3
Diagnostic Imaging and Testing
Sally A. Perkins and Lawrence J. Kusior
At the completion of this chapter the reader should be able to do the following:
1. Identify the various diagnostic imaging and laboratory tests for a given medical condition
2. Explain test preparation and procedures to patients undergoing diagnostic evaluation
3. Relate risks and side effects of specific procedures
4. Justify which medical conditions can be diagnosed by specific diagnostic imaging or laboratory testing
5. Apply appropriate pre-MRI testing health questions to patients
6. State normal values for urine and blood
7. Differentiate radiation levels of assorted diagnostic tests
Diagnostic Imaging
Radiography: X-rays
An x-ray is a form of electromagnetic radiation that, when passed through a patient, allows viewing of internal structures. The x-ray beam is absorbed to different extents by the various body tissues. Less dense tissue appears darker because the radiation is not absorbed in these structures. For example, the lungs appear dark because air does not absorb radiation. Fat is gray, and bone and calcium are light or white (Figure 3-1). Sometimes
contrast agents such as barium or iodine are introduced intravenously and are used for gastrointestinal imaging. Contrast agents generally show on the radiograph as white or light. Most of the x-ray beam is absorbed by the tissues or is scattered, while a small amount passes through the body part to the receptor, creating the image. The image may be developed to film or, in the case of digital radiographs, may be saved and viewed on a computer.
Risks or Side Effects
Radiographs should not be taken of women who are pregnant, because the radiation may have an effect on the fetus. It is imperative that pregnancy status be determined by a blood test, or through a comprehensive menstrual history, before radiography is allowed. Any time that radiation is used there is a slight chance of developing certain types of cancer such as leukemia and melanomas. Physicians try to minimize exposure to x-rays by using the least amount of radiation necessary and by screening patients on the basis of criteria such as the Ottawa ankle rules. The Ottawa ankle rules are used to determine whether radiographs should be taken after an ankle injury. There are also criteria for the knee. Criteria for the ankle/foot are based on location of bone pain, tenderness, and weight-bearing ability. Criteria for the knee are slightly different, with consideration of age (over 55 yr), patella and/or fibular head tenderness, ability to flex the knee, and weight-bearing ability. Table 3-1 illustrates the amount of radiation introduced into the body for common diagnostic tests, including x-ray radiographs.
TABLE 3-1
Comparison of Radiation From Imaging and Natural Radiation Exposure
| For This Procedure: | The Effective Radiation Dose (mSv) Is: | Comparable to Natural Background Radiation for: |
| Abdominal Region | ||
| Computed Tomography | ||
| Abdomen and pelvis | 10 | 3 yr |
| Body | 2-10 | 8 mo to 3 yr |
| Radiography | ||
| Lower GI tract | 8 | 3 yr |
| Upper GI tract | 6 | 2 yr |
| Bone | ||
| Radiography | ||
| Spine | 1.5 | 6 mo |
| Extremity | 0.001 | Less than 1 d |
| Bone densitometry (DEXA) | 0.001 | Less than 1 d |
| Central Nervous System | ||
| Computed Tomography | ||
| Head | 2 | 8 mo |
| Spine | 6 | 2 yr |
| Myelography | 4 | 16 mo |
| Chest | ||
| Computed tomography: chest | 7 | 2 yr |
| Radiography: chest | 0.1 | 10 d |
| Face and Neck | ||
| Computed tomography: sinuses | 0.6 | 2 mo |
| Women’s Imaging | ||
| Mammography | 0.7 | 3 mo |
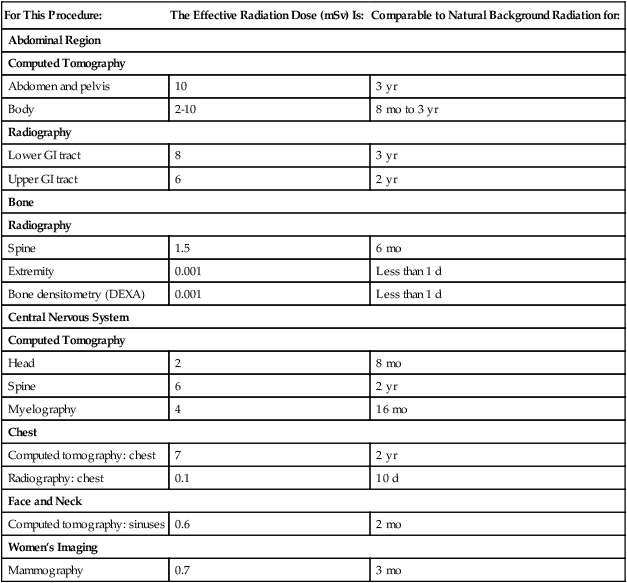
Modified from RadiologyInfo.org: Radiation exposure in x-ray examinations. Available at http://www.radiologyinfo.org/en/safety/index.cfm?pg=sfty_xray#2. Accessed June 2010.DEXA, Dual-energy x-ray absorptiometry; GI, gastrointestinal; mSv, millisievert.
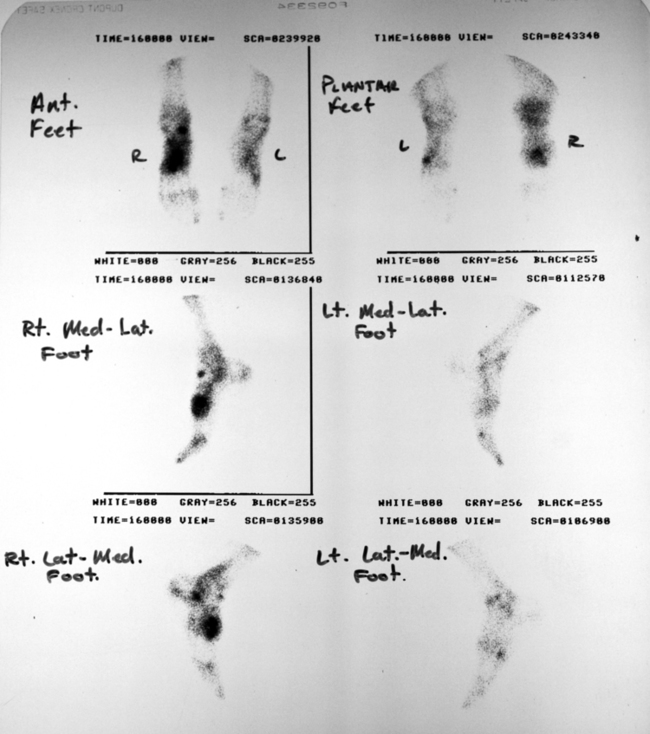
Radionuclide Bone Scan
Areas of inflammation or injury to a bone will appear dark on a bone scan; these are called “hot spots.” Lighter areas on the bone scan show normal tissue and bone (Figure 3-2).
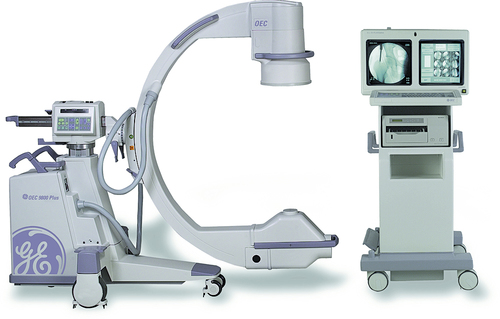
Fluoroscopy
The patient stands or sits next to the machine and the technician lines up the machine and the structure to be evaluated (Figure 3-3). Radiation is allowed to pass through the skin, creating light and shadows that are viewed on a computer screen and can be printed. Dense areas such as bone will appear white on the film, and less dense areas such as the lungs will appear darker.
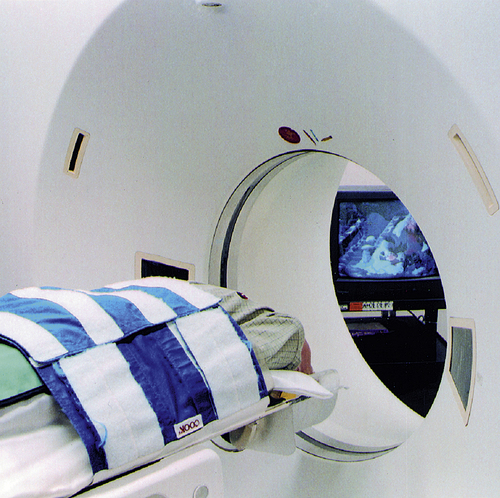
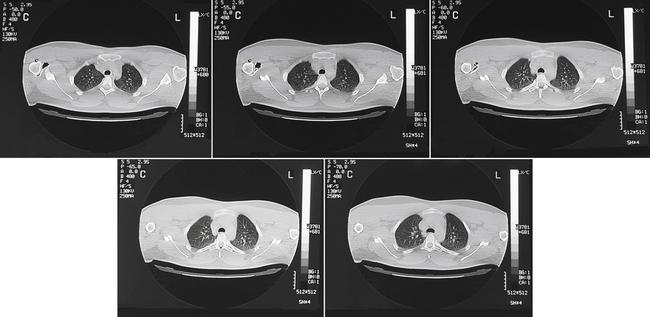
Computed Tomography Scan
A computed tomography (CT) scan combines specialized high-resolution radiographs with computers to give better visualization of internal structures in cross-section or three dimensions (3D). It works by passing rotating beams of x-rays through the patient and measuring the transmission at thousands of points. The images may be seen individually as a series of cross-sectional “slices,” but 3D images can be produced by a computer (Figure 3-4). CT exposes a patient to about 10 to 100 times the radiation of an x-ray. Depending on the structures to be examined, the patient may be injected with a contrast dye or asked to consume a barium or other contrast solution at various intervals before or during the CT scan. Contrast agents are usually the same iodinated agents used in other imaging studies. The patient may feel some warmth as the contrast dye is administered intravenously.
CT scans are performed to look at cross-sections of internal organs, bone, soft tissue, and blood vessels (Figure 3-5).
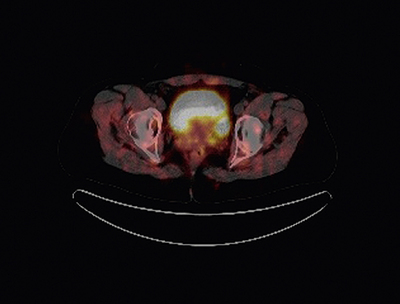
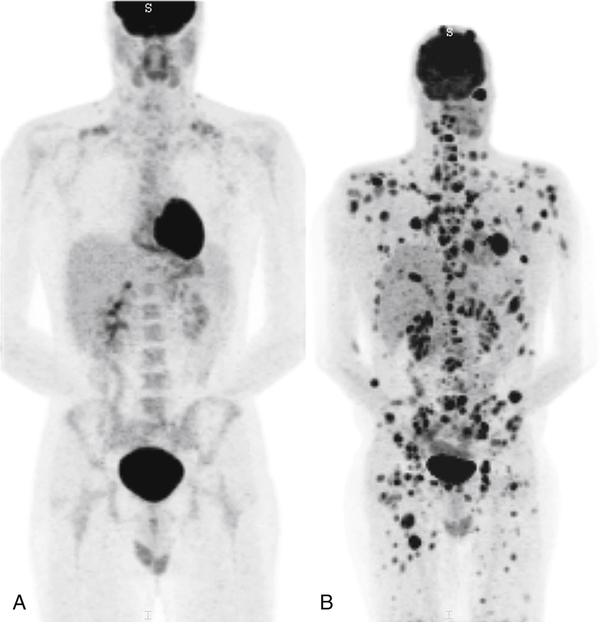
Positron Emission Tomography Scan
A positron emission tomography (PET) scan is ordered by a physician to examine the cell metabolism and biochemistry of tissue and organs. PET scans can identify abnormal metabolic activity before it becomes apparent on a CT scan or by magnetic resonance imaging (MRI). The patient is administered a glucose-based radionuclide injection intravenously, or tablets by mouth, depending on the suspected condition. The patient is placed on a table and the imaging unit takes pictures of specific areas of the body. The patient needs to remain still at all times and may be asked not to breathe for short periods of time so that the image produced is clear. The table will move the patient in and out of the machine, similar to a CT scan. At times the machine may move around the patient. The glucose-based radionuclide is absorbed by the area of abnormal metabolic activity and will appear dark on the body image view, similar to a bone scan, or as bright colors on 3D images (Figures 3-6 and 3-7).
Magnetic Resonance Imaging
An MRI scan (also termed an “MR”) is a test that applies a magnetic field to the body. The magnetic field aligns the body’s atoms in such as way that, when released, they generate radio waves. The frequency of the emitted radio waves is related to the location and chemical environment of the atoms (Figure 3-8). A computer analyzes the data and creates an image. This image provides detailed information about organs, soft tissue, bones, tumors, bleeding, or infection. MRI scans are used to identify tumors, musculoskeletal injuries, soft tissue conditions, fractures, and bleeding (Figure 3-9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree