CHAPTER 11 The ankle
Approximately 14% of all sports injuries are sprains to the ankle, representing one ankle injury each season for every 17 participants. In high risk sports, such as jumping and running, this percentage is even higher, at 25% of all lost-time injuries (Reid, 1992). Ankle sprain has been shown to be 2.4 times more common in the dominant leg, and to have a high (73.5%) prevalence of recurrence (Yeung et al., 1994).
The joint mechanics of the ankle and foot have been described in Chapter 7. The ankle joint is the articulation between the trochlear surface of the talus and the distal ends of the tibia and fibula. The fibula may support 15–20% of the body weight (Lambert, 1971), with the fibula moving downwards and laterally during the stance phase of running to deepen the ankle mortice and enhance stability. This fibular motion creates tension in the interosseous membrane and tibiofibular ligament to provide some shock attenuation. Loss of this mechanism through tibiofibular disruption greatly affects the ankle joint, with a 1–2 mm lateral shift of the fibula increasing joint forces by as much as 40% (Reid, 1992).
The ankle is subjected to considerable compression forces during sport (Fig. 11.1). Compression forces as high as five times body weight have been calculated during walking and up to 13 times body weight during running (Burdett, 1982).
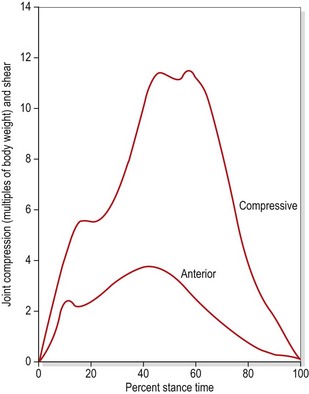
Figure 11.1 Compression forces on the talus during running.
From Burdett, R.G. (1982) Forces predicted at the ankle during running. Medicine and Science in Sports and Exercise, 14, 308. With permission.
Collateral ligaments
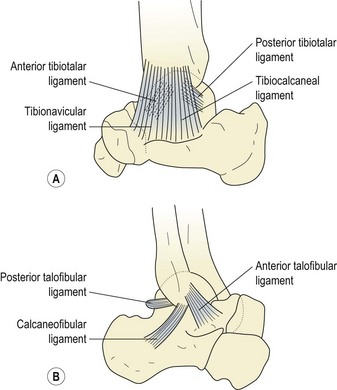
The medial (deltoid) ligament (Fig. 11.2A) is triangular in shape. Its deep portion may be divided into anterior and posterior tibiotalar bands. The more superficial part is split into tibionavicular and tibiocalcaneal portions, which attach in turn to the spring ligament. The lateral ligament (Fig. 11.2B) is composed of three separate components, and is somewhat weaker than its medial counterpart. The anterior talofibular (ATF) ligament is a flat band 2–5 mm thick and 10–12 mm long which travels from the anterior tip of the lateral malleolus to the neck of the talus, and may be considered the primary stabilizer of the ankle joint (Palastanga, Field and Soames, 1989). The posterior talofibular (PTF) ligament travels almost horizontally from the fossa on the bottom of the lateral malleolus to the posterior surface of the talus. Lying between the ATF and PTF ligaments is the calcaneofibular ligament, arising from the front of the lateral malleolus to pass down and back to attach onto the lateral surface of the calcaneum. The role of the collateral ligaments in maintaining talocrural stability is summarized in Table 11.1.
Table 11.1 Role of the collateral ligaments in ankle stability
| Movement | Controlled by |
|---|---|
| Abduction of talus | Tibiocalcaneal and tibionavicular bands |
| Adduction of talus | Calcaneofibular ligament |
| Plantarflexion | ATF ligament and anterior tibiotalar band |
| Dorsiflexion | Posterior tibiotalar band and PTF ligament |
| External rotation of talus | Anterior tibiotalar and tibionavicular bands |
| Internal rotation of talus | As above with ATF ligament |
Adapted from Palastanga, Field and Soames (1989).
Injury
Swelling
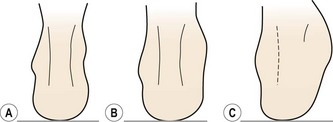
There is usually an egg-shaped swelling in front of, and around, the lateral malleolus. When viewed from behind, the definition of the Achilles tendon is a good indicator of severity of injury (Reid, 1992). With more severe injuries (grade III) the definition of the Achilles tendon is lost due to excessive bleeding into the joint (Fig. 11.3).
Objective measurement of swelling is made using the figure-of-eight measure, a valid and reliable measure (Mawdsley, Hoy and Eerwin, 2000; Rohner-Spengler, Mannion and Babst, 2007). For this test the end of a tape measure is placed on the anterolateral aspect of the ankle midway between the tibialis anterior tendon and the lateral malleolus. The tape is passed medially over the dorsum of the foot to the tuberosity of navicular and then beneath the plantar aspect proximal to the tubercle of the 5th metatarsal. The tape passes medially once more to rest distal to the medial malleous and is pulled across the Achilles back to the starting point.
Manual evaluation
The lateral malleolus should be gently palpated to assess if bone pain is present; if it is, an x-ray may be required (see below). If palpation reveals tenderness below, rather than over, the lateral malleolus and the athlete is able to bear weight, there is a 97% probability of soft tissue injury alone (Vargish and Clarke, 1983). Any fracture that is missed by this type of close palpation is likely to be an avulsion or non-displaced hairline type that will respond favourably to management as a sprain (Garrick and Webb, 1990).
Ligamentous laxity may be assessed using the anterior draw test when acute inflammation has subsided. The patient’s foot is placed in slight (10−15°) plantarflexion and the heel is gripped with the therapist’s cupped hand, while the other hand stabilizes the lower tibia and fibula. The heel is drawn forwards against an opposite force pressing the tibia backwards and the amount of anterior movement is noted if the talus moves out of the ankle mortice. The test determines the integrity of both the anterior talofibular ligament and the calcaneofibular ligament and has been shown to be valid when compared to surgical observation (van Dijk et al., 1996).
Following severe ankle sprain or fracture, a bony link may form between the tibia and fibula (tibiofibular synostosis). Typically, pain occurs after an injury, and increases during vigorous activity, mimicking stress fracture. Pain is most severe during the push-off action of running and jumping, and dorsiflexion is often limited to 90°, mimicking impingement pain (see below). The synostosis is revealed by x-ray and removed surgically (Flandry and Sanders, 1987).
X-ray
Accurate physical examination will usually give sufficient information to preclude fracture, making x-ray unnecessary in most cases. Only 15% of patients suffering an acute ankle injury may have a fracture, and the Ottawa Ankle Rules provide a highly accurate clinical decision guide in this respect (Stiell et al., 1994). The rules state:
A poster describing the rules is free to download at www.ohri.ca/emerg/cdr/docs/cdr_ankle_poster.pdf.
In a systematic review of 27 studies (15 581 patients) Bachmann et al. (2003) found the sensitivity of the Ottawa Ankle Rules to be almost 100% and claimed that their application would reduce the number of unnecessary radiographs by 30−40%.
Fractures associated with ankle injuries
Osteochondral lesion of talar dome
This fracture is more common in cases where ankle sprain has occurred in the presence of a compression force such as landing from a single leg jump. The talar dome is compressed within the ankle mortise and may fracture at the superomedial corner particularly. The condition is normally not recognized at the time of injury, but presents as a dull persistent ache during rehabilitation. There will be persistent swelling with stiffness. The site can be palpated by plantar flexing the ankle to draw the talar dome forwards of the ankle mortise. Injury may be graded from (I) focal compression of the subchondral bone through to (IV) fully detached bone fragment. Treatment is by reduced weight bearing while maintaining motion to stimulate cartilage healing (Karlsson, 2007). Occasionally arthroscopic removal of the bone fragment may be required.
Fracture of talar process
The lateral aspect of the talus, which normally articulates with the fibula and calcaneus, may fracture. Pain occurs over the bone area which is palpated anterior and inferior to the tip of the lateral malleolus. If the fracture is not displaced, simple immobilization is required. Where displacement is greater than 2 mm excision or internal fixation is generally required (Karlsson, 2007).
Management of an ankle sprain
Early mobility is essential to increase ligament strength and restore function. For grade I and II injuries, early mobilization has been shown to be more effective than immobilization. In a group of 82 patients with these grades of injury, 87% who were immobilized with a plastercast for 10 days still had pain after 3 weeks. This compared to 57% of those who received early mobilization in the form of an elastic strap for 2 days followed by a functional brace for 8 days (Eiff, Smith and Smith, 1994). Even grade III injuries (rupture) respond better to conservative treatment than surgery. Studies have shown 87% good and excellent results with conservative management compared to 60% for surgery of grade III injuries. In addition at 6 weeks post injury the surgical group had limited range of motion not seen in the conservative group (Kaikkonen, Kannus and Jarninen, 1996).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree