Patellar fractures
INTRODUCTION
The patella is the largest sesamoid bone in the human body. It serves as the fulcrum of the extensor mechanism between the quadriceps and patellar tendons. The patella shifts the moment arm of the quadriceps anteriorly thereby increasing the efficiency of the extension force. Fractures of the patella most commonly occur following a simple fall in the elderly, with open fractures rare. In the elderly patient, fractures can also occur around a total knee arthroplasty or could be due to a pathological lesion.
The primary goal of management in the elderly patient is to regain function. Treatment is guided by bone quality, fracture pattern, physical examination, as well as the patient’s functional status and medical comorbidities. Options for treatment include non-operative management, open reduction internal fixation, partial patellectomy and in rare cases total patellectomy.
EPIDEMIOLOGY
Patellar fractures represent about 1% of all fractures,1,2 with an incidence in the elderly of 0.5 per 1000 from a national database of patients the over the age of 65 years.3 The risk of patellar fracture is about 3.5 times higher in women than men. There is conflicting data on whether each decade of life adds further risk of a patellar fracture.3 In a study of patellar fractures in 68 patients over the age of 65, Shabat et al.4 demonstrated that 66% had a comminuted fracture pattern and 85% of fractures were associated with disruption of the extensor mechanism requiring surgical fixation.
Associated injuries may include hip dislocations, knee ligamentous injuries, femoral neck or shaft fractures and distal femur or proximal tibia fractures.2,3 Fractures can also occur after total knee arthroplasty, anterior cruciate ligament (ACL) graft harvesting or due to a pathological lesion. Primary patellar tumours are exceedingly rare, with predominantly case reports and small series in the literature. Benign tumours are more common than malignant, with a giant cell tumour being the most commonly reported lesion.5
Mechanism of injury
Fractures of the patella can be caused by either a direct blow or indirectly through eccentric contraction of the quadriceps. The most common mechanism of injury in the elderly is a simple low energy fall from standing height.1 The subcutaneous position of the patella increases the chance of direct trauma and open injury. Open patellar fractures are rare, and more frequent following a high energy injury such as a motor vehicle collision. Open fractures are more likely to have associated injuries and a higher Injury Severity Score (ISS).
Periprosthetic fractures
The overall prevalence of total knee arthroplasty in the United States is estimated to be 4.2% in those over 50 years of age, with increasing prevalence in each decade of life. The estimated number of patients who have had a total knee arthroplasty in the United States alone is over 4 million.6 Patellar fractures may be the most common periprosthetic fracture after total knee arthroplasty with a very large range of reported prevalence ranging from 0.05% to 21%.7,8,9 and 10 The true prevalence of periprosthetic patellar fracture is likely below 1%. However, given the large numbers of current and future total knee arthroplasty patients, periprosthetic patellar fractures will continue to become more common in the elderly population.
Patellar fractures are much more common after total knee arthroplasty (TKA) when the patella is resurfaced.11 Factors that have been shown to increase the risk of fracture after resurfacing are the number of previous surgeries, preoperative mechanical limb malalignment, postoperative patellar tendon length and patellar post-resection thickness.12
CLASSIFICATION
The commonly utilized classification systems for patellar fractures are descriptive in nature. Fractures can be broadly described as non-displaced or displaced. Displacement has been defined as articular step-off of greater than 2 mm and/or fragment separation of greater than 3 mm.13,14,15 and 16 The degree of displacement is associated with the severity of medial and lateral retinacular damage. Displaced fractures with disruption of the extensor mechanism are often treated surgically given the inferior outcomes associated with non-operative treatment.16
Non-displaced and displaced fractures are further categorized by location and pattern of fracture. Patellar fracture descriptions by location and pattern may be predictive of the injury mechanism. Several common descriptive patterns of fracture are shown in Figure 38.1. Pattern descriptors include transverse, vertical, stellate and multifragmented. These patterns may be non-comminuted or comminuted. Elderly patients are more likely to sustain comminuted fractures of the patella.4,17 Location descriptors include proximal pole, distal pole or osteochondral. Osteochondral fractures are typically seen in younger patients.
The Orthopaedic Trauma Association (OTA) classification system designates the patella as location 34. This classification divides patella fractures into the standard A-type extra-articular, B-type partial articular, vertical, and C-type complete articular, non-vertical.18 There is no prognostic outcome data for the OTA classification system; however, it is useful for the purposes of research.
Anatomical considerations
The patella is a triangular bone that resides within the quadriceps femoris tendon. It is convex and is covered by a continuation of the quadriceps tendon anteriorly. The superior three-fourths of the posterior patella is covered by thick articular cartilage. The distal anterior apex of bone serves as the origin of the patellar tendon. The posterior surface of the patella is divided into two major medial and lateral facets separated by a large vertical ridge. The medial and lateral facets are divided transversely by two smaller ridges, creating superior, intermediate and inferior facets. A smaller vertical ridge at the medial edge of the posterior patella separates the medial facet from the small facet.1
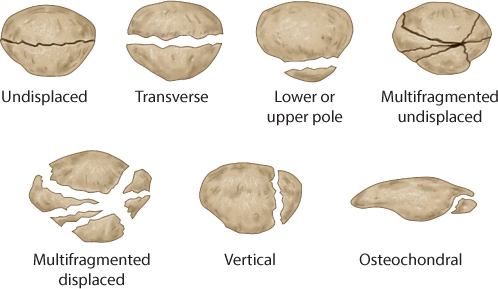
Figure 38.1 Patellar fracture patterns.
The patella typically forms from a single ossification center. There is anomalous ossification in approximately 3% of the population causing a bipartite or tripartite patella. One or two irregular fragments with smooth cortical edges are seen at the superolateral corner of the patella. This anomaly is more common bilaterally.19 This developmental variation should not be mistaken for an acute fracture (Figure 38.2).
The vascular supply of the patella has been of interest due to the risk of osteonecrosis and the prevalence of anterior knee pain after injury. Scapinelli20 described the extraosseous and intraosseous vascular supply of the patella. The extraosseous system is an anastomotic ring comprised of the supreme genicular, medial superior genicular, medial inferior genicular, lateral superior genicular, lateral inferior genicular and anterior tibial recurrent arteries. The intraosseous arteries are organized into two separate systems. The first are the mid-patellar vessels that enter the patella from the anterior surface. The second are the polar vessels that enter the patella from the distal pole, between the patellar tendon and the articular cartilage. Given this vascular arrangement, the proximal pole of the patella is at risk of devascularization following fracture (Figure 38.3).20,21
CLINICAL ASSESSMENT
The patient should be evaluated with a complete history and physical examination. A history of direct trauma to the knee or eccentric load and subsequent knee pain should alert the clinician to a possible extensor mechanism injury. A large hemarthrosis may be present depending on the injury to the retinaculum. Removal of the hemarthrosis and injection of local anesthetic can help facilitate further physical examination testing, although the literature to support this is limited. Patients can often retain a portion of their active extension in the setting of a patella fracture if the medial and/or lateral retinaculum is intact. In this setting, an extension lag is often seen. With a patellar fracture and complete rupture of the retinaculum, the patient will have no ability to actively extend the knee and perform a straight leg raise.
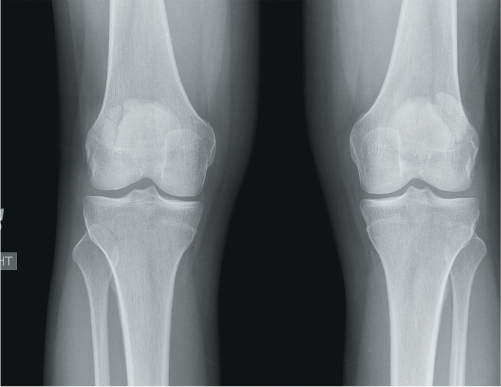
Figure 38.2 Standing bilateral knee radiographs demonstrating a right-sided tripartite patella and a left-sided bipartite patella.
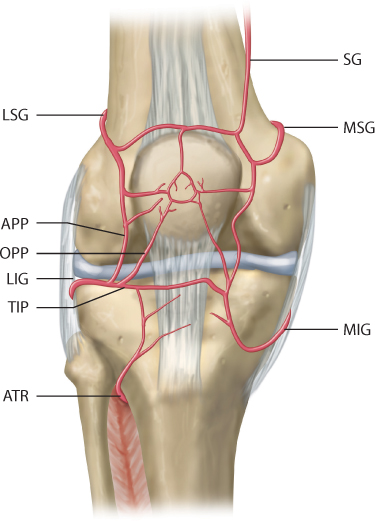
Figure 38.3 Arterial supply of the patella with the extraosseous geniculate system and intraosseous system. APP, ascending parapatellar artery; ATR, anterior tibial recurrent artery; LIG, lateral inferior genicular artery; LSG, lateral superior genicular artery; MIG, medial inferior genicular artery; MSG, medial superior genicular artery; OPP, oblique prepatellar artery; SG, supreme genicular artery; TIP, transverse infrapatellar artery. (Reprinted with permission from Scapinelli R. J Bone Joint Surg Br 1967;49(3):563–570.)
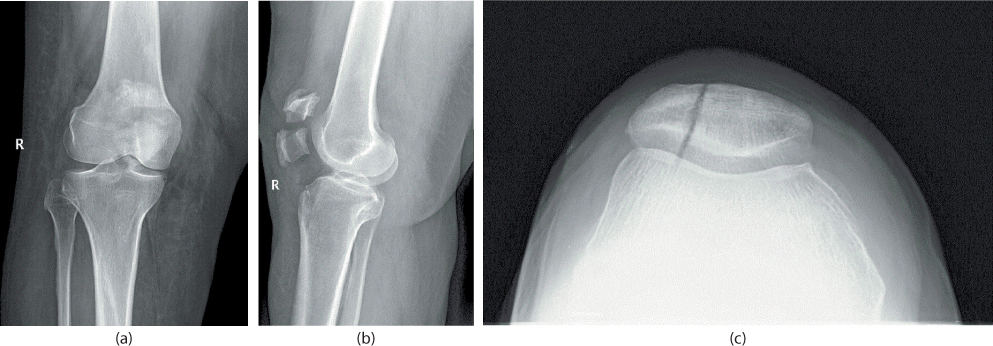
Figure 38.4 Anteroposterior (AP) (a) and lateral (b) views of a displaced transverse patellar fracture. Sunrise view of a vertical patellar fracture (c).
The subcutaneous patella should be palpated and examined for tenderness, crepitus or separation of fracture fragments if possible. Any lacerations, abrasions and contusions must be carefully examined for possible open injury. A saline load test can be performed with an intra-articular injection of 150 mL of sterile saline when in doubt, with extravasation of fluid from the wound or soft tissue seen.22
Imaging
Patellar fractures should be evaluated using anteroposterior, lateral and sunrise X-ray views. The superimposed distal femur may make interpretation of the anteroposterior (AP) view difficult. The lateral view allows a profile view of the patella demonstrating displacement and articular incongruity. The axial view is helpful for vertical and osteochondral fracture patterns (Figure 38.4). Further advanced imaging such as bone scan, CT or MRI are rarely needed. However, there may be a role for advanced imaging when evaluating for stress fractures in osteoporotic elderly patients or other pathologic lesions of the patella.5,23
TREATMENT
The treatment goals of patellar fracture management in the elderly are to restore prior functional level, maintain function of the extensor mechanism and restore articular congruence. The choice of fracture treatment depends on the fracture pattern, physical examination findings and the patient’s functional status and medical comorbidities. In the elderly, it is also important to consider age, bone quality, surgical risk and the ability to maintain weight bearing and range of motion restrictions.
Efforts should be made to preserve as much of the patella as possible. However, in cases of severe comminution, part or all of the patella may have to be excised. Options for treatment include non-operative treatment, open reduction internal fixation, partial patellectomy and total patellectomy.
Non-operative
Non-displaced fracture patterns are amenable to non-operative treatment. Fractures may be transverse, stellate or vertical. There should be no more than 3 mm of fracture fragment separation or 2 mm of articular incongruity, and there should be an intact extensor mechanism on physical exam.
Patients are immobilized with the knee held in extension for 4–6 weeks. This can be done with a cylinder or long leg cast, a hinged knee brace or a knee immobilizer. Weight bearing is allowed as tolerated with the knee in the extended position. Straight leg raising exercises may be initiated within several days.
Casts must be changed if there is any concern for skin compromise. The lighter hinged knee braces or knee immobilizers may be better tolerated by the elderly. However, the patient must reliably wear the brace as directed with the knee locked in extension for ambulation. After evidence of healing is noted, a program of strengthening and active motion is initiated. Typically the knee is allowed to flex in a staged manner. This can be done with a hinged knee brace, which can continue to be locked in extension for ambulation until the quadriceps strength and patella healing allow for a pain-free straight leg raise. One such protocol would be to allow flexion from 0 to 30 degrees after 6 weeks of extension. The amount of flexion can then be advanced by 30 degrees every 2–3 weeks thereafter with careful follow-up to ensure no further displacement. Elderly patients may require a closely monitored physical therapy regimen to maximize strength and motion.
Non-operative management may be appropriate for patients with displaced fractures in the face of significant medical comorbidities. These patients can be allowed to ambulate and initiate range of motion once their pain allows. Pritchett24 reported a series of 18 patients with patellar fractures displaced greater than 1 cm managed non-operatively. Twelve surviving patients were followed for 2 years. At follow-up, no patients had severe pain and nine patients had only minimal or moderate activity restrictions.
Operative
For displaced fractures and patients unable to perform a straight leg raise, operative intervention is routinely required. Generally, greater than 2 mm of displacement and/or articular incongruity are defined as displacement. The preferred open approach is a longitudinal midline incision centred over the patella. This approach can be extended proximally to the quadriceps tendon and distally to the tibial tubercle as needed. Percutaneous and external fixation methods have also been described.25,26 and 27 These techniques may be useful in cases of severe soft tissue damage.
OPEN REDUCTION INTERNAL FIXATION
Large, displaced vertical fracture fragments can be treated with lag screw fixation alone. For transverse or comminuted patterns, various techniques have been described consisting of wire fixation in cerclage or tension band configurations. These techniques have been evaluated biomechanically and clinically. The modified anterior tension band wire technique has been found to provide a superior fracture stability compared to other wiring techniques.2,13,15,28,29 The force across the patella during flexion causes apex anterior angulation. The anterior tension band allows conversion of the tension force to a compressive force at the articular surface of the patella. A cerclage wire or cancellous screws may be added for additional stability, especially in the face of comminution.29,30 Further studies have shown increased stability, decreased complications and good clinical outcomes when the tension band wire is threaded through cannulated screws.13,31
Modified anterior tension band wiring
Although Benjamin et al.32 showed screw fixation alone to be adequate for transverse fractures in patients with adequate bone, fixation in the elderly requires more stable fixation. Modified anterior tension band wiring remains the treatment of choice for transverse, non-comminuted patellar fractures with good bone stock. After incision, fracture edges are exposed and cleaned of hematoma and soft tissue. The knee joint should be thoroughly irrigated. A provisional reduction can be performed and held with reduction forceps to evaluate reduction. The reduction of the articular surface should be palpated through the retinacular tear. If the tear is too small, longitudinal medial or lateral arthrotomies can be performed as described by Carpenter et al.13 and Gardner et al.,33 respectively. Subsequently, 1.6 mm K-wires or 4.0 mm cancellous screws can be placed in a vertical, parallel manner to maintain the reduction and to anchor the cerclage wire. The reduction can also be taken down to allow the K-wires to be passed in a retrograde manner through the fracture site. A 14- or 16-gauge angiocatheter or equivalent is then passed through the patellar and quadriceps tendon adjacent to the patella, posterior to the tips of the K-wires. This minimizes the soft tissue between the cerclage wire and the bone. An 18-gauge wire is then passed through the catheter in a circular or a crossed figure-of-eight pattern. After ensuring reduction of the articular surface, the wire is then tightened. When using a figure-of-eight pattern, the medial and lateral loops should be tightened symmetrically. The proximal ends of the K-wires are then bent, twisted to face posteriorly around the cerclage wire and then buried into the proximal patella. The excess distal ends of the K-wires are then cut (Figure 38.5).34
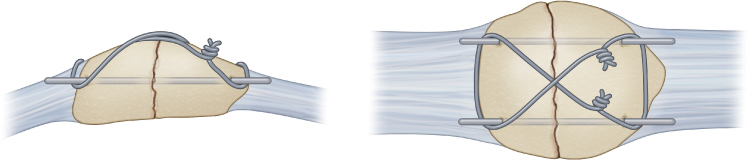
Figure 38.5 Modified anterior tension band construct. (Reprinted with permission from Archdeacon M, Sanders R. Patella fractures and extensor mechanism injuries. In: Browner B, Levine A, Jupiter J, Trafton P, Krettek C, editors. Skeletal Trauma. 4th Edition. Philadelphia, PA: Saunders; 2009. pp. 2131–2166.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








