CHAPTER 19 The wrist and hand
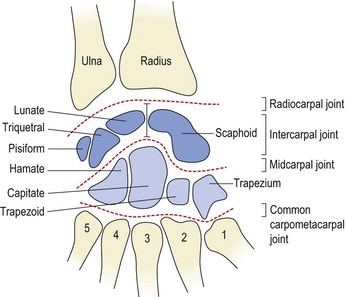
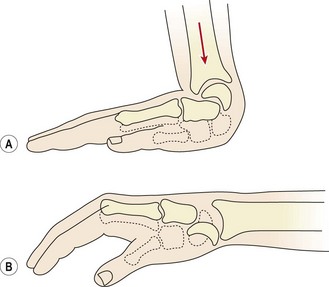
The wrist area has a series of articulations between the distal end of the radius and the carpal bones (radiocarpal joint), and between the individual carpals themselves (intercarpal joints). The radiocarpal joint is formed between the distal end of the radius and the scaphoid, lunate and triquetral. The end of the radius being covered by a concave articular disc. The eight carpal bones are arranged in two rows, the junction between the rows forming the mid-carpal joint. This joint is convex laterally and concave medially, giving it an ‘S’ shape (Fig. 19.1).
The wrist is strengthened by collateral, palmar and dorsal ligaments. The ulnar collateral ligament is a rounded cord stretching from the ulnar styloid to the triquetral and pisiform. The radial collateral ligament passes from the radial styloid to the scaphoid and then to the trapezium. The dorsal radiocarpal ligament runs from the lower aspect of the radius to the scaphoid, lunate and triquetral. On the palmar surface, the radiocarpal and ulnocarpal ligaments attach from the lower ends of the radius and ulna to the proximal carpal bones (Fig. 19.2).
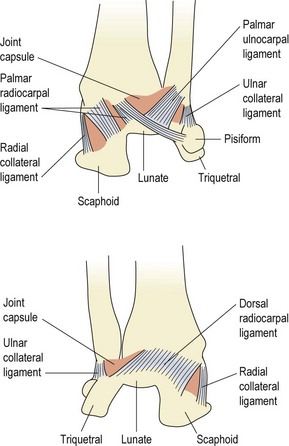
Figure 19.2 The capsular and collateral palmer ligaments of the radiocarpal joint. (A) Anterior. (B) Posterior.
After Palastanga, Field and Soames (1994) with permission.
The available range of movement at the wrist is a combination of radiocarpal and mid-carpal movement. Flexion occurs more at the mid-carpal joint, while extension is greater at the radiocarpal joint, but the combined movement is about 85° in each direction. Abduction occurs mostly at the mid-carpal joint and has a range of about 15°, whereas adduction involves more movement of the radiocarpal joint and has a range of 45° (Palastanga, Field and Soames, 1989). The difference in range occurs because the radial styloid comes down further than the ulnar styloid, and so is more limiting to abduction.
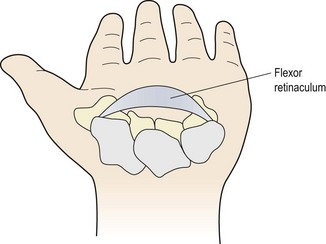
The carpal bones form a transverse arch, concave on their palmar aspect (Fig. 19.3). This arch is maintained by the flexor retinaculum, which attaches medially to the pisiform and the hook of hamate. Laterally, the retinaculum binds to the scaphoid tubercle and to the groove of trapezium, through which runs the tendon of flexor carpi radialis. The space formed beneath the retinaculum is called the ‘carpal tunnel’, and the tendons of flexor pollicis longus, flexor digitorum profundus, flexor digitorum superficialis and the median nerve pass through it.
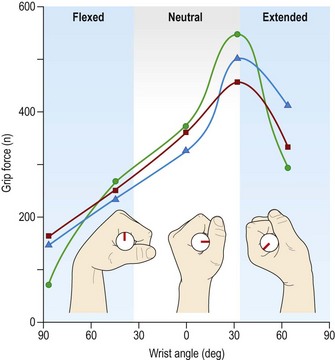
Grip
In power grips the long flexors and extensors work to lock the wrist and grip the object. A balance must exist between these two sets of muscles to lock (stabilize) the wrist in its optimal gripping position. Where this balance breaks down pathology may result. In lateral epicondylalgia for example (see Chapter 18) the power of the long extensors is reduced allowing the flexors to dominate, giving an average of 11° less wrist extension (Bisset et al., 2006). The line of action of the finger flexor muscles (flexor digitorum superficialis and profundus) is at some distance to the axis of the wrist joint. This position creates a significant leverage force which tends to flex the wrist as well as the fingers. This tendency for wrist flexion is counterbalanced by the extensor carpi radialis muscles to give an optimal gripping position of 35° wrist extension and 5° ulnar deviation. During light grip the extensor carpi radialis brevis (ECRB) is most active, but as grip power increases and heavier objects are held the extensor carpi ulnaris (ECU) and extensor carpi radialis longus (ECRL) are activated (Neumann, 2002). Grip force is reduced as wrist flexion increases (Fig. 19.4) due to the shortened position of the finger flexors and the passive extension force created by the finger extensor muscles.
Screening examination
This examination, described by Cyriax (1982), provides the examiner with enough information to establish whether a lesion is intracapsular or not, and whether contractile tissue is affected. For the physiotherapist, further assessment is usually required to assess and record range of motion and accessory movements. Movements of the individual carpal bones gives more detail about the exact site of the lesion, and the sequence for testing is shown in Table 19.1. In addition, specific tests are used once the initial examination has focused the therapist’s attention onto a specific area or series of tissues.
Table 19.1 Assessing motion of individual carpal joints
| Movements around the capitate |
| Movements on the radial side |
| Movements of the radiocarpal joint |
| Movements on the ulnar side |
From Kaltenborn, F.M. (1993) The Spine. Basic Examination and Mobilisation Techniques, 2nd edn. Olaf Norlis Bokhandel, Oslo, Norway. With permission.
Scaphoid fracture
A further cause of injury to the scaphoid is striking an object with the heel of the hand, a mechanism seen in contact sports such as the martial arts or in a collision with another player. In addition, scaphoid fracture can be seen as a punching injury. Horii et al. (1994) described a series of 125 patients with fractured scaphoid, 14% of whom had acquired the injury through punching. Normally it is a bending force within the scaphoid which creates the fracture line when falling onto the outstretched hand. With a punching scaphoid fracture, however, stress force creates the fracture, making displacement and delayed union more likely.
Examination
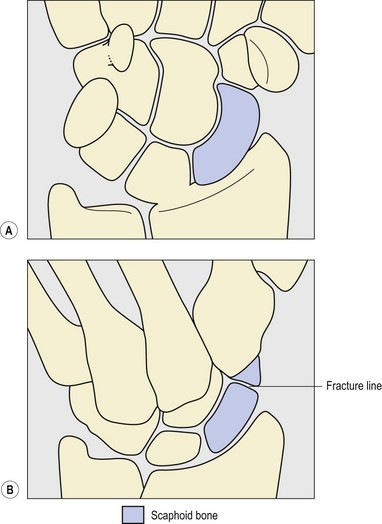
Radiographic examination is helpful, but a negative x-ray does not rule out fracture (Garrick and Webb, 1990). Non-displaced fractures are often normal to begin with and only become positive when some bone reabsorption has occurred, the fracture line beginning to show up 2–4 weeks after injury. Plain AP (anteroposterior) views of the wrist may easily miss a scaphoid fracture (Fig. 19.5A), while a specialist scaphoid view which focuses on the bone itself is more reliable (Fig. 19.5B).
The scaphoid is ‘nut-shaped’ with a narrow waist and two poles (proximal and distal). On the palmar surface of the distal pole there is a tubercle for the attachment of the flexor retinaculum and the tendon of abductor pollicis brevis. The blood supply to the scaphoid enters through the waist (centre) of the bone (Fig. 19.6). Smaller arteries enter from the distal pole and retrograde flow from these supplies the proximal pole, this pole having no separate blood supply itself. This has an important clinical bearing, because fractures to the waist of the bone can sever the communicating vessels, starving the proximal segment of blood (Gutierrez, 1996). This situation makes non-union or malunion more likely.
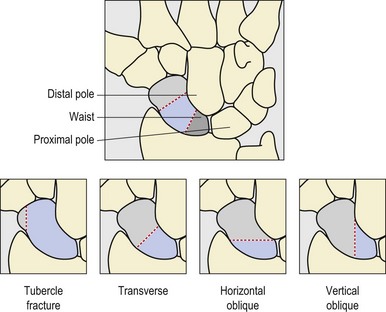
Figure 19.6 Classification of scaphoid fracture.
From Gutierrez, G. (1996) Office management of scaphoid fractures. Physician and Sportsmedicine 24(8), 1–8. With permission.
Classification of injury is important as fractures occurring more proximally tend towards avascular necrosis. In addition, fracture orientation should be noted (see Fig. 19.5) as this will influence stability. Horizontal oblique fractures are generally stable, whereas transverse fractures are inherently unstable.
Management
Successful union has been shown in 90% of patients treated with a Herbert differential pitch screw (which is completely buried in the bone) combined with bone grafting (Bunker, McNamee and Scott, 1987). This type of fixation significantly reduces the time to return to active sport. With fixation, return in some athletes is immediate, but on average 4.3 weeks. Athletes treated non-operatively with a playing cast return on average in 11 weeks (Rettig, Weidenbener and Gloyeske, 1994). In a systematic review (12 studies met the inclusion criteria out of 112 initially considered), Modi et al. (2009) found percutaneous fixation to give faster rates of union and an earlier return to sport (mean 7 weeks) compared with cast immobilization.
Wrist pain
Sprains
A ‘sprained wrist’ is a common diagnosis, but really only indicates the area of pain, and the fact that soft tissue is the likely structure affected. The most common tissues affected are the intercarpal ligaments, with or without subluxation of a carpal bone. Pain is reproduced to passive wrist flexion and is generally well-localized to the particular tissue injured. Common ligaments affected include the lunate-capitate (Cyriax, 1982) and scapho-lunate (Wilkes, 1989). Transverse frictions to the ligament with the wrist flexed are effective, but manipulation to rupture adhesive scarring is not (Cyriax, 1982).
Carpal dislocation
Subluxation or dislocation of a carpal bone, rather than a scaphoid fracture, may occur from a fall onto the outstretched hand. The bone most commonly affected is the lunate, although the capitate may also sublux (Cyriax and Cyriax, 1983). Movement is generally limited in one direction only (contrast the capsular pattern). Pain is localized by palpating in a line along the third finger to reach the third metacarpal. In the normal hand the capitate lies in a hollow just proximal to the base of the third metacarpal and the lunate is felt proximal to this, and slightly towards the ulna.
Keypoint
When palpating the dorsum of the wrist the capitate bone lies in a hollow just proximal to the base of the third (centre) metacarpal and the lunate is felt proximal to this, and slightly towards the ulna (see Fig. 19.1).
Full dislocation of the lunate may occur with a fall onto the extended wrist. The shape and position of the lunate lying between the lower radius and capitate make it prone to dislocation. On forced wrist extension, the wedged-shaped lunate is squeezed out from between the two bones to lie on the palmar surface of the carpal region (Fig. 19.7) as an apparent ‘swelling’. If the athlete is asked to form a fist, the third metacarpal head should normally project above the second and fourth. Where the lunate has dislocated, however, all three metacarpal heads may appear in line (Magee, 2002).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree