5
Medication Therapeutic Categories
Kevin Sneed and Dorraine Reynolds
At the completion of this chapter the reader should be able to do the following:
1. List the basic drug categories in which drugs are classified, including mechanism of action, side effects, and adverse effects
2. Describe the inflammatory process and discuss appropriate pharmacological management of inflammation
3. Describe the key points for using a metered dose inhaler (MDI) and common medications administered with an MDI
4. Describe the indications, contraindications, dosage, and side effects of antihistamines and decongestants and their implications for athletic participation
5. List common narcotic analgesics, and understand the federal restrictions for administration of the drugs and their potential for addiction
6. Appreciate the risks to the athlete participating in athletics while using local anesthetics
7. Understand the actions of antibiotics, including bactericidal and bacteriostatic actions
8. List the common antivirals and antifungals, their indications, contraindications, dosage, and side effects
9. Describe the basic use of anticoagulants in athletics and their mechanism of action, as well as precautions to be observed with the use of this class of drugs
Introduction
This chapter discusses various categories in which drugs are classified. Within each category, the mechanism of action in the body for various drugs is discussed. Side effects, and adverse effects, of drugs are also discussed. For information about pharmacodynamics and pharmacokinetics, please see Chapter 4.
Antiinflammatory Agents
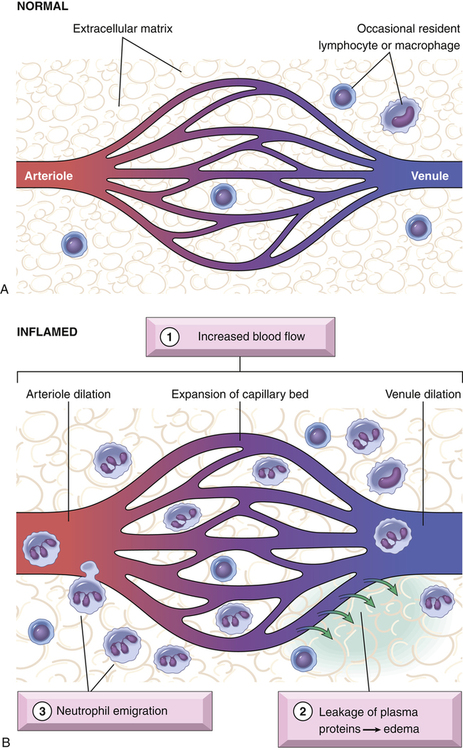
Initially, a vasoconstriction occurs to prevent the loss of blood. This is followed by the release of chemical mediators such as prostaglandins, histamine, leukotrienes, and bradykinins. These mediators cause vasodilation and an increase in cell wall permeability, resulting in fluid escaping from the cells into the interstitial spaces in the quickly progressing inflammatory cascade (Figure 5-1, A and B). Inflammation results in pain, redness, warmth, swelling, and loss of function. Often, conservative management approaches will be used, including cold applications, compression, and resting the affected area. The physician may prescribe antiinflammatory medication to limit the extent of the inflammatory process or cascade. The antiinflammatory medication classifications include nonsteroidal and steroidal antiinflammatory agents.
Nonsteroidal Antiinflammatory Agents
Among the most common medications used in the athletic setting are the NSAIDs (Table 5-1). NSAIDs decrease pain, inflammation, and fever (i.e., antipyretic effect). Many of these drugs are available over the counter, and thus are frequently used by both athletes and the general population (Figure 5-2).
TABLE 5-1
Nonsteroidal Antiinflammatory Drugs (NSAIDs)
| Trade Name(s) | Generic Name | Usual Dose | Maximum Dose per Day |
| Advil, Motrin | Ibuprofen | 400 mg every 4-6 h | 3200 mg |
| Aleve, Anaprox, Naprosyn | Naproxen | 250 mg every 6-8 h | 1250 mg |
| Cataflam, Voltaren | Diclofenac | 50 mg 3 times daily | 200 mg |
| Lodine | Etodolac | 200-400 mg every 6-8 h | 1200 mg |
| Indocin | Indomethacin | 25-50 mg PO or rectally 2 or 3 times daily | 200 mg |
| Orudis, Orudis KT | Ketoprofen | 25-50 mg every 6-8 h | 300 mg |
| Toradol | Ketorolac | IV: 30 mg × 1 dose or 30 mg every 6 h | 120 mg |
| IM: 60 mg × 1 dose or 60 mg every 6 h | 120 mg | ||
| PO: 20 mg initially, then 10 mg every 4-6 h | 40 mg | ||
| Mobic | Meloxicam | 7.5 mg every day | 15 mg |
| Relafen | Nabumetone | 1000-2000 mg every day or twice daily | 2000 mg |
| Daypro | Oxaprozin | 1200 mg every day | 1800 mg |
| Feldene | Piroxicam | 20 mg every day or twice daily | 40 mg |
| Celebrex | Celecoxib | 100-200 mg twice daily | 400 mg |
| Bextra∗ | Valdecoxib | 10-20 mg once or twice daily | 40 mg |
| Vioxx∗ | Rofecoxib | 12.5-50 mg every day | N/A |
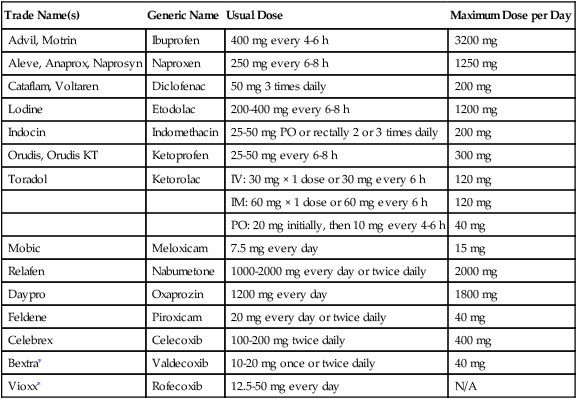
IM, Intramuscular; IV, intravenous; N/A, not applicable; PO, oral (per os).
∗Vioxx and Bextra were removed from the market by their manufacturers, Merck and Pfizer, respectively, because of documented increased links with heart attack and stroke. In February 2005, the FDA ruled that, although there is an increased risk of cardiovascular events in specific populations, Vioxx is still considered an effective and safe medication.
Data from Clinical pharmacology [database online]: Tampa, FL, 2010, Gold Standard, Inc. Available at http://www.goldstandard.com. Accessed May 2010; Facts and comparisons eAnswers [database online]: Conshohocken, PA, 2005, Wolters Kluwer Health. Available at http://efactsweb.com. Accessed May 2010; and Drug information full text [database online]: Wolters Kluwer Health. Available at http://www.ovid.com/site/catalog/DataBase/48.jsp. Accessed May 2010.
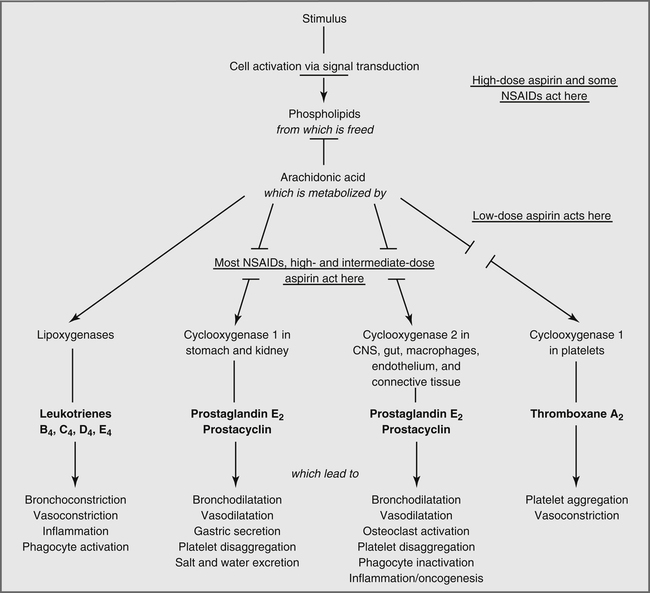
acid (Figure 5-3).1 The COX-2 inhibitor is selective for the COX-2 enzyme. NSAIDs are given primarily via the oral route, although ketorolac (Toradol) may be given orally (per os, PO), intramuscularly (IM), or intravenously (IV). It should be noted that the only COX-2 inhibitor that is currently available is celecoxib (Celebrex). The other COX-2 inhibitors (rofecoxib [Vioxx] and valdecoxib [Bextra]) have been withdrawn from the market.2
Side Effects
Prostaglandins stimulate the secretion of a protective mucosal layer in the gastrointestinal tract. Inhibition of these prostaglandins leads to a breakdown of this mucosal layer, which leads to ulceration. Aspirin, when administered without an enteric coating, buffers, or antacids, causes increased entry of acid into the gastric mucosa, leading to cellular damage at the site of dissolution. As mentioned previously, enteric-coated aspirin will undergo dissolution in the small intestine, thereby avoiding the direct effect on the gastric lining. The administration of NSAIDs with food or milk will minimize adverse gastrointestinal effects. Coadministration of aspirin and other NSAIDs with corticosteroids increases the risk of gastrointestinal lesions. Alcohol consumption concomitant with the intake of aspirin or NSAIDs may put patients at increased risk of upper gastrointestinal bleeding, a risk that is elevated by increasing alcohol consumption.3,4
Aspirin, salicylates, and to a much lesser extent NSAIDs have hematological effects that must be considered in the athlete. Aspirin inhibits platelet aggregation and decreases hepatic synthesis of blood coagulation factors. At normal doses of up to 6 g/day, aspirin rarely increases the prothrombin time (PT), the time it takes blood to clot, by more than 2 to 3 seconds. Higher doses, fever, and increased metabolic rate may cause greater increases in PT. For athletes in contact sports, especially when the likelihood of head trauma is high, aspirin may not be a good therapeutic choice. Head trauma occurring in an athlete in an anticoagulated state might increase the risk or extent of intracranial bleeding. Research is mixed on the probability of aspirin causing increased intracranial bleeding after head trauma for the patient who is receiving low-dose aspirin therapy.5
Other NSAIDs, such as ibuprofen, inhibit platelet aggregation but to a lesser extent than aspirin. This has raised some concern that NSAIDs not be used by athletes in sports that may put the athletes at risk for head trauma. Physicians have various views on this subject.5 Health care providers working with athletes in contact or collision sports have a responsibility to know and uphold the views of the team physicians on this subject.
The safety of the COX-2 inhibitors has been questioned with the industry withdrawal of rofecoxib (Vioxx) and valdecoxib (Bextra), due to increased risk of cardiovascular events.6–8 At this time, celecoxib (Celebrex) remains the only COX-2 inhibitor available for use by patients. Previous meta-analyses revealed that all nonselective NSAIDs may have increased cardiovascular risks, although the risks are relatively low when compared with the number of patients taking these medications. The athletic trainer and general consumer must remember that along with the benefits, potential adverse effects occur with any drug. Individual patient needs and risk factors must be considered to make the best drug therapy choices. The lowest possible effective dose should always be used to minimize the chance of adverse drug events.
Interactions
Because many NSAIDs are readily available over the counter, the athlete may be tempted to take NSAIDs such as ibuprofen with acetaminophen.9 These two drugs have different mechanisms of action, and therefore it is safe to combine them if the maximum dosage of over-the-counter NSAIDs is not providing enough analgesia. The athletic trainer is strongly encouraged to monitor the medication intake of all athletes, regardless of whether the medication is available without a prescription.10 If the athlete’s discomfort is not relieved, the team physician should be consulted about the condition. The athletic trainer also needs to educate the athlete that many products contain the same active ingredients and therefore care must be taken when taking medications of any kind.
Steroidal Antiinflammatory Agents: Corticosteroids
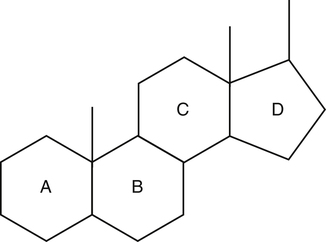
The adrenal cortex (part of the adrenal glands, located above the kidneys) produces two classes of steroids: corticosteroids and androgens (anabolic steroids). Both corticosteroids and androgenic steroids have similar chemical structures (Figure 5-4), but their pharmacological actions are very different from each other. Androgens are typically recognized as male hormones (i.e., testosterone), although there is a subtle role for these hormones in women. Corticosteroids serve as metabolic and electrolyte regulators of organ systems in the human body. The corticosteroids are further divided into two subclasses: the glucocorticosteroids and the mineralocorticosteroids. The glucocorticosteroids are considered to regulate carbohydrate metabolism, and the mineralocorticosteroids regulate electrolyte balance.1,11 Glucocorticoid actions decrease inflammation, cause immune system suppression, and stimulate gluconeogenesis. They also promote protein catabolism, redistribute peripheral fat to central areas, decrease intestinal absorption of calcium, and increase renal excretion of calcium. Mineralocorticoid actions affect electrolytes and fluid balance, with the net effect being sodium and fluid retention, and potassium and hydrogen excretion. The pharmacological effects of the corticosteroids are most likely caused by their complex enzymatic influence on various organ systems.
For the athletic health care provider, the most important effects of corticosteroids are their antiinflammatory properties, which are beneficial in the treatment of inflammatory joint and connective tissue injuries and environmental allergies (Table 5-2).
TABLE 5-2
| Trade Name(s) | Generic Name | Route | Usual Dose/Dosage |
| Cortef, Solu-Cortef | Hydrocortisone | Intraarticular or intralesional | 5-75 mg |
| IM or IV | 15-240 mg/d | ||
| PO | 20-240 mg/d | ||
| Rectal | 100 mg/d | ||
| Deltasone, Liquid Pred, Orasone | Prednisone | PO | 5-60 mg/d |
| Various | Prednisolone | IM, IV, or intraarticular or soft tissue | 4-60 mg |
| PO | 5-60 mg/d | ||
| Medrol, Solu-Medrol | Methylprednisolone | IM | 80-120 mg |
| Intraarticular and soft tissue | 4-80 mg | ||
| Dermatological | 40-120 mg/wk | ||
| IV | 10-40 mg | ||
| PO | 4-48 mg/d | ||
| Kenalog, Kenacort, Aristocort | Triamcinolone | IM | 25-60 mg/d |
| Intraarticular or intrabursal | 2.5-40 mg/d | ||
| Intradermal | 1 mg per site | ||
| Intralesional or sublesional | 5-48 mg | ||
| PO | 8-16 mg/d | ||
| Decadron | Dexamethasone | IM | 4-8 mg |
| Intraarticular or soft tissue | 4-16 mg | ||
| PO | 0.75-9 mg/d |
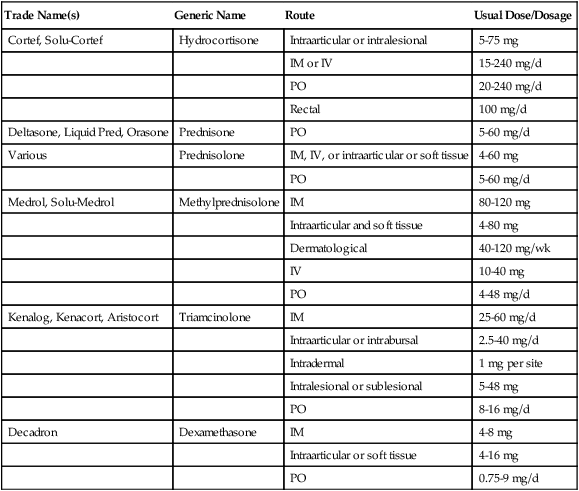
IM, Intramuscular; IV, intravenous; PO, oral (per os).
Data from Clinical pharmacology [database online]: Tampa, FL, 2010, Gold Standard, Inc. Available at http://www. ndard.com. Accessed May 2010; Facts and comparisons eAnswers [database online]: Conshohocken, PA, 2005, Wolters Kluwer Health. Available at http://efactsweb.com. Accessed May 2010; and Drug information full text [database online]: Wolters Kluwer Health. Available at http://www.ovid.com/site/catalog/DataBase/48.jsp. Accessed May 2010.
Pharmacological Treatment Options: Corticosteroids
Most corticosteroids used to treat inflammatory joint injuries are administered in one of three ways: by intrasynovial injection, intraarticular injection, or iontophoresis. It is not atypical that these injections be accompanied by a short-acting anesthetic such as lidocaine (Xylocaine). Injectable corticosteroids are typically used after more conservative treatments, such as cold compression therapy, have failed and the inflammatory process can be localized to a small area.12 Iontophoresis involves the use of mild electrical charges applied to topical adhesive patches that contain medication to propel medication through the dermis. This noninvasive procedure has become a popular corticosteroid option for the treatment of injuries in athletes, but debate remains about whether iontophoresis is as effective as intraarticular injection.13–15
The immunosuppressive properties of corticosteroids make them invaluable in the treatment of allergies and inflammatory joint conditions. Prednisone and methylprednisolone are the oral agents used most frequently in the treatment of allergic reactions and acute joint inflammation. Typically a large dose (equivalent to approximately 30-60 mg of prednisone) will be given on the first day of treatment and then the dose will be tapered by 5 to 10 mg/day over subsequent treatment days . The initial dose and subsequent doses may be given as a single daily dose or as divided doses. Both prednisone and methylprednisolone are supplied as a convenient dose pack consisting of tablets in a daily blister pack with complete instructions for appropriately taking the medication. For inflammatory conditions of a joint, the steroid taper phase will usually be followed by a course of a nonsteroidal antiinflammatory drug if necessary, such as ibuprofen or celecoxib (a COX-2 inhibitor).1,2 If the condition being treated is exacerbated during the taper, then the dose of steroid will be increased and maintained for a short time before the taper is restarted.
Additional Pharmacological Uses: Corticosteroids
Inhaled Corticosteroids
Inhaled corticosteroids are used in the treatment of asthma, and are dispensed by metered-dose inhalers (MDIs). Intranasal steroids are also used in the treatment of allergic rhinitis or allergies. (Table 5-3). These steroids are manufactured for oral inhalers and as intranasal metered-dose sprays to provide a local antiinflammatory effect and to reduce the effects of environmental allergens through immunosuppressive mechanisms. Inhaled corticosteroids provide a local antiinflammatory effect in the airways. They should never be used for acute exacerbations of asthma because they do not cause immediate bronchodilation.
TABLE 5-3
| Trade Name(s) | Generic Name |
| AeroBid | Flunisolide |
| Fluticasone Proprionate | |
| Azmacort | Triamcinolone |
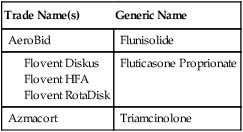
Modified from Silvestri LA: Comprehensive review for the NCLEX-RN examination, ed 4, Saunders, 2007.
Side Effects
The side effects of corticosteroids depend on the dose and the route of administration. They are minimal with intrasynovial injection, intraarticular injection, intranasal application, inhalation, or short-term therapy. However, tendon ruptures have occurred in patients receiving corticosteroid injections. The Achilles tendon is especially susceptible to this effect. Research indicates that repeated short courses, intranasal corticosteroids, and inhaled corticosteroids may also cause decreased bone density and osteoporosis.16,17
In addition, high doses or prolonged use of corticosteroids used for treatment of systemic inflammatory or autoimmune diseases, such as lupus, multiple sclerosis, or inflammatory bowel syndromes (e.g., Crohn’s disease), may produce devastating side effects. These may include changes in physical appearance caused by changes in fat deposition, adrenal suppression, cataracts, or peptic ulcers. Long-term use of corticosteroids may lead to decreased bone density and osteoporosis.16
Corticosteroids, including those administered intranasally, may cause a reduction in growth velocity in pediatric patients but have no impact on final adult height.16 The growth of pediatric patients receiving corticosteroids should be monitored routinely. In addition, in order to prevent decreases in bone density, children older than 11 years of age should receive calcium, 1500 mg/day, and vitamin D, 800 IU/day, throughout the course of treatment with corticosteroids.17
Repeated intrasynovial or intraarticular injection will not result in any systemic effects but will cause damage to the joint. Intraarticular injections in major weight-bearing joints are not recommended because of the potential softening of joint cartilage.17 Even after a single injection, if the joint is not allowed proper time to heal, damage may occur. Consideration of the potential risks to the joint must be considered and discussed with the patient before intraarticular injection.
Intranasal corticosteroids are generally very well tolerated. The most common side effects are nasal irritation, pharyngeal irritation, and dryness. Similarly, the most common side effects of inhaled corticosteroids are hoarseness, dry mouth, sore throat, and oropharyngeal fungal infections, such as Candida albicans or Aspergillus niger.2 After using an inhaled corticosteroid, the mouth should always be rinsed to prevent oral fungal infections.
Additional Respiratory Pharmacological Options
Bronchodilators
Bronchodilators are β-adrenergic agonists (Table 5-4). These agents stimulate the β-adrenergic receptors in the bronchi and bronchioles to cause a widening of these airways and allow for improved airflow. In the athlete, exercise-induced bronchospasm (EIB) is the most common cause of airway constriction requiring treatment with bronchodilators.
TABLE 5-4
| Drug | Administration |
| Albuterol (Ventolin, Proventil) | Metered-dose inhaler, oral tablets, oral solution, solution for nebulization |
| Levalbuterol (Xopenex) | Solution for nebulization |
| Racemic epinephrine (S2 Inhalant) | Solution for nebulization |
Data from Clinical pharmacology [database online]: Tampa, FL, 2010, Gold Standard, Inc. Available at http://www. ndard.com. Accessed May 2010; Facts and comparisons eAnswers [database online]: Conshohocken, PA, 2005, Wolters Kluwer Health. Available at http://efactsweb.com. Accessed May 2010; and Drug information full text [database online]: Wolters Kluwer Health. Available at http://www.ovid.com/site/catalog/DataBase/48.jsp. Accessed May 2010.
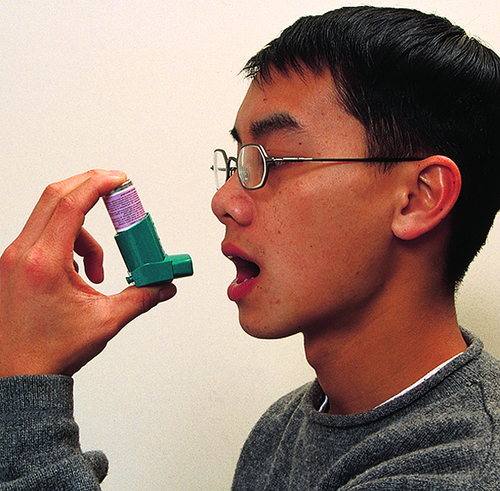
Proper technique for using an inhaler is discussed in Box 5-1. A spacer that holds the puff of medicine between the inhaler device and the athlete can be used to increase the ease of use. When a spacer is used, the actuation of the inhaler does not have to be timed to the inhalation of the drug; the inhaler delivers the drug into the spacer (Figure 5-5). The athlete then inhales the drug slowly and often more completely through the spacer as a separate step.
Nebulizers are machines that use air pressure to aerosolize a drug and then deliver the quickest onset and maximized amount of drug. They are expensive and bulky to transport, but the drug can be delivered simply by placing a mask over the mouth and nose (Figure 5-6).
Side Effects
The main adverse effects of bronchodilators are tremor, nervousness, dizziness, headache, nausea, and tachycardia. A paradoxical bronchospasm also has been reported in 8% of individuals using bronchodilators.18,19 It is usually associated with the first use of a new MDI canister and may be related to exposure to the propellant. To avoid this reaction, a new MDI can be actuated into the air a few times before its first use. Nebulized albuterol caused coughing in 4% of individuals in various clinical trials. Side effects that occurred in less than 3% of individuals but that may be significant in the athlete include muscle cramping, muscle spasm, and dilated pupils.18
Leukotriene-modifying Respiratory Medications
Leukotriene-modifying medications are either competitive antagonists of leukotriene receptors or inhibitors of leukotriene synthesis20. Leukotriene receptor antagonists inhibit the action of leukotrienes, which are potent constrictors of bronchial smooth muscle. These medications include zafirlukast (Accolate) and montelukast (Singulair). Leukotriene inhibitors prevent the formation of 5-lipoxygenase, which catalyzes the formation of leukotrienes from arachidonic acid. The medication zileuton (Zyflo) represents this class of medication. Both classes of leukotriene-modifying medications display efficacy in the treatment of asthma,21 but are generally not effective for the treatment of EIB,21 and are not replacements for short-acting β-agonists when treating EIB.
Anticholinergic Agents
Bronchodilation is achieved with anticholinergic medications used for the treatment of asthma. These medications relax bronchial smooth muscle through competitive antagonism of muscarinic receptors present in the lungs. There are short-acting (ipratropium) and long-acting (tiotropium) respiratory anticholinergics, which are both effective for asthma and chronic obstructive pulmonary disease (COPD). In some athletes, these agents may be effective for prevention of EIB when used before exercise.22
Antihistamines
The histamine antagonists are classified into two groups on the basis of their likelihood of causing sedation. The first-generation, or sedating, antihistamines are older agents with a much higher incidence of anticholinergic adverse effects, including sedation (Table 5-5). They are used in the treatment of seasonal allergies and some cold symptoms. The sedating properties associated with these drugs also make them useful in the short-term treatment of insomnia. In addition, some antihistamines, such as meclizine (Antivert) and hydroxyzine (Atarax, Vistaril), are used in the treatment of nausea, vertigo, motion sickness, and hives. Sedating antihistamines are commonly used to treat allergy symptoms associated with seasonal allergies and are usually formulated in combination with decongestants.
TABLE 5-5
| Antihistamine (Sedating) | Trade Name(s) | Usual Adult Dosage |
| Azatadine | Optimine, 1 mg | 1-2 mg twice daily |
| Rynatan and Trinalin, 1 mg, with pseudoephedrine, 120 mg | ||
| Brompheniramine | Numerous | 4 mg every 4 h or 6-12 mg every 12 h (extended release) |
| Dexbrompheniramine with pseudoephedrine | Drixoral | 6 mg every 12 h (extended release) |
| Carbinoxamine with pseudoephedrine | Rondec, Cardec | 4 mg 4 times daily or 8 mg every 12 h (extended release) |
| Chlorpheniramine | Chlor-Trimeton, numerous others | 4 mg every 4-6 h or 8-12 mg twice daily (extended release) or 16 mg once daily (extended release) |
| Clemastine | Tavist | 1.34 mg every 12 h |
| Diphenhydramine | Benadryl, various others | 25-50 mg every 4-6 h |
| Promethazine | Phenergan | 6.25 mg every 4-6 h |
| Triprolidine | Actifed | 2.5 mg every 4-6 h |
Data from Clinical pharmacology [database online]: Tampa, FL, 2010, Gold Standard, Inc. Available at http://www. ndard.com. Accessed May 2010; Facts and comparisons eAnswers [database online]: Conshohocken, PA, 2005, Wolters Kluwer Health. Available at http://efactsweb.com. Accessed May 2010; and Drug information full text [database online]: Wolters Kluwer Health. Available at http://www.ovid.com/site/catalog/DataBase/48.jsp. Accessed May 2010.
Nonsedating, or second-generation, antihistamines are used to treat and prevent seasonal allergies and to treat chronic idiopathic urticaria. These antihistamines are often the drug of choice for the athlete because they are nonsedating (Table 5-6). The nonsedating antihistamines currently available by prescription are fexofenadine (Allegra) and desloratadine (Clarinex). Cetirizine (Zyrtec) and loratadine (Claritin, Alavert) are now available as over-the-counter products. Cetirizine and fexofenadine are also formulated in combination with the decongestant pseudoephedrine (Zyrtec-D, Allegra-D).
TABLE 5-6
| Antihistamine (Nonsedating) | Trade Name(s) | Usual Adult Dosage | Drug Interactions | Adverse Effects |
| Cetirizine∗ | Zyrtec | 5-10 mg once daily | Somnolence, fatigue, dizziness, dry mouth | |
| Desloratadine | Clarinex, Clarinex RediTabs | 5 mg daily | ||
| Fexofenadine | Allegra | 60 mg twice daily or 180 mg once daily | Aluminum- and magnesium-containing antacids decrease absorption and peak plasma levels; do not take fexofenadine within 2 h of antacids | Headache, insomnia, dizziness, back pain |
| Loratadine∗ | Claritin, Alavert | 10 mg once daily | Headache, sedation, insomnia, nervousness, dry mouth, abdominal pain |
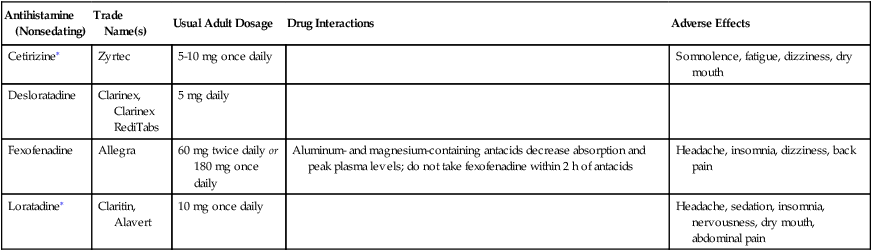
Data from Clinical pharmacology [database online]: Tampa, FL, 2010, Gold Standard, Inc. Available at http://www. ndard.com. Accessed May 2010; Facts and comparisons eAnswers [database online]: Conshohocken, PA, 2005, Wolters Kluwer Health. Available at http://efactsweb.com. Accessed May 2010; and Drug information full text [database online]: Wolters Kluwer Health. Available at http://www.ovid.com/site/catalog/DataBase/48.jsp. Accessed May 2010.
The adverse effects most often associated with the first-generation sedating antihistamines are those caused by central nervous system (CNS) depression, such as drowsiness, muscular weakness, and dizziness. Therefore antihistamines should be used with caution in athletes participating in events where coordination and alertness are needed to prevent injury. The incidence of injury may be increased and performance decreased even with a mild sedative effect from the antihistamine. Anyone taking antihistamines should avoid alcohol intake because of the additive effect on CNS depression.2
Additional adverse effects seen with first-generation antihistamines may be gastrointestinal in nature and include nausea, vomiting, diarrhea, and constipation. These antihistamines also cause anticholinergic side effects, such as dry mouth, blurred vision, urinary retention, impotence, nervousness, and irritability.1
Antihistamines must be used with caution in individuals with hypertension and hyperthyroidism (see Chapters 8 and 14). Because there is some controversy over the potential for antihistamines to induce asthma attacks by virtue of their drying effect on bronchial tissues, antihistamines are contraindicated in individuals who experience acute asthmatic attacks. The drug interactions of the sedating antihistamines are primarily with other CNS depressants, which will cause an additive CNS depressant effect.
Decongestants
Decongestants are medications that stimulate primarily the α-adrenergic receptors and to a lesser extent the β-adrenergic receptors (Table 5-7). The beneficial result of this α-adrenergic stimulation is vasoconstriction in the nasal mucosa, which shrinks swollen nasal passages and thereby relieves nasal congestion. The decongestants are used orally either alone or in combination with other agents used to treat cold and allergy symptoms (e.g., antihistamines).
TABLE 5-7
| Generic Name | Trade Name(s) | Usual Adult Dosage | Adverse Effects |
| Naphazoline | Privine | 2 drops every 3-6 h | Rebound congestion, burning, stinging, nasal dryness, sneezing, headache, hypertension, palpitations, tachycardia, reflex bradycardia, nervousness, nausea, dizziness, weakness, sweating |
| Oxymetazoline | 2-3 drops/sprays every 10-12 h for no more than 3 d | Rebound congestion, burning, stinging, rhinorrhea, nasal dryness, sneezing, hypertension, nervousness, nausea, dizziness, headache, insomnia, palpitations, tachycardia, reflex bradycardia | |
| Phenylephrine | 2-3 drops or 1-3 sprays every 4 h | Rebound congestion, burning, stinging, sneezing, rhinorrhea, nasal dryness, palpitation, tachycardia, PVCs, headache, pallor, tremors, sweating, hypertension, nausea, dizziness, nervousness | |
| Propylhexedrine | Benzedrex | 2 inhalations every 2 h | Rebound congestion, burning, stinging, nasal dryness, sneezing, headache, hypertension, nervousness, tachycardia |
| Tetrahydrozoline | Tyzine | 2-4 drops/sprays every 4-6 h | Rebound congestion, burning, stinging, nasal dryness, sneezing, headache, hypertension, weakness, sweating, palpitation, tremor |
| Xylometazoline | Otrivin | 2-3 drops/sprays every 8-10 h for no more than 3-5 d | Rebound congestion, burning, stinging, nasal dryness, sneezing, hypertension, nervousness, nausea, dizziness, headache, insomnia, palpitations, tachycardia, arrhythmia |
| Ophthalmic decongestants | |||
| Naphazoline | 1-3 drops every 3-4 h | Blurred vision, mild stinging or irritation, pupil dilation, headache, hypertension, palpitations, tachycardia, reflex bradycardia, nervousness, nausea, dizziness, weakness, sweating | |
| Oxymetazoline | 1-2 drops every 6 h | ||
| Phenylephrine | 1-2 drops every 3-4 h | Headache, blurred vision, irritation, pupil dilation, palpitation, tachycardia, PVCs, headache, pallor, tremors, sweating, hypertension, nausea, dizziness, nervousness | |
| Tetrahydrozoline | 1-2 drops up to 4 times daily | Irritation, blurred vision, pupil dilation, rebound congestion, headache, hypertension, weakness, sweating, palpitation, tremor | |
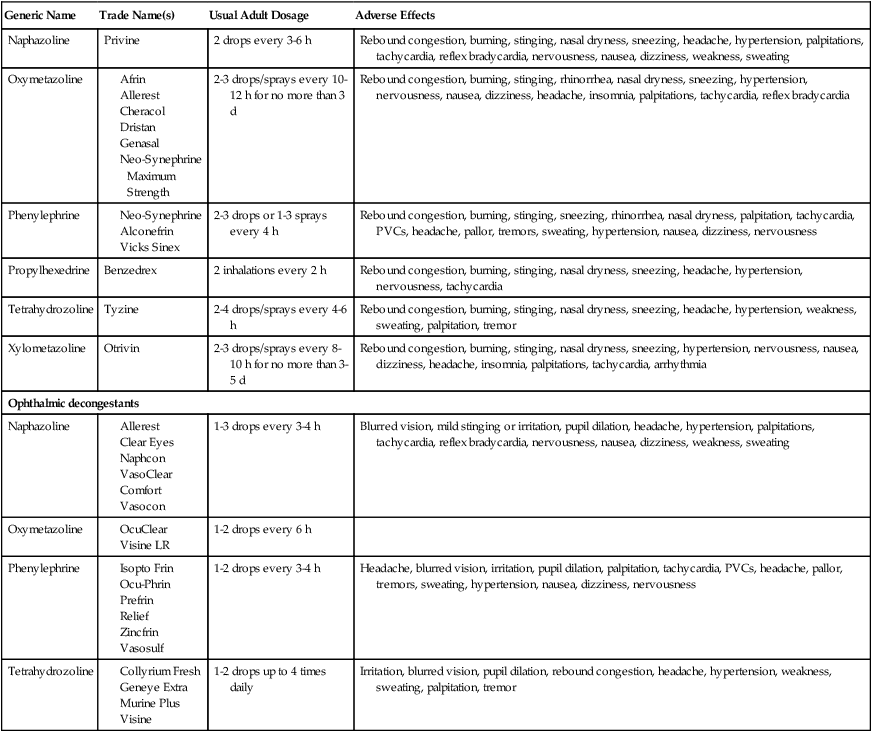
PVCs, Premature ventricular contractions.
Data from Clinical pharmacology [database online]: Tampa, FL, 2010, Gold Standard, Inc. Available at http://www. ndard.com. Accessed May 2010; Facts and comparisons eAnswers [database online]: Conshohocken, PA, 2005, Wolters Kluwer Health. Available at http://efactsweb.com. Accessed May 2010; and Drug information full text [database online]: Wolters Kluwer Health. Available at http://www.ovid.com/site/catalog/DataBase/48.jsp. Accessed May 2010.
Pseudoephedrine (Sudafed) is the oral decongestant most commonly used alone or in combination products. Pseudoephedrine is a naturally occurring substance found in plants of the genus Ephedra and is an isomer of ephedrine. The usual adult dose of pseudoephedrine is 30 to 60 mg every 4 to 6 hours. Sustained-release products of pseudoephedrine are available as 120 mg tablets given every 12 hours and 240 mg tablets given every 24 hours.2 The side effects associated with the use of pseudoephedrine include mild CNS stimulation such as nervousness, dizziness, weakness, insomnia, and headache. Whereas pseudoephedrine causes minimal blood pressure changes in individuals with normal blood pressure, it should be used with caution in individuals with high blood pressure because α-adrenergic stimulation causes vasoconstriction and may raise blood pressure.
Pseudoephedrine can be used to make methamphetamine, a CNS stimulant with high addictive potential. For this reason, federal law limits the quantity of pseudoephedrine that can be sold by retail distributors. However, it is important that the athletic trainer be aware that the oral decongestants pseudoephedrine and phenylephrine are no longer listed in the National Collegiate Athletic Association (NCAA) bylaws (Section 31.2.3) as banned drugs.23 It should be noted that other CNS stimulants remain on the banned substances list.23
Phenylephrine (Neo-Synephrine) is used as a topical decongestant in nasal drops and sprays. It, too, is no longer listed on the NCAA list of banned drugs.23 Phenylephrine nasal drops or sprays for adults are available as 0.25% or 0.5% solutions that are applied to the nasal mucosa every 4 to 6 hours. Adverse effects of phenylephrine nasal solutions include transient burning, stinging, sneezing, rhinitis, and nasal dryness. Prolonged use of phenylephrine nasal solutions should be avoided because it may result in chronic or rebound swelling of the nasal mucosa, which resolves within 1 week of discontinuing the drug.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree