15
Infectious Diseases
At the completion of this chapter the reader should be able to do the following:
1. Explain common infection transmission routes and their prevention
2. Justify the importance of maintaining immunization against those diseases for which there is vaccine
3. Describe the reporting levels of communicable diseases
4. List the signs and symptoms of common infectious diseases
5. Recognize common childhood diseases and how to prevent them
6. Demonstrate universal precautions for the prevention and transmission of infectious disease
Introduction
In 2007, there were 14,000 deaths in the United States attributed to infectious disease.1 Nearly every chapter in this text addresses an infectious condition: sinusitis in the chapter on disorders of the ear, nose, throat; urinary tract infection in the chapter on genitourinary and gynecological disorders; and pneumonia in the chapter on respiratory disorders. This chapter provides an overview of the infectious disease process that includes common transmission mechanisms and routes as well as preventive measures that can be used to stop the infectious cycle and protect athletes and the population at large. The conditions discussed in this chapter encompass many common childhood diseases, in addition to hepatitis and streptococcal, staphylococcal, as well as neurological infections. Sexually transmitted infections (STIs) are discussed in Chapter 10).
Transmission
Most infections arise from one of four transmission routes: airborne, direct contact, bloodborne, or water- and foodborne.2–6 Infectious organisms from someone who is sick can be spread via these pathways, and sanitary precautions are the most important line of defense in retarding many illnesses found in otherwise healthy adults. Healthy humans live in harmony with microbial flora that protect against the invasion of disease-causing microorganisms.7 These flora reside in specific organs of the body, such as the skin, respiratory system, and gastrointestinal tract, and provide assistance in safeguarding these organs’ natural environment. Certain medications can disrupt this balance, as can repeated exposure to infectious organisms in an overtrained athlete. Many flora that protect humans can also do a turnabout and invade their hosts given certain conditions. Specific disease transmission routes are discussed within the appropriate section on the disorder.
Prevention
Vaccination
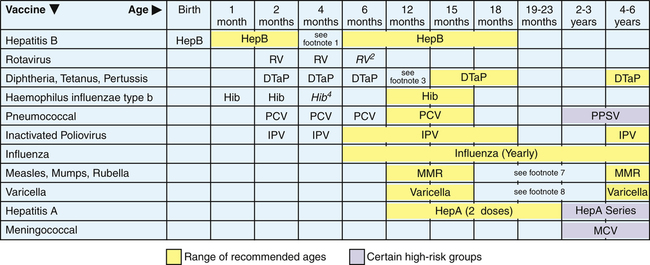
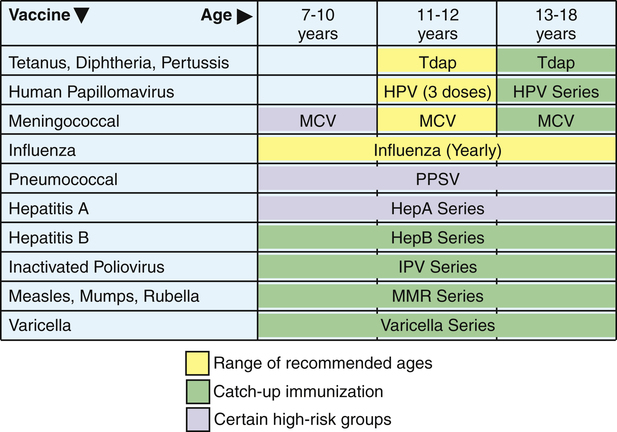
Practicing universal precautions and sanitation measures (see Chapter 1) can prevent the transmission of most infectious diseases. In addition, immunization has deterred the spread of many adult and childhood diseases, such as the MMR vaccine for measles, mumps, and rubella.
that may prevent future cervical cancer that can be caused by HPV. A varicella (chicken pox) vaccine was approved in 1995, and studies indicate that a two-dose series was warranted in order for the vaccine to truly be effective. It was recommended in 1996 that all children receive the two-dose immunization for full immunity.7,8 Adults are not removed from immunizations, as in addition to pneumonia vaccine for those over 65 years of age, and annual influenza protection, the Food and Drug Administration (FDA) recommended in 2008 that adults over the age of 60 years be vaccinated to prevent varicella-zoster (shingles).9,10
Some adults missed the window of opportunity for certain immunizations because they were born before these immunizations became available. For example, an effective vaccine for hepatitis B virus (HBV) was not established until 1982. Immunization against HPV is also an example, as 13- to 26-year-old females are encouraged to complete the series if they missed their window of opportunity.11 Adults who were not immunized as children and who have no history of a particular disease should be vaccinated as adults, especially if they work in areas where they would be susceptible to the disease.11 Figures 15-1 and 15-2 provide the recommended schedules for vaccination for children and adults.
Children are no longer routinely vaccinated for smallpox because this disease has not been found in humans for more than a generation. Other communicable diseases, such as typhus, botulism, Escherichia coli, polio, and anthrax, are not common but are extremely dangerous if contracted.12 The danger with rare and extinct diseases is that they do still live in some laboratories, and recent events have made many people aware that releasing these organisms could initiate global germ warfare. Because few individuals are currently vaccinated against these dormant, yet deadly, diseases, their rapid spread is plausible.12
Because of the diligence in immunization, U.S. public health officials established a goal via Healthy People 2010 to eliminate diphtheria, hepatitis B, measles, mumps, polio, rubella, varicella, and tetanus by the year 2010. However, it has been discovered that immunization status after vaccination is not always guaranteed. Of the 6584 people who contracted mumps in the outbreak of 2006, 77% to 97% of the college students who acquired the illness had received the required two-dose MMR (mumps/measles/rubella) vaccine shots.13,14
With prevention being paramount, health histories typically include immunization records. However, in a study of the immune status of first-year medical students in New South Wales, Australia, it was discovered that immunity corresponded poorly with the self-reported history.15 Tests were done to determine the students’ antibody titers to certain vaccine-preventable diseases; results showed that their antibody titers were insufficient to protect them from future infection. Another article provided evidence for what many parents already know: that giving an infant acetaminophen (Tylenol) to reduce fever caused by an immunization actually reduces the effect of the vaccine.16 This research may shed light on why so many previously immunized people have had less than the desired effect of the vaccine later in life.
Although there may be little debate over the suggested vaccines among health care providers, not all agencies have adopted minimal standards for immunization, leaving it to institutional autonomy or state authority. Even the Commission on Accreditation of Athletic Training Education (CAATE) standards only call for “an immunization review” for athletic training students; they do not articulate from what diseases the students should be immune.17
Annual Immunization
An annual influenza shot for those working in the field of health care, older adults, children, and those with weakened immune systems has become an important health care benchmark each fall.9 It should be noted that the seasonal influenza shot is usually targeted for a specific type of influenza, and does not provide global immunity for all types of influenza. Typically, influenza A and B cause seasonal epidemics in the winter months in the United States.18 Each of these flus has subtypes and a slightly different physiological makeup. Vaccines are created annually to deter the viruses, but these illnesses have been known to alter themselves genetically to better fit a host. When this occurs, the current vaccine is not effective in preventing the new strain. The two most common influenza vaccines are the trivalent inactivated influenza vaccine (TIV) and the live intranasal influenza vaccine (LAIV). The former is administered via an intramuscular injection, whereas the LAIV is a nasal spray that provides a small amount of a live virus. The “FluMist” nasal spray has some contraindications, as those with chronic respiratory conditions or sinusitis must receive the injectable version instead, because of potential complications from the inhalation of the live virus. The live virus usually creates some flulike symptoms within a few days of administration, whereas the injected variety does not. Because seasonal influenza most often strikes in the winter months (typically between October and March), it is recommended that patients receive their annual dose in October to provide full-season coverage that lasts through mid-spring.
As previously mentioned, airborne and direct contact are two methods of infecting others with communicable diseases. The close surroundings of athletic huddles, time-outs, locker rooms, and team buses afford these two methods many opportunities to spread infections among team members.2,19 Numerous precautions, however, can help prevent infections from being transmitted. The basic practices of personal hygiene are underappreciated in the fight against the spread of disease. Simple habits of frequent hand washing (Figure 15-3), covering one’s mouth or nose when coughing or sneezing, showering with quality antibacterial soap, and protecting the skin, including good foot care, are all examples of personal responsibility in hygiene.19 Athletes with infections are isolated while contagious, and any equipment or clothing that they have worn is sanitized before the next use.
Methods of protection against disease that could affect the whole team include safeguarding the water source and containers, and sanitizing surfaces that athletes have contact with, such as treatment tables, mats, and rehabilitation equipment. Certain states have regulations about the type of hose that may be used to draw potable (i.e., drinkable) water. These regulations may be found at the particular state health website or U.S. Occupational Safety and Health Administration (OSHA) website. When sanitizing equipment, surfaces, and water containers such as coolers, ice containers, and water bottles, a solution of 1 part bleach to 9 parts water is effective as a germicidal agent.19
Reporting Communicable Diseases
The health care provider has a legal obligation to report certain medical conditions to the public health authorities, such as some sexually transmitted infections (STIs) or tuberculosis. The rationale behind reporting these conditions is to protect the public from an outbreak of the disease; the courts have ruled that for certain medical conditions, the risks of exposure outweigh the patient’s right to privacy (Box 15-1). Local, state, and national agencies review the lists of reportable diseases, and report them to the proper authority when diagnosed by physicians or in laboratories.20
A five-class reporting system for communicable diseases is used in the United States. When a physician has confirmed a certain infectious disease, the disease but not the person is reported to the correct state or federal agency.20 On rare occasions, such as with an STI, the infectious individual is reported, and any partners who may have been infected are contacted.
Reporting Epidemics
There are five identified classes for reporting these diseases:
Class 1: Case report universally required by international health regulations or as a disease under surveillance by the World Health Organization (WHO, Geneva, Switzerland). These comprise the internationally quarantinable diseases such as plague, cholera, and yellow fever. The specific diseases in this category were first identified in 1969 and updated as recently as 2005 before distribution to the World Health Assembly.
Diseases listed in class 1 are to be immediately reported to the WHO because they are considered of urgent international public health importance. A subcategory of class 1 includes louse-borne typhus fever, paralytic poliomyelitis, malaria, and influenza. These diseases must be reported as urgent to state or federal agencies by fax, e-mail, or telephone with a subsequent daily or weekly update as dictated by law.
Class 2: Case report regularly required wherever the disease occurs. The first subcategory includes diseases such as typhoid fever, diphtheria, and agents used by bioterrorists, including anthrax, botulism, and smallpox. The second subcategory comprises diseases that require a less urgent form of notification, within 1 week as opposed to a same-day report. An example of a disease in this category is leprosy.
Class 3: Diseases selectively reportable in recognized endemic areas. These include three subcategories to specific regions, counties, or states that may have a particular proclivity for an infectious disease. Many states have no diseases in class 3.
Class 4: Obligatory report of epidemics but no case report required. Class 4 diseases are to be reported immediately and include staphylococcal foodborne intoxication.
Class 5: Official report not ordinarily required for sporadic and uncommon infectious diseases, as well as those having no practical measures for containment, such as the common cold and sinusitis.
Pandemic
The term pandemic has been coined to reflect an illness that quite literally affects “all people,” as the Greek root of the word indicates.21 Pandemics in modern history include human immunodeficiency virus (HIV) and the “swine” flu (H1N1). Pandemics are infectious diseases that cross continents; and seasonal flus are not included in these descriptors. Historically significant pandemics include cholera, typhus, smallpox, measles, tuberculosis, leprosy, malaria, and yellow fever.21 A disease must meet three specific criteria in order to be termed “pandemic” by the WHO22:
Pathological Conditions
Influenza
In the United States, seasonal influenza has caused approximately 36,000 deaths and 200,000 hospitalizations each year.23 Ninety percent of the deaths and 60% of the hospitalizations are of adults over the age of 65 years. In 2008-2009 approximately 83% of the U.S. population met the criteria to undergo vaccination, yet less than 40% received the influenza vaccine.24
Another influenza variant that has surfaced periodically throughout the world is swine flu. Originally detected in 1976, it was transmitted from pigs to humans; and in 2009 another outbreak occurred, this time attributed to the H1N1 influenza virus. H1N1 was labeled as a pandemic by the WHO in June 2009 and by July there were more than 94,000 confirmed cases in more than 100 countries.25 H1N1 is different enough from the 1976 strain of swine flu that those who were vaccinated in 1976 were most likely not immune to the H1N1 virus of 2009.23
Avian influenza (bird flu) was first discovered in 1997 in Hong Kong and outbreaks in humans occurred in China in 2003. The bird flu is not easily transmitted between humans and therefore does not pose a threat for a pandemic.23
Signs and Symptoms
Signs and symptoms include fever, cough, sore throat, body ache, headache, stuffy nose, chills, and fatigue. People are contagious from 1 day before the onset of symptoms, up to 7 days after they realize they are sick. For diagnostic tests, treatments, and return to participation guidelines for the flu, please see Chapter 7.
Infectious Mononucleosis
Infectious mononucleosis (mono) has also been called the kissing disease because it is easily transmitted via oropharyngeal contact. Caused by the Epstein-Barr virus (EBV), mononucleosis is a common occurrence in college-aged athletes, but 50% of children have also had the infection by the age of 5 years. There is some speculation that chronic fatigue syndrome is associated with a chronic EBV infection, but little evidence supports this theory.7
The EBV is a herpesvirus that attacks lymphocytes and nasopharyngeal cells. It is found in oropharyngeal saliva secretions of up to 50% of healthy, nonsymptomatic adults.26 Ninety percent of adults over the age of 50 years have serological evidence of the disease, but few have had a full clinical presentation.27 Although a tainted blood transfusion is not a common transmission pathway for EBV, it is possible.26 Despite its reputation as the kissing disease only 5% of patients have a recent history of contact with an infected person, and it is not a particularly contagious disease. For reported direct exposure, the incubation period is 10 to 50 days.27 Nevertheless, athletes are warned to avoid sharing drinking cups and putting their mouths on common water bottle spouts.
Signs and Symptoms
The chief signs and symptoms of infectious mononucleosis consist of fatigue, pharyngitis, fever, and lymphadenopathy, but not all signs and symptoms are present in every patient. Often the first complaint is of overwhelming fatigue and the inability to get enough sleep (Figure 15-4). The athlete will feel run down or experience sore throat symptoms. Other manifestations include hepatitis, renal failure, pulmonary involvement, cough, encephalitis, dyspnea, and a maculopapular rash.28
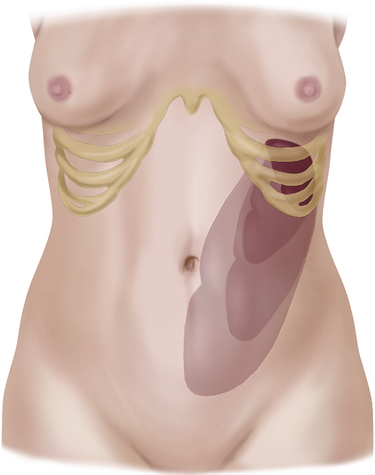
the course of the disease. Splenomegaly is present in 50% of cases and is most prevalent in the second and third weeks of the disease.7 When enlarged, the spleen is more susceptible to injury, because swelling causes it to protrude below the left costal margin (Figure 15-5). A blow to the left ribs of an athlete with splenomegaly can rupture the spleen, causing a life-threatening emergency if the injury is not quickly recognized and treated.
Although 10% of patients experience hepatomegaly, or an enlarged liver, with infectious mononucleosis, it does not carry the severe ramifications that splenomegaly does in athletics.27 There are hepatic complications, however, because hepatocellular enzyme levels are elevated two to three times normal in 95% of patients and can take as long as 1 month to return to preinfection rates.
Referral, Diagnostic Tests, and Differential Diagnosis
Athletes suspected of having infectious mononucleosis will often present with mild leukocytosis, which is also common in a number of other illnesses.7 Specifically, a strong indicator for EBV includes a blood count indicating lymphocytosis of 50% or greater, including at least 10% atypical cells.26,27
A more specific blood test, the mononucleosis spot test, or monospot, is based on agglutination, or clumping, of erythrocytes. This screening test is reliable in up to 90% of patients and is usually positive within 4 weeks of onset.27,28 However, the sensitivity for the presence of Epstein-Barr virus in the monospot test may be negative early after infection.29 False-positive Monospot results can occur in the context of other diseases, such as lymphoma, autoimmune disease, and hepatitis.30
Treatment
The standard treatment for mononucleosis is rest and hydration, although complete bed rest is not recommended.30 More than 95% of patients recover with symptomatic treatment alone.28
Research has shown that there is no specific pharmacological treatment promoting recovery from infectious mononucleosis.7 However, if the pharyngitis is such that it warrants medication, corticosteroids have been shown to relieve pain and prevent airway compromise from swelling. To assist in the management of body aches and fever, acetaminophen is preferred over aspirin because of aspirin’s association with Reye’s syndrome.7 In addition, athletes would be wise to avoid prolonged use of nonsteroidal antiinflammatory drugs (NSAIDs) during the illness because of hepatic complications already associated with mononucleosis.
Prognosis, Return to Participation, and Prevention
Infectious mononucleosis is a self-limiting disease associated with obvious symptoms for 2 weeks to 2 months; the most acute phase lasts 2 weeks. Research shows that 20% of military and university patients return within 1 week, and 50% return within 2 weeks.7 In athletics, special care must be taken to be sure the athlete is reconditioned for sport before full return. Athletes involved in contact or collision sports may need 1 month or more to recover sufficiently to allow the spleen to again fit behind the rib cage for adequate protection. Physicians need to consider each athlete individually along with the sport involved before allowing full return to activity.31 Whereas a swimmer may return to full activity rather quickly, a diver may still be in danger of spleen injury with a premature return to activity.
Mononucleosis has a mortality rate of less than 1% because of complications from the disease, namely encephalitis, splenic rupture, or airway obstruction from severe pharyngitis.7 It is prevented by proper hygiene, and by not sharing eating or drinking dishes or materials with infected people. Infectious mononucleosis is not a nationally reportable disease.
Mumps
Mumps is a contagious viral disease that manifests with enlarged parotid and salivary glands and on occasion involves the sublingual or submaxillary glands as well. It presents as an acute epidemic that peaks in late winter or early spring and chiefly involves 5- to 15-year-old children. Children younger than 2 years are typically immune.7 A national immunization campaign was intended to eradicate the disease by 2010, but with a 2006 outbreak in the Midwest involving more than 6500 people, it appears the disease is still present in the United States; and the two-dose vaccination was not sufficient to prevent the disease for many.13,14
Mumps has a 2- to 3-week incubation period and is spread through the air via infected droplets as well as through direct contact with contaminated saliva. It has been found in saliva 1 to 6 days before onset and up to 9 days after glandular swelling. It has also been found in the urine 6 days before parotitis (i.e., inflammation of the parotid salivary glands) and 15 days afterward. In addition, the virus may be isolated in symptomatic patients’ blood.7
Signs and Symptoms
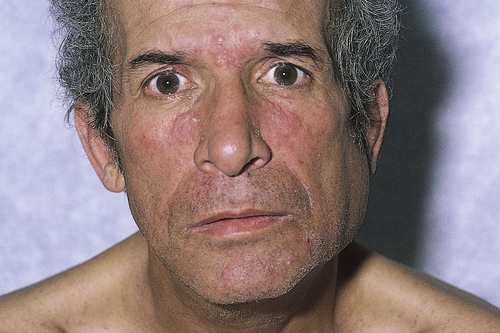
The chief signs and symptoms of mumps include parotitis, headache, low-grade fever, malaise, anorexia, vomiting, and nuchal rigidity in the posterior neck. Common symptoms also include pain with chewing and swallowing, especially swallowing acidic drinks or foods such as orange juice, pickles, or lemons. Within 24 hours of onset of the aforementioned signs and symptoms, the parotid glands swell and become sensitive to palpation (Figure 15-6). Initially, it is not unusual for only one gland to become swollen, with the second following about 2 days later.32 An athlete generally presents with asymmetry in the face and jaw caused by the unilateral swelling of the parotid gland. The enlargement of the glands can extend from in front of to below the ear, and the associated skin can become tight and shiny because of the pressure of the swelling.7
The complications of mumps include orchitis, oophoritis, meningoencephalitis, and pancreatitis. Postpubertal males may experience testicular inflammation, which is typically unilateral. Although this can occur in 20% to 30% of the adult males with mumps, it is rarely associated with infertility, but it can lead to testicular atrophy in 50% of the cases.26 Epididymitis precedes orchitis in 85% of the cases.33
In females, oophoritis occurs in 50% of postpubertal women with mumps and is more difficult to diagnose; however, it rarely results in fertility issues.33 Exposure to mumps within the first trimester of pregnancy may induce spontaneous abortion.2,7
Because the patient with mumps has a headache, stiff neck, and sometime low (20 to 40 mg/dl) cerebrospinal fluid (CSF) glucose levels, it is often mistaken for bacterial meningitis. Fifty percent of patients with mumps experience CNS involvement, but only 1% to 10% manifest symptoms. Although permanent damage such as deafness or facial paralysis is unusual, it may result from mumps with CNS involvement.7 Another rare association with mumps is encephalitis, which is more serious than viral meningitis.32 Encephalitis is thought to be an autoimmune response producing demyelination and has an onset 7 to 10 days after parotitis.
Referral, Diagnostic Tests, and Differential Diagnosis
Patients who present with swollen saliva glands, malaise, or a low-grade fever are referred to a physician. The diagnosis is largely based on signs and symptoms coupled with a history of recent exposure. Atypical presentations require laboratory confirmation, usually by culturing the mumps virus or discovering the mumps immunoglobulin M (IgM) antibody.2
Treatment, Prognosis, and Return to Participation
A person with mumps should be isolated from others until parotid swelling returns to normal. Treatment of the disease is based on the person’s symptoms. Use of over-the-counter analgesics or antipyretics as necessary to alleviate headache and fever, avoidance of acidic foods and beverages, and maintaining a soft diet to lessen mastication are encouraged. Because mumps is typically a self-limited disease, most patients recover without pharmacological intervention.34
Prevention
A vaccine for mumps is available that causes little systemic reaction. The live virus vaccine, introduced in the United States in 1967, is administered alone or in combination with rubella and measles (MMR) viruses. It is generally administered anytime after the first year of life but most typically between 12 to 15 months of age.26 Current recommendations suggest a second dose between ages 4 and 6 years. This childhood vaccination is intended to be lifelong, but no studies have supported this claim. Postexposure vaccination will not necessarily prevent subsequent onset from that exposure.7
Rubeola
Also known simply as “measles” or “red measles,” rubeola is one of the most highly communicable infectious diseases. Before immunization was available, more than 90% of the population was infected by the age of 20 years.26 After immunization, measles cases have dropped 99%, with the residual in the United States attributed to unimmunized or underimmunized children who have had only one shot. There are still outbreaks worldwide, with China (131,441 reported cases in 2008) and Japan (11,015) leading Western Europe in outbreaks.35 The resurgence of measles have been attributed to living in remote communities, misinformation regarding the vaccine, cultural factors, and insufficient vaccine coverage.36–38
Measles is spread through airborne droplets via nasal or throat secretions of infected people. A lesser means of transmission is through direct contact with soiled articles such as towels, which may contain secretions from those already sick. The incubation period is typically 10 days but can range from 7 to 18 days.26 Measles is most contagious just before the rash erupts through 4 days after eruption.
Signs and Symptoms
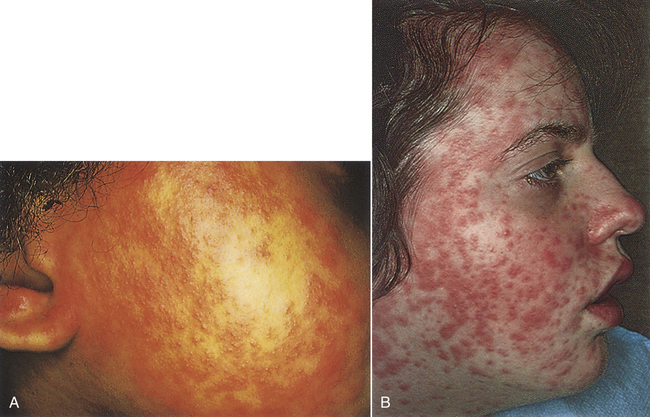
Most often, a rash is the manifestation of rubeola, and it appears after a prodromal fever, most often in the third to seventh day of the disease. The erythematous rash begins on the face before spreading to the body proper and lasts approximately 4 to 7 days (Figure 15-7). The patient is contagious before eruption of the rash and for up to 4 days after appearance of the rash. Other signs and symptoms of measles include conjunctivitis, cough, leukopenia, headache, fever, and sore throat. Leukopenia will be present beginning with the onset of the rash largely because of a decrease in lymphocytes.2 Complications arising from the disease include otitis media, pneumonia, encephalitis, diarrhea, and laryngotracheobronchitis, or croup.10
Referral, Diagnostic Tests, and Differential Diagnosis
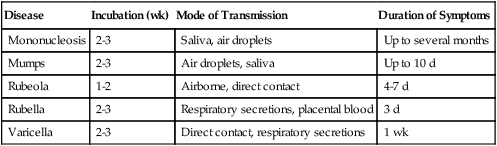
Many childhood diseases have similar presentations and are often the differential diagnoses of each other. Table 15-1 compares several childhood diseases. Specific differential diagnoses for rubeola are rubella, mononucleosis, influenza, Rocky Mountain spotted fever, and allergic rhinitis.
TABLE 15-1
Comparison of Childhood Infectious Diseases
| Disease | Incubation (wk) | Mode of Transmission | Duration of Symptoms |
| Mononucleosis | 2-3 | Saliva, air droplets | Up to several months |
| Mumps | 2-3 | Air droplets, saliva | Up to 10 d |
| Rubeola | 1-2 | Airborne, direct contact | 4-7 d |
| Rubella | 2-3 | Respiratory secretions, placental blood | 3 d |
| Varicella | 2-3 | Direct contact, respiratory secretions | 1 wk |
Treatment, Prognosis, and Return to Participation
Because no antiviral remedy for measles is currently available, the best treatment is supportive and symptomatic care. Rubeola is largely a self-limiting disease, but analgesics and antipyretics may help alleviate symptoms associated with the illness.34 If the patient has accompanying bacterial complications, such as conjunctivitis, otitis, sinusitis, or pneumonia, antibacterial therapy may be warranted.
Prevention and Public Health Implications
Individuals born after 1957 are encouraged to be immunized for measles. A single injection of the live measles virus is often administered in conjunction with two other live viruses, mumps and rubella, and reduces susceptibility to measles by 94% to 98%, whereas a second dose may elevate immunity to 99%.2,7,34 The two-dose vaccine is recommended to ameliorate the possibility of immunization failure. Most often, the MMR initial dose is given at 12 to 15 months of age, with the second dose administered at the onset of school (4 to 6 years), although if exposure risk is high, the second dose can be delivered as soon as 4 weeks after the first.
Rubella
Rubella is acquired through the upper respiratory tract or through placental blood exchange with a mother infected in early pregnancy. Exposure to rubella during pregnancy can cause abortion or stillbirths or profoundly affect the fetus.30 Congenitally acquired rubella can result in deafness in 85% of children, intrauterine growth restriction (70%), retinopathy (35%), in utero death (20%), mental retardation (up to 20%), behavior disorders (20%), bone radiolucencies (10% to 20%), diabetes mellitus (up to 20% by age 35 years), and cardiac defects.33 Obviously, great care must be taken to ensure that pregnant women are safeguarded from exposure.