Dislocations around the shoulder
Acromioclavicular joint dislocations
INTRODUCTION
The prevalence of traumatic dislocations of the shoulder in the elderly is increasing due to lifestyle changes and prolonged life expectancy. However, injury mechanisms, clinical manifestations and treatment modalities are routinely determined from data on younger patients.
The literature has demonstrated differences between the clinical manifestations and prognosis of elderly and young patients who sustain a dislocation of the shoulder. A dislocation of the shoulder is usually due to a low energy fall onto the outstretched hand in the elderly, unlike younger patients where it is commonly due to higher energy injuries, for example during sports.1 Recurrence is less commonly seen in the elderly, although higher morbidity can be expected due to associated rotator cuff tears, greater tuberosity fractures and/or nerve injuries.2
EPIDEMIOLOGY
Rowe reported an equivocal incidence for shoulder dislocations in patients below and above the age of 45 years.3 Recent studies have reported that 20–44% of patients with an anterior shoulder dislocation are over the age of 60 years.3,4 and 5 Rotator cuff tears are common sequelae of traumatic shoulder dislocations in the elderly, with the incidence ranging from 34% to 100%.4,6,7,8 and 9
McLaughlin10 suggested that a dislocation of the shoulder may occur due to failure of either the anterior structures that include the antero-inferior glenoid and labrum (anterior mechanism), or the posterior structures that include the postero-superior rotator cuff (posterior mechanism) (Figure 21.1).
In elderly patients, since the rotator cuff is the weakest structure due to normal age related degenerative changes, it is the first structure to give way and hence the anterior capsulolabral structures are relatively well preserved.10 Labral lesions are less commonly found in patients over 40 years compared to young patients following a traumatic dislocation.11 However, Gumina and Postacchini found anterior labral tears in all their patients and concluded that the anterior capsulolabral structures may be damaged and may contribute to recurrent dislocation in the elderly patient.4 Patients with recurrent dislocation over 55 years are routinely found to have either a Bankart lesion or glenoid rim fracture, along with a concomitant large or massive tear of the rotator cuff.12
The spectrum of injury mechanism may vary. At one end are patients with pre-existing degeneration of the rotator cuff that is disrupted as a consequence of the dislocation and results in a tear. The other end of the spectrum is where the rotator cuff is relatively intact and the anterior capsulolabral structures give way. In some patients both rotator cuff tear and Bankart lesion may coexist (Figure 21.2). Clinicians must be aware of the common associated pathologies and evaluate for these injuries as part of a thorough clinical assessment.
CLINICAL PRESENTATION
Patients can present with an acute dislocation in the emergency room or subacutely with a history of dislocation which has been reduced with persistent pain, weakness of the shoulder, neurological deficit, stiffness due to prolonged immobilization or recurrent dislocation. In an acutely dislocated shoulder, after reduction is achieved, the affected shoulder and upper limb are carefully examined. The first priority is to rule out neurovascular injury. The radial and brachial arteries are assessed and if the pulse is absent, further evaluation and treatment is the priority. Neurological assessment focuses on a thorough assessment of the brachial plexus and specifically the axillary nerve. The axillary nerve may be difficult to examine in the acute setting as a diminished or absent sensation in the military badge area may not be a reliable way of detecting a deficit.13
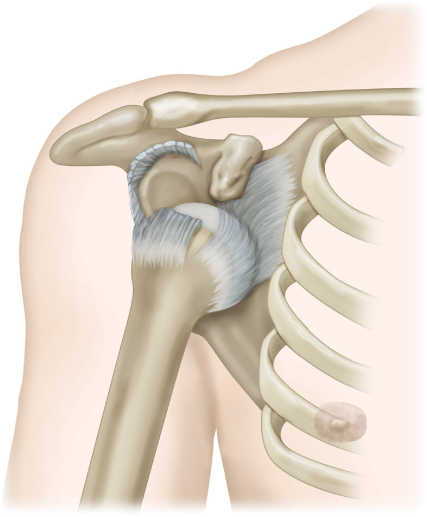
Figure 21.1 Posterior injury mechanism. Elderly patients with shoulder dislocation are prone to a tear of the rotator cuff. (Please note the direction of the dislocation is still anterior)
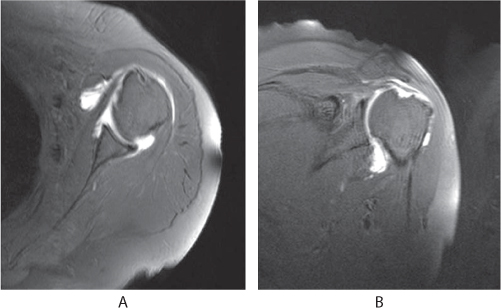
Figure 21.2 MRI of a 65-year-old patient following a primary anterior shoulder dislocation. The axial image shows a Bankart lesion (a) and the coronal image shows a medium sized full-thickness rotator cuff tear (b).
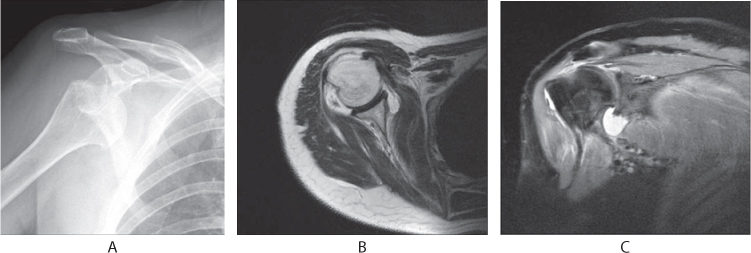
Figure 21.3 A 64-year-old patient following primary anterior shoulder dislocation (a). MRI axial image shows an anterior capsular tear with intact anterior labrum (b) and the coronal image shows a medium sized full-thickness rotator cuff tear (c).
Diagnostic imaging
In a patient with an acute dislocation, detailed plain radiographs include a true anteroposterior, modified axial and scapular lateral views prior to reduction. Associated injuries around the shoulder (e.g. greater tuberosity fracture) and other injuries in the upper limb should be excluded. After reduction of the dislocation the views have to be repeated to confirm congruency of the joint and to rule out other injuries. If there is any suspicion of associated fractures, a 3D CT scan should be performed.
FURTHER IMAGING
Ultrasound can aid in the diagnosis of rotator cuff tears. A recent Cochrane review concluded that ultrasound has a sensitivity and specificity similar to MRI for diagnosing a full-thickness rotator cuff tear and slightly inferior for diagnosing a partial-thickness tear.14 While it may allow for evaluation of tuberosity fractures or a Hill–Sachs lesion, ultrasound is not the ideal imaging modality for evaluating the labrum.15
An MRI or a MR arthrogram may help in determining the size of an associated rotator cuff tear, Bankart lesion and/or another anterior bony or capsulolabral lesion such as an anterior capsular tear (Figure 21.3). MRI is recommended when patients present with persistent weakness, pain or instability despite appropriate following dislocation. If an MRI is contraindicated e.g. due to metallic implants, a CT arthrogram may be useful for evaluation of the rotator cuff and has demonstrated comparable accuracy to MRI. The timing of MRI is a matter of controversy. One study recommended evaluating patients at 7–10 days post injury,16 while other authors have recommended an MRI can be done at 4 weeks without any increased incidence of stiffness.9,17
If a neurological deficit is suspected, an electromyography-nerve conduction velocity test (EMG-NCV) may be done at 4 weeks and repeated at 3 months if no improvement is seen. Although findings on EMG-NCV may be delayed, it may act as a baseline for further evaluation.
Associated injuries
PERIPHERAL NERVE INJURIES
A prospective study reported that the prevalence of associated nerve injuries in patients over the age of 65 years was 54%, which was more than the 26% seen in younger patients.13 The increased prevalence may be due to lower muscle tone, which allows the humeral head to displace more and therefore lead to greater disruption of the surrounding soft tissues. Another reason for the high prevalence of nerve injuries could be due to age related neural degeneration making injury following a simple dislocation more likely.
The most commonly involved nerve is the axillary nerve. The prevalence quoted in a large prospective study was 9.3%, compared to 4.6% in younger patients.4 However, the prevalence is increased when all patients are tested with electromyography.13 The proportion of nerve injuries as confirmed on NCV studies is found in Table 21.1.
AXILLARY ARTERY INJURIES
Although uncommon, an injury to the axillary artery can lead to devastating complications, particularly if there is a delay in diagnosis. A review of the literature demonstrates that of the axillary artery injuries reported following a dislocation of the shoulder, 86% are found in patients over 50 years of age18. Most injuries occur in the third part of the artery distal to the pectoralis minor, with 68% presenting with an axillary mass. Distal pulses may rarely be present due to collateral vessel flow and should not rule out an arterial injury. Any patient presenting with an axillary mass and diminished pulses after a shoulder dislocation should be investigated with an arteriogram for possible axillary artery injury and early vascular input is required. Atherosclerotic changes in the artery associated with tenting of the artery over the pectoralis minor may be responsible for the increased incidence of this injury in the elderly patient.18
Table 21.1 Incidence of nerve injuries following a dislocation of the shoulder
Nerve | Percentage injury |
|---|---|
Axillary | 37 |
Suprascapular | 29 |
Radial | 22 |
Musculocutaneous | 19 |
Ulnar | 8 |
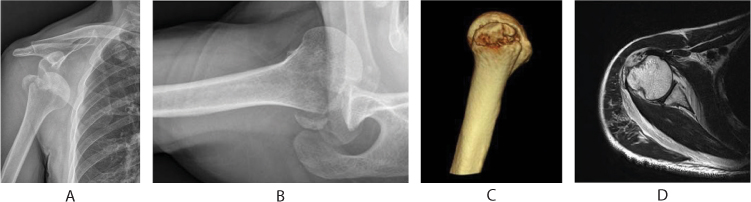
Figure 21.4 A 67-year-old patient with anterior shoulder dislocation with greater tuberosity fracture confirmed on radiographs (a,b), 3D-CT (c) and MRI (d).
ASSOCIATED FRACTURES
Approximately 15–30% of anterior shoulder dislocations are associated with a greater tuberosity fracture.3,19 Fracture occurs either due to a shearing mechanism or as a result of avulsion. Shearing injuries are due to the greater tuberosity abutting against the glenoid and eccentric contraction of the rotator cuff during dislocation. In a retrospective review of 103 patients, 57% of the fractures were due to an anterior shoulder dislocation.20
The standard anteroposterior radiographs may underestimate the displacement of the greater tuberosity, with axillary and scapular Y views more indicative. These fractures usually are displaced superiorly and posteriorly due to the pull of the intact attachment of the posterosuperior cuff. A CT scan can better delineate such fractures (Figure 21.4). Glenoid rim fractures are less common in elderly patients, with one study reporting two cases among the 52 patients studied.16
ROTATOR CUFF TEARS
Rotator cuff tears are frequently reported following a traumatic shoulder dislocation in the elderly with the incidence ranging from 34% to 100%.4,6,7,8 and 9 Neviaser et al. reported that all 31 patients in their series, all of whom were more than 35 years of age and were unable to abduct their arm after a dislocation of the shoulder and adequate immobilization, had a rotator cuff tear, with the rate of axillary nerve injury of 7.8%.8
While some authors have found the incidence of cuff tears in patients with shoulder dislocation increases with age,6,21 others have found no such association.4,7,17 A prospective study comparing the incidence of rotator cuff tears found a significant increase in the rate of rotator cuff tears after shoulder dislocation in elderly patients. However, the increase was only of statistical significance among patients below the age of 60 years when compared to patients above 60 years of age.6 There is considerable debate as to whether a rotator cuff tear leads to a dislocation or a dislocation leads to rotator cuff tear. Many biomechanical studies have shown that the cuff is an important dynamic stabilizer of the shoulder and large to massive tears have been demonstrated to cause shoulder instability (Figure 21.5).22
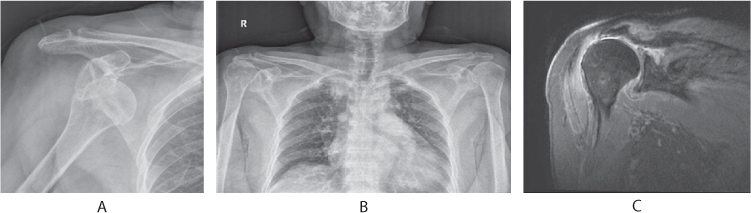
Figure 21.5 An 81-year-old patient who sustained an anterior shoulder dislocation following a fall from standing height (a). The patient was found to have a rotator cuff arthropathy after reduction of the shoulder (b). Coronal MRI shows a massive rotator cuff tear with arthropathy (c). This implies that in essentially asymptomatic patients, a massive cuff tear may predispose the patient to primary dislocation following minimal injury.
A cadaveric study has found that less capsular disruption is needed in the presence of cuff defects to result in a shoulder dislocation.23 Similarly, a large rotator cuff tear is a significant risk factor for redislocation within the first week following reduction of a primary dislocation.24 A study utilizing ultrasound found 15.1% of patients presenting with a shoulder dislocation have chronic tears that were large to massive in size.6 Similarly a population based study of the prevalence of rotator cuff tears found 20.7% of patients had a rotator cuff tear and 16.9% of asymptomatic patients had a cuff tear.25 One study reported no difference in the incidence of cuff tears in patients with pre-existing shoulder symptoms and those with no symptoms prior to dislocation in a study of 95 patients over 60 years of age.4
It might be inferred that large to massive tears predispose to instability, which can lead to shoulder dislocation after a provocative trivial traumatic event. In these patients the degree of trauma required to dislocate the shoulder might be less than required when the cuff is intact. In patients with a degenerate cuff, the shoulder dislocation may be a causative factor in a subsequent tear. It is important to appreciate that rotator cuff tears may be asymptomatic prior to dislocation, with subsequent trauma and dislocation precipitating symptoms in such patients.
TREATMENT
Acute dislocation
After a thorough examination, the shoulder joint should be reduced (Figure 21.6). This can be done under sedation or general anesthesia depending on patient comorbidities and the degree of anticipated difficulty in reduction. Gentle manoeuvring is needed and excessive traction should be avoided. The arm is held close to the shoulder to prevent concomitant fractures of the humerus. A study reported five cases of iatrogenic fracture of the humeral neck after closed reduction of shoulder dislocation under sedation, but with all patients having a greater tuberosity fracture prior to reduction.26
The duration of subsequent immobilization is controversial. Some authors suggest shorter periods of 7–10 days,16 while some suggest 3–4 weeks.4 Longer periods of immobilization may lead to stiffness and difficult rehabilitation, whereas shorter periods may lead to persistent pain that may not allow the patient to follow a rehabilitation protocol. A prudent approach is to immobilize the shoulder for 2 weeks. At the end of 2 weeks, if pain is tolerable, a detailed clinical and neurological examination can be performed, with or without ultrasound as indicated to detect the presence of an associated rotator cuff tear.17,21 In the absence of pain, rehabilitation progressing from passive to active movements and strengthening exercises can be commenced once shoulder motion is restored. If the patient continues to experience pain after 2 weeks, a further 2 weeks of immobilization can be used with rehabilitation initiated after a further thorough evaluation has been performed. If patients are comfortable at the end of 4 weeks then rehabilitation is initiated.
Rotator cuff tears
NON-OPERATIVE
In patients who do not have a rotator cuff tear and respond well to rehabilitation,6,17 conservative treatment has been reported to give good to excellent results in 79% of patients with a shoulder dislocation 2 years following injury (Figure 21.6). The patients without associated rotator cuff tears who were treated conservatively had a better outcome than patients who had surgical repair of a cuff tear.17 Patients with a dislocation of the shoulder who improve with physiotherapy and have no significant rotator cuff tear are ideal candidates for conservative treatment.
Conservative treatment may also be indicated in some patients with shoulder instability and large rotator cuff tears. These include patients with multiple comorbidities and low functional demands where the risk of surgery outweighs the benefit, moribund patients, those who would not be expected to co-operate with a rehabilitation protocol after surgery and those who refuse surgery. Such patients should be counseled to accept the functional disability and avoid provocative activities. Treatment in such patients is aimed at pain relief and achieving a functional range of motion for activities of daily living.
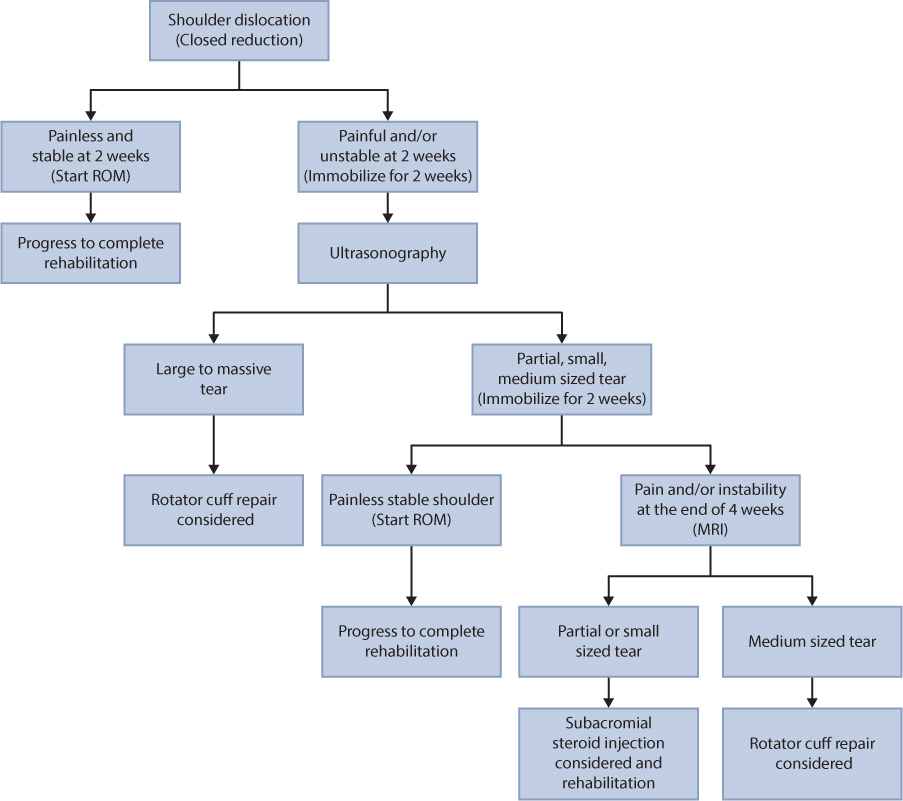
Figure 21.6 Treatment algorithm following a dislocation of the shoulder in elderly patients, with and without rotator cuff tears.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








