open fracture treatment protocol should be initiated in a timely fashion for open distal humerus fractures. A thorough neurologic examination must be performed and accurately documented.
Incomplete ulnar neuropathy has been reported in 26% of patients with type C distal humerus fractures at the time of presentation.15 Any clinical suggestion of vascular compromise should prompt comprehensive assessment, including brachial-brachial Doppler pressure index and vascular surgeon consultation. Compartment syndrome should always be considered, particularly in the setting of high-energy trauma, and compartment pressures assessed when the clinical examination is inconclusive.
Imaging
Standard anteroposterior and lateral radiographs of the elbow should be performed. Radiographs taken out of immobilization where splint material may impair fracture visualization, as well as traction radiographs, may be beneficial.
Computed tomography imaging is helpful in delineating complex fracture patterns such as coronal plane articular fractures, comminuted or segmental articular fractures, and ‘low’ transverse extra-articular fractures. Increased interobserver and intraobserver reliability for fracture classification as well as increased intraobserver reliability for treatment decisions has been reported with the use of three-dimensional CT.16 CT is particularly useful in instances where a less invasive surgical approach for open reduction and internal fixation (ORIF) is being contemplated, such as using a paratricipital approach rather than an olecranon osteotomy. CT may also help to identify highly comminuted articular fractures in the elderly, which may be better treated with primary arthroplasty.
TREATMENT
Non-operative treatment
Complex distal humerus fractures were often historically managed non-operatively with cast immobilization, collar and cuff treatment or early mobilization.17,18 A number of studies have demonstrated that ORIF yields better outcomes than non-operative treatment.15,19,20,21 and 22 A pooled analysis of two level III studies, including one that was based exclusively on patients aged 75 years or older, demonstrated that patients treated non-operatively are almost three times more likely to have an unacceptable result.23 Another retrospective study reported that nonoperatively treated patients were almost six times more likely to have a nonunion and four times more likely to have delayed union than operatively treated patients.3
While non-operative management of complex distal humerus fractures in the elderly is generally reserved for patients with limited pre-existing function of their fractured arm or when medical comorbidities preclude operative treatment,24 it may represent a safe treatment option with satisfactory clinical results.25
Cast immobilization is generally the preferred non-operative treatment. A well-padded cast is applied with the elbow at 90 degrees of flexion and the forearm in neutral rotation for 6–8 weeks. Frequent follow-up visits are required to ensure appropriate cast fit and that there has been no development of soft tissue compromise. Once bony union is evident, active range of motion is encouraged. Physiotherapy with static progressive splinting is prescribed in selected patients where the recovery of motion is slow. Collar and cuff immobilization is the recommended non-operative treatment modality for patients with widely displaced fractures and those with cognitive or communicative disability which prevents them from conveying symptoms of an ill-fitting cast and resultant development of pressure ulcers. Despite the prolonged immobilization period often required to achieve union, elbow stiffness is not common in this patient group. A recently published26 retrospective review of 19 medically unwell and elderly patients treated non-operatively for a fracture of the distal humerus at our institution demonstrated an 81% union rate with an overall 68% good to excellent subjective outcome at final follow-up (Figure 23.2). The mean elbow flexion extension arc was 22–128 degrees, a mean Mayo Elbow Performance Score (MEPS) of 90 and a mean Disabilities of the Arm, Shoulder and Hand (DASH) score of 38. One patient with a distal humeral non-union was sufficiently symptomatic to undergo a total elbow arthroplasty (TEA).
Open reduction and internal fixation
ORIF is recommended for displaced or angulated distal humeral fractures in the elderly. Rigid internal fixation allows for anatomic fracture reduction and permits early range of motion, which is essential in preventing post-traumatic elbow stiffness. Anatomic reduction of the articular surface and overall elbow alignment are prioritized over early motion when stable fixation is unattainable. However, in elderly patients with poor intraoperative fixation stability, consideration should be given to conversion to a primary arthroplasty. A secondary arthroplasty for failed internal fixation has a higher complication rate and a poorer functional outcome than a primary arthroplasty.
POSITIONING AND APPROACHES
The patient can either be positioned in the supine position, with the elbow supported by a sterile bolster or folded sheet placed on the patient’s chest. An alternative is the lateral decubitus position using a bean bag with the elbow supported on an arthroscopy arm holder. A commercially available articulated arm positioner can be used in the supine position when an assistant is unavailable. This device also takes pressure off the patient’s chest, which may be important in patients with compromised pulmonary capacity or those undergoing surgery under a regional anaesthetic.
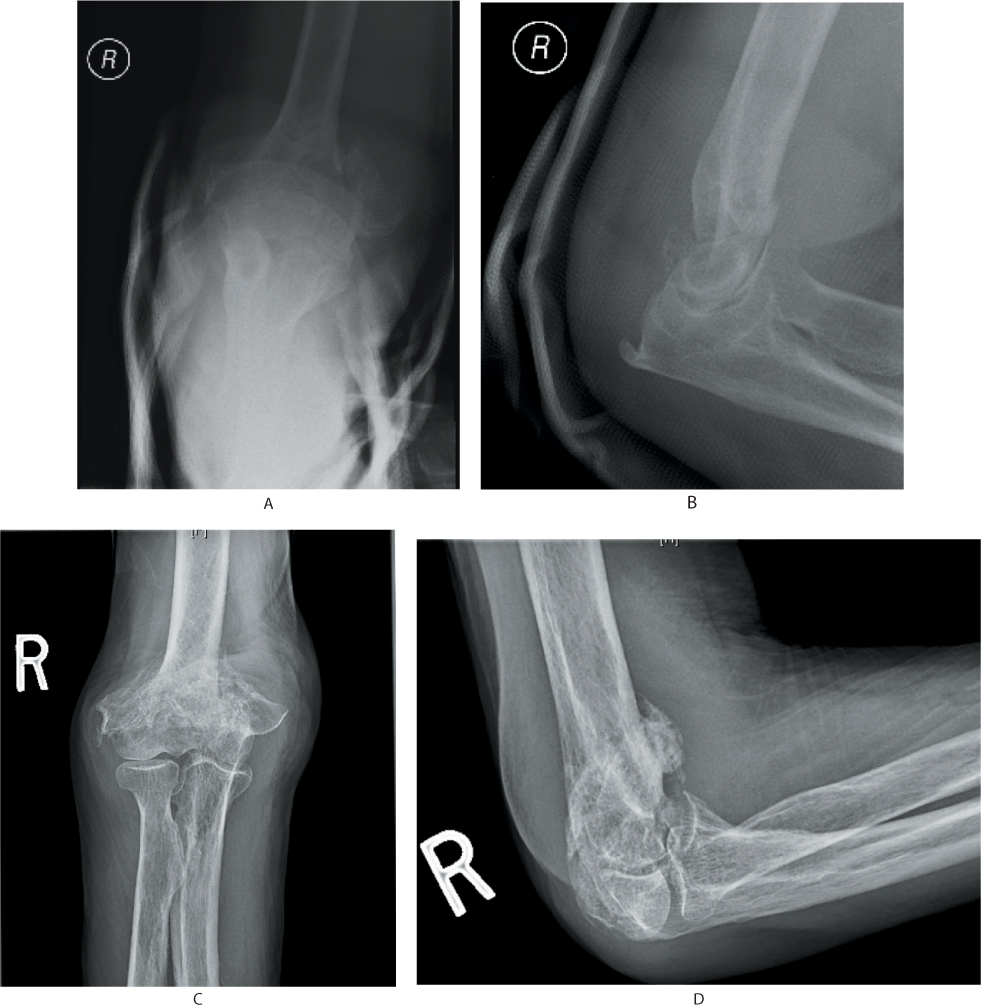
Figure 23.2 A 93-year-old man with a type C distal humerus fracture, treated non-operatively with pain free elbow and functional range of motion at last follow-up (a–d).
The choice of surgical approach depends on several factors. It must provide adequate exposure to permit anatomic reduction and appropriate fixation while minimizing soft tissue disruption. Fracture pattern, extent of articular involvement, associated soft tissue injury, rehabilitation protocol, surgeon preference and the possibility of intraoperative conversion to arthroplasty must be considered.
In general, a utilitarian posterior skin incision with elevation of full-thickness fasciocutaneous medial and lateral flaps is used to access the distal humerus through one of the posterior approaches or through medial or lateral approaches. Although a direct lateral incision and approach through the Kocher interval, Kaplan interval or a common extensor tendon split can be used for treatment of capitellar fractures and simple partial articular lateral column fractures, the direct midline posterior incision is advantageous as it permits unrestricted access to both the medial and lateral columns and has also been shown to have a decreased risk of cutaneous nerve injury.27 Furthermore, the same incision can be used for contracture release and for elbow arthroplasty if required secondarily.
The ulnar nerve should be identified and protected throughout the course of the procedure. The necessity for transposition of the ulnar nerve is controversial. If the nerve demonstrates instability or has a tendency to lie over the applied medial plate, anterior transposition should be considered. In the setting of preoperative ulnar nerve dysfunction, transposition has been recommended.28 In the absence of definitive data, the authors routinely perform an ulnar nerve transposition for all distal humeral fractures requiring medial column fixation.
Posterior approaches include the olecranon osteotomy, the paratricipital ‘triceps on’ and the ‘triceps off’ approaches. Triceps off approaches include triceps reflecting, triceps splitting and the triceps tongue approaches. The fracture characteristics, including the degree and complexity of articular involvement, dictate the most appropriate surgical approach.
Visualization of the distal humerus articular segment varies with each approach. The olecranon osteotomy approach has been shown to expose 57% of the distal articular segment, whereas the triceps splitting and triceps reflecting approaches have been shown to expose 35% and 46%, respectively.29 The latter approaches can generally be used for simple extra-articular fractures. The triceps off approaches require postoperative protective protocols that may be impractical in the geriatric population. These protocols restrict elbow flexion and limit triceps activation, which may compromise the patient’s ability to mobilize with ambulatory aids and to perform their activities of daily living.
Potential complications associated with olecranon osteotomy include malunion, nonunion and symptomatic internal fixation. Eight per cent of patients who had undergone olecranon osteotomy required removal of symptomatic osteotomy fixation, regardless of the fixation used.30 Schmidt-Horlohé et al.31 reported a 22.5% complication rate, including delayed or nonunion and screw loosening, and 48.4% rate of fixation removal in their series of 31 patients with olecranon osteotomies repaired with one-third semi-tubular hook plates. Ring et al.32 achieved a 98% union rate at 6 months postoperatively using tension band fixation of the olecranon osteotomy, with 27% of the patients in their series requiring K-wire removal. Hewins et al.33 reported a 100% union rate with only one of 17 patients requiring fixation removal in their series of olecranon osteotomies repaired with plate fixation. Hewins et al. suggested that plate fixation may provide a more rigid and stable construct by offering more potential points of fixation, increased resistance to tensile forces along the posterior surface of the olecranon and improved resistance of both shear and rotational forces along the osteotomy site.
Olecranon osteotomy
While olecranon osteotomy provides the best visualization of the articular segment,29 it should be avoided if primary arthroplasty is being considered. The paratricipital approach is preferred for cases where repairability of the fracture is to be determined intraoperatively.
After elevating full-thickness fasciocutaneous flaps, the olecranon bare area is identified through a medial and limited lateral dissection. Predrilling and fixation of a precontoured periarticular locking plate prior to osteotomy simplifies osteotomy reduction and fixation. An apex distal chevron osteotomy provides intrinsic stability though its necessity when using rigid plate fixation is debated. The osteotomy should be cut two-thirds with a saw and the remaining one-third predrilled with a K-wire and completed with osteotomes. This facilitates achieving an anatomic reduction and contact of the fragments33 (Figure 23.3).
Preserving the innervation of the anconeus by dissecting it from the distal ulna without detaching it from the triceps has been recommended by some authors.34 The exposure may be extended proximally by continuing into the paratricipital approach.
Paratricipital approach
The triceps sparing paratricipital approach provides limited visualization of the articular segment and is best reserved for extra-articular or simple intra-articular fractures with minimal comminution (Figure 23.4). This approach avoids disruption of the extensor mechanism and skeletonization and devascularization of the proximal ulna. Because the triceps mechanism is preserved, the extensor mechanism does not need to be protected and immediate active triceps function can be initiated in the postoperative rehabilitation program. The authors prefer the lateral para-olecranon approach35 for TEA as it allows improved exposure of the ulna for preparation and placement of the ulnar component relative to the paratricipital approach without detaching the main insertion of the triceps on the olecranon. A description of this approach is outlined below.
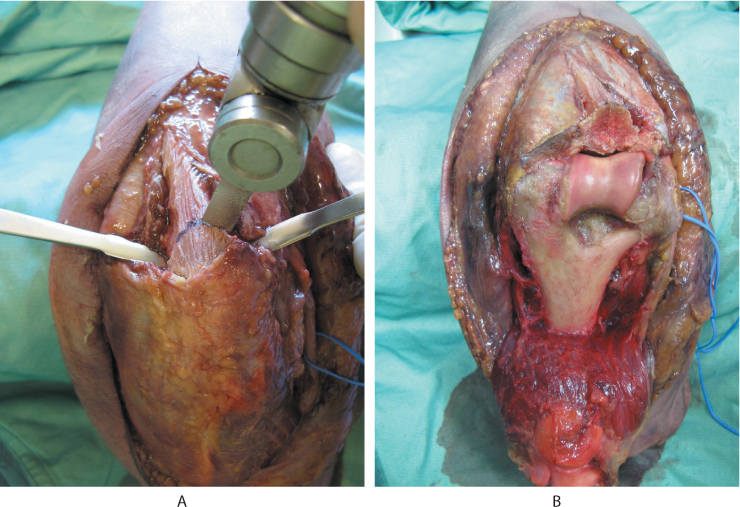
Figure 23.3 Olecranon osteotomy (a) Apex distal chevron osteotomy. (b) Exposure with olecranon osteotomy reflected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








