CHAPTER 17 The shoulder
Functional anatomy
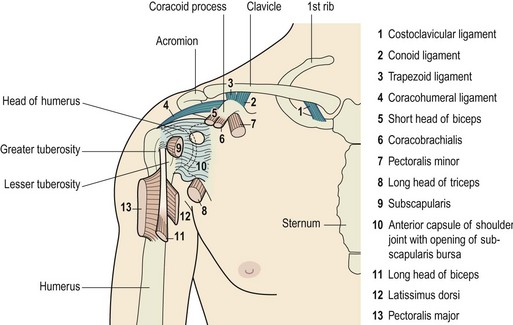
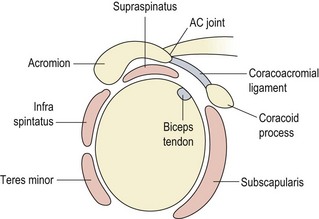
The glenoid fossa is only one third the size of the humeral head, but the fossa is extended by the glenoid labrum attached to its periphery. This fibrocartilage rim is about 4 mm deep with its inner surface lined by, and continuous with, the joint cartilage. The joint itself is surrounded by a loose capsule with a volume twice as large as the humeral head. The anterior capsule is strengthened by the three glenohumeral ligaments. The lower portion of the capsule is lax in the anatomical position, and hangs down in folds. It has two openings, one for the passage of the long head of biceps and the other between the superior and middle glenohumeral ligaments which communicates with the subscapular bursa (between subscapularis and the joint capsule). The capsule is further strengthened by the rotator cuff muscles which act as ‘active ligaments’ and blend with the lateral capsule. The ‘roof’ of the joint is formed by the bony coracoid and acromion processes and the coracoacromial ligament which runs between them, the three structures together forming an arch. Surface marking of the shoulder is shown in Fig. 17.1.
Rotator cuff action
Most joints have a high degree of passive stability provided by their capsules and ligaments (see also Table 17.3). The shoulder, however, depends more on the active stability provided by its muscles to maintain joint integrity. In the anatomical position, the weight of the arm is largely supported by the coracohumeral ligament and superior capsule. When the arm moves away from the side of the body, tension in the superior capsule is immediately lost. Now joint stability is provided by the rotator cuff muscles alone.
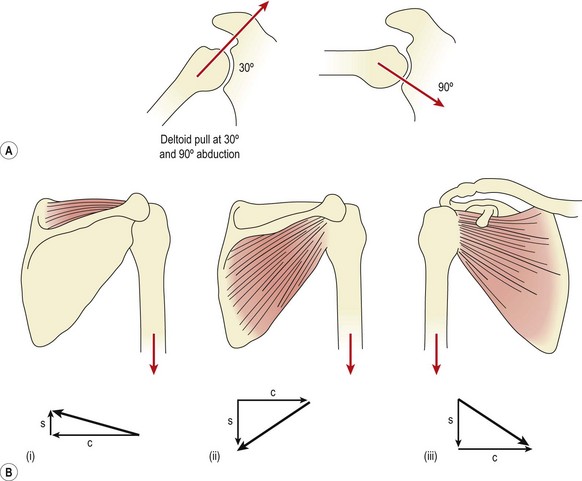
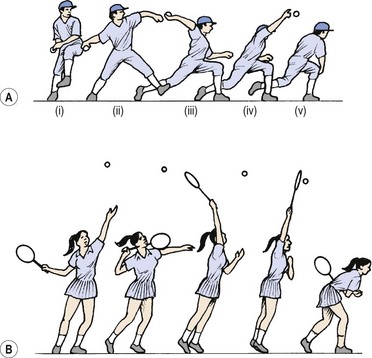
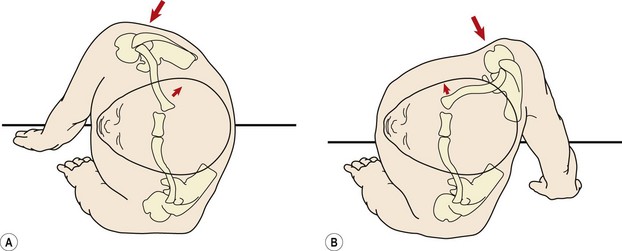
Active abduction of the humerus is accomplished by the supraspinatus and deltoid, acting as the prime movers. With the arm dependent, contraction of the deltoid (particularly the middle fibres) merely approximates the joint (upward translation), because the medial muscle fibres run almost parallel with the humerus. Unopposed, this pull would force the head of the humerus into the coracoacromial arch, resulting in impingement. Contraction of the infraspinatus, subscapularis, and teres minor (Fig. 17.2) causes compression and downward translation to offset the upward translation of deltoid (Culham and Peat, 1993). In an overhead throwing or serving action (Fig. 17.3) the subscapularis moves superiorly because the humerus has externally rotated and the muscle can no longer effectively control the humeral head. The infraspinatus and to a lesser extent the teres minor stabilize the joint anteriorly in this position (Cain, Mutschler and Fu, 1987). For this reason sEMG addresses this muscle in stabilization programmes targeted at throwing sports. By 90° abduction, the pull of the deltoid no longer tends to cause impingement, as shear forces are exceeded by compression, and the humeral head is stabilized into the glenoid (Perry and Glousman, 1995).
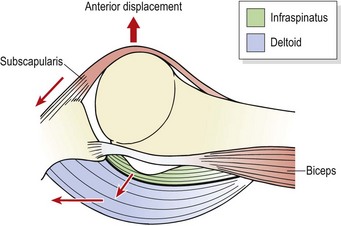
Figure 17.3 Muscular restraints to anterior displacement of the humeral head in an overhead throwing action.
Adapted from Reid (1992), with permission.
Scapulohumeral rhythm
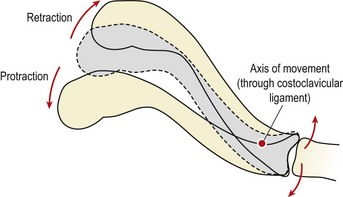
Motion of the shoulder girdle as a whole changes the position of the glenoid fossa, placing it in the most favourable location for the maximum range of humeral movement. When the glenoid cavity moves, it does so in an arc, the diameter of which is the length of the clavicle (Palastanga, Field and Soames, 1989). The medial border of the scapula moves in a similar but smaller arc and as a consequence the positions of the shoulder girdle structures change in relation to each other.
With both shoulder abduction and flexion, the clavicle axially rotates. As the scapula twists, the coracoclavicular ligament ‘winds up’ and tightens, causing the clavicle itself to rotate. As the arm is abducted to 90° (phase I and II, see below) the clavicle elevates by 15° but does not rotate. Above 90° (phase III) further elevation of the clavicle occurs (up to 15°) but marked posterior rotation now occurs to 30–50° (Magee, 2002). For this reason a diminished range of movement at either SC or AC joints which reduces clavicular rotation will also impair scapular and therefore glenohumeral motion.
The abduction cycle
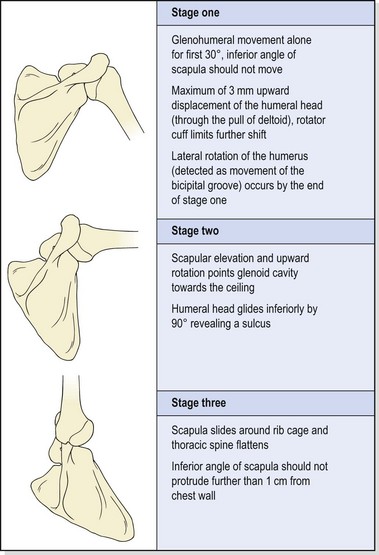
Movement of the arm into abduction may be divided into three overlapping stages (Table 17.1).
Table 17.1 Movement of the arm into abduction
Stage (I)
In stage (I), no movement of the scapula should occur. The scapular stabilizers (serratus anterior especially) should hold the scapula firmly on the ribcage, providing a stable base for the humerus to move upon. As the arm abducts, lateral rotation of the humerus may be detected by palpation of the bicipital groove (intertubercular sulcus). If the humerus is maintained in a neutral position, abduction in the frontal plane is limited to about 90°. Laterally rotating the humerus increases this range to 120° (Lucas, 1973). When the arm is elevated in the sagittal plane, abduction is accompanied by medial rotation due to tightness in the coracohumeral ligament (Gagey, Bonfait and Gillot, 1987). No rotation is required for elevation in the scapular plane (30–45° anterior to the frontal plane). In this position, the joint capsule does not undergo torsion, and the deltoid and supraspinatus are optimally aligned.
Stage (II)
By the beginning of stage (II), from 30° of abduction, the scapula should be upwardly rotating to maintain clearance between the acromion and the approaching greater tuberosity of the humerus. Scapular rotation in the beginning of stage (I) occurs as a result of elevation of the clavicle on the SC joint. Between 80 and 140° the instantaneous axis of rotation (IAR) migrates towards the AC joint along the upper central scapular area. Movement then occurs as elevation of the clavicle on the SC joint, and rotation of the scapula on the clavicle at the AC joint. More movement occurs at the glenohumeral joint than at the scapulothoracic joint. Ratios of 2 : 1 are normally quoted, giving 120° of movement at the glenohumeral joint and 60° at the scapulothoracic joint in a total abduction range of 180°. However, some authors (Lucas, 1973) have argued that the ratio is closer to 5 : 4 or 3 : 2 after phase (I) of abduction.
Scapular rotation occurs as a result of force-couples between the various muscles attached to the scapula (Fig. 17.4). Upward (lateral) rotation accompanying shoulder joint abduction or flexion is brought about by contraction of the upper and lower fibres of trapezius and the lower portion of serratus anterior. Serratus anterior is probably the most important of the group. It has two sets of fibres. The fibres of the upper portion run horizontally and slightly upwards, while those of the lower portion are aligned downwards. Both sets pull powerfully on the scapula, anchoring it to the ribcage and causing scapular upward rotation as trapezius lifts the lateral end of the clavicle and acromion process. If serratus anterior and the lower fibres of trapezius are ineffective, the upper trapezius will dominate the movement. In this case, these fibres show increased tone and can be tight. As the abduction moves further into stage (II), the moment arm of lower trapezius is lengthened and this portion of the muscle becomes increasingly active in the movement.
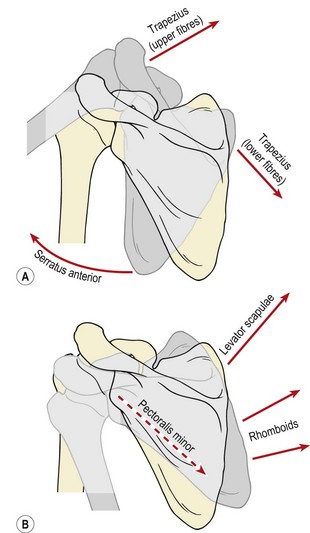
Figure 17.4 Muscle force couples which create scapular rotation. (A) Lateral rotation. (B) Medial rotation.
From Palastanga, Field and Soames (1989), with permission.
The biomechanics of throwing
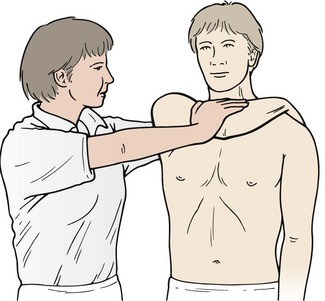
Screening examination of the shoulder complex
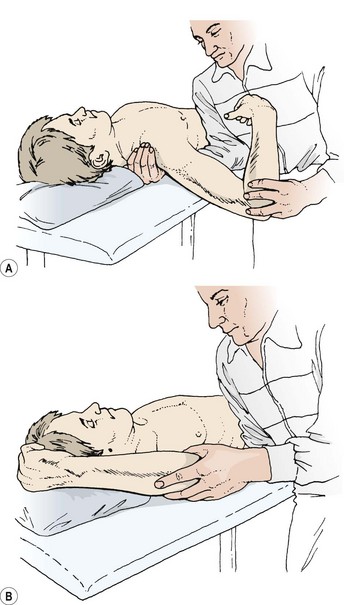
After a subjective history has been taken, a screening examination is performed to enable the examiner to focus more closely on the injured area. The patient’s posture and actions are noted while undressing, and the area is inspected for swelling, colour and deformity. A combination of active, resisted and passive movements are used to assess the shoulder complex (Cyriax, 1982). The patient is viewed from behind to note any alteration in scapulohumeral rhythm. It is helpful to have the patient facing a full length mirror, so the anterior aspect of the shoulder and the patient’s facial expression may also be assessed. Active abduction and flexion–abduction are performed with overpressure applied at end-range, to assess end-feel. Positional changes of the scapula, either at rest or during movement, warrant closer inspection. Active glenohumeral rotation may be performed by asking the patient to place a hand behind the back (medial rotation) and then behind the head (lateral rotation). Passive lateral rotation is performed with the elbow flexed and upper arm held into the side. This is also the position for resisted lateral and medial rotations. Passive medial rotation is performed with the patient placing a hand into the small of the back. The examiner stabilizes the upper arm, and keeps the patient’s elbow tucked into the side of the body. The examiner then gently pulls the patient’s forearm away from the body, increasing medial rotation. Any limitation of movement is noted, and the percentages of limitation relative to each other reveal if a capsular pattern exists. The capsular pattern for the glenohumeral joint is gross limitation of abduction with some limitation of lateral rotation and little limitation of medial rotation.

Figure 17.6 Angular displacement of the shoulder during a throwing action.
After Fleisig, Dillman and Andrews (1994), with permission.
Locking test and quadrant test
Should movement apparently be full and painless at the glenohumeral joint, two further procedures are useful to reproduce the patient’s symptoms. These are the locking test and the quadrant position (Maitland, 1991). Both tests refer to the position of the greater tuberosity relevant to acromial arch and glenoid (Corrigan and Maitland, 1994). Each should be assessed for pain and end-feel, and compared with the uninjured side.
Locking test
The locking position combines internal rotation, extension and abduction of the shoulder with the scapula fixed. In this position the subacromial space is compressed and will give pain should an impingement syndrome be present. Cadaveric studies have shown that in the locking position the posterosuperior tip of the glenoid is in contact with the humeral head (Mullen, Slade and Briggs, 1989).
Keypoint
The locking position compresses the subacromial space and gives pain with an impingement syndrome.
Quadrant test
The quadrant position stresses the anterior and inferior capsule, and combines external rotation, slight flexion and full abduction of the shoulder. The therapist’s forearm grips the patient’s shoulder to prevent shrugging. The action is to hold the elbow and move the patient’s arm into abduction, allowing the humerus to move from medial rotation (palm to chest) to lateral rotation (palm to ceiling). The point at which the humerus begins to change from medial to lateral rotation marks the beginning of the quadrant (Petty and Moore, 2001). From this point horizontal extension is examined by pressing the elbow to the floor, releasing it and then moving into further abduction before pressing again. Both the quality and the range of motion are assessed, as well as the occurrence of muscle spasm. The affected shoulder is compared to the unaffected side.
Sternoclavicular joint
The sternoclavicular (SC) joint provides, via the clavicle, the only structural attachment of the scapula to the rest of the body (Norkin and Levangie, 1992). The joint performs functionally as a ball and socket. The medial end of the clavicle articulates with the clavicular notch of the sternum, and the adjacent edge of the first costal cartilage. The congruity of the joint is enhanced by the presence of an interarticular fibrocartilage disc, which separates the joint cavity into two. In addition to improving the congruity of the joint, the disc also provides cushioning between the two bone ends. Furthermore, it holds the medial end of the clavicle against the sternum, preventing it moving upwards and medially when pushing actions are performed.
Injury
Injury to the SC joint is unusual, forming about 3% of all shoulder girdle trauma. Anterior dislocations occur more commonly than posterior dislocations in a ratio of 20 : 1 (Zachazewski, Magee and Quillen, 1996). Normally, the clavicle will fracture or the acromioclavicular joint will give way before the SC joint is seriously injured. However, when damage does occur, it is frequently the result of direct lateral compression of the shoulder, such as occurs when falling onto the side of the body. The injury is more common in horse-riding and cycling where sufficient force is produced, but is seen in rugby and wrestling.
Posterior dislocations, even if successfully reduced, will still require hospital referral and observation. Posterior dislocations usually stay reduced, but anterior dislocations are apt to recur. Surgical fixation of anterior dislocation is possible, but the number of complications makes the procedure undesirable. Migration of a Steinmann pin or Kirchner wire into the heart or major vessels has been reported (Garrick and Webb, 1990). Rockwood and Odor (1989) reported excellent results following conservative management of atraumatic anterior displacement 8 years after initial treatment. Patients treated surgically (not by these authors) in the same study had complications including scarring, instability, pain and limitation of activity.
Even though the joint is frequently hypermobile, joint mobilizations may be used to relieve pain (Maitland, 1991). Anteroposterior gliding may be performed with the therapist placing his or her thumbs over the sternal end of the clavicle.
Acromioclavicular joint
Examination
The cross body test has been shown to gap the AC joint by an average of 6.4 mm measured using ultrasonography compared to a gap of 7.7 mm with passive end range external rotation. However, greater direct stress is placed on the AC joint using the cross body manoeuvre than with humeral rotation (Park, Park and Bae, 2009). The cross body test has been shown to have a sensitivity of 77% compared to 41% for the active compression test (Chronopoulos et al., 2004). This latter test was designed to assist the diagnosis of labral tears and to differentiate them from AC joint involvement depending on the patient’s description of their pain location as ‘on top’ or ‘inside’ the shoulder (Brian et al.: O’, 1998).
Injury
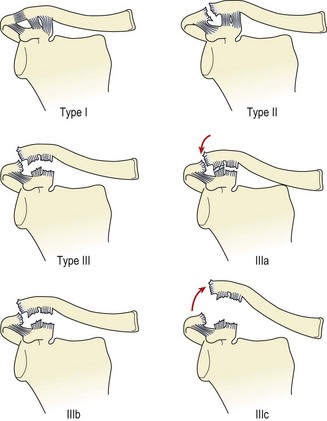
The most common conditions affecting the AC joint are sprains and degeneration. AC joint sprains vary in intensity between minor grade I injuries to grade III ruptures representing complete disruption of the coracoclavicular ligament and AC joint dislocation (sprung shoulder) (Fig. 17.11). The injury may be further classified using weight-lifting radiographs. Here, the anterior deltoid is contracted by having the patient hold a weight with the elbow flexed and arm next to the body. If the clavicular attachment of the deltoid is intact, the joint may reduce as weight is taken (IIIa), or there may be no change in the joint appearance (IIIb). However, if the lateral end of the clavicle becomes more prominent, the clavicular attachment of the deltoid may have been stripped off (Dias and Gregg, 1991). Radiographs are also used to differentiate the condition from fractures of the distal clavicle where this is suspected.
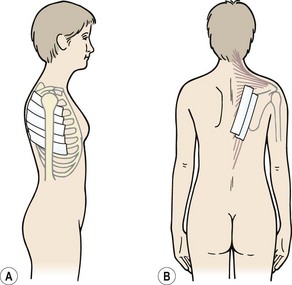
Acromioclavicular taping
Stress may be taken off the AC joint by a simple taping designed to press the clavicle down and take some of the weight of the arm away from the distal shoulder structures (Austin, Gwynn-Brett and Marshall, 1994; Macdonald, 1994). The athlete is positioned in sitting at the side of the couch with the elbow flexed to 90° and the shoulder abducted to 30°. The shoulder is slightly elevated and the arm rests on the couch. The shoulder and chest on the injured side of the body should be shaved of long hair. Spray adhesive is applied, making sure that the athlete turns the head away from the spray and covers the eyes with the unaffected hand. Also, the nipple area must be protected with a non-adhesive pad.
A felt pad is placed over the acromion to protect it from abrasion. Two anchors of 7.5 cm elastic adhesive tape are applied. The first runs horizontally from the sternum to the paravertebral area on the side of injury. The second is placed around the mid-humerus with light tension, ensuring that the limb is not excessively compressed (Fig. 17.12A). Two stirrups of 7.5 cm elastic adhesive tape are placed (pre-stretched) from the front to the back of the chest anchor, passing over the acromion (Fig. 17.12B). These are then reinforced by two strips of 5 cm zinc oxide taping. Two further strips of elastic adhesive tape are placed (pre-stretched) laterally from the arm anchor across the anterior aspect of the shoulder to join the chest stirrups over the acromion, and laterally from the anchor, passing posteriorly over the shoulder to the acromion (Fig. 17.12C). Again, these stirrups are reinforced by 5 cm zinc oxide taping. If the shoulder stirrups have been applied correctly, their tension will tend to lift the arm into abduction slightly. The chest and arm stirrups are closed by reapplying the chest and arm anchors (7.5 cm elastic adhesive tape) to act as fixing strips. Sensation and pulse should be re-tested after tape application.
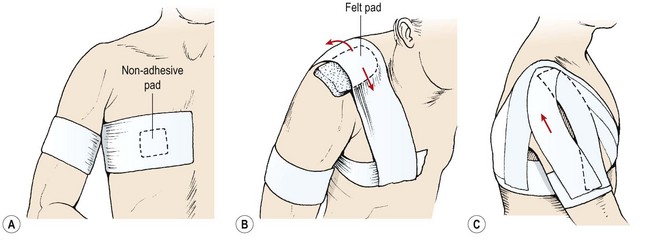
Figure 17.12 Acromioclavicular joint taping. (A) Anchors. (B) Stirrup applied under tension. (C) Arm stirrups.
Surgical intervention
There is some controversy concerning the treatment of this condition. Both conservative and surgical approaches restore function to a similar degree (Larsen, Bjerg-Nielsen and Christensen, 1986; Dias et al., 1987; Bannister et al., 1989), and some surgical methods have been shown to give long-term functional detriment. Certainly, removal of the distal end of the clavicle (Gurd, 1941) will disrupt the acromioclavicular ligament, a main stabilizer of the joint (Fukuda et al., 1986). In the literature, the main argument for surgery has been the development of degenerative changes in the joint as a result of non-operative management. However, degeneration does not occur in all patients, and when it does occur, it is not necessarily a limitation (Dias et al., 1987). In addition, surgery is often as effective if done in the acute or chronic condition, so there is normally no advantage to operating immediately. Importantly, surgery carries with it a high risk of complications (Ejeskar, 1974; Lancaster, Horowitz and Alonso, 1987; Taft, Wilson and Oglesby, 1987).
In a literature review of 11 papers detailing the long-term results of both surgical and conservative management of this injury, Dias and Gregg (1991) found poor results to have occurred in 13 out of 247 patients treated conservatively (5.3%), and 22 out of 233 managed surgically (9.4%). These authors argued that as comparable results were obtained regardless of the method used, conservative management was the treatment of choice for most AC injuries. Looking at strength testing following grade III AC injuries treated conservatively (average 4.5 year follow-up), Tibone, Sellers and Tonino (1992) found no subjective complaints in patients, all of whom were able to participate in sport. Full motion occurred in all subjects, and no significant differences were found in muscle strength of injured and non-injured sides in rotation, abduction/adduction or flexion/extension.
AC joint degeneration
Joint degeneration is common in later years following injury, regardless of the grade of damage which occurred, and particularly after repeated trauma. In addition, some sports, such as weight-lifting, have a higher incidence of degenerative changes in the AC joint, even where no incidents of trauma may have occurred. Cahill (1982) reported 46 cases of osteolysis of the distal clavicle, all but one occurring in weight-lifters. He argued that degeneration occurred as a result of subchondral stress fractures resulting from repeated microtrauma. The condition presents as pain, usually dull and aching in nature, brought on by activities such as lifting and throwing. On examination there is point tenderness over the joint, with pain and crepitus to passive horizontal adduction (cross body test).
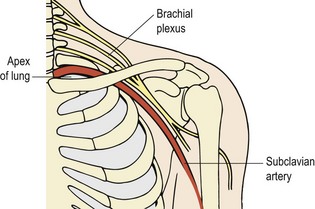
Fractures of the clavicle
The most common mechanism of injury is a fall onto the outstretched arm, and occasionally direct trauma to the shoulder. Although common, these injuries should not be taken too lightly, as it must be remembered that the subclavian vessels and the medial cord of the brachial plexus lie in close proximity, as does the upper lobe of the lung (Fig. 17.13). Neurovascular and pulmonary examination may therefore be required.
Distal fractures tend to be displaced by retraction immobilization, and are better wired. Internal fixation of the proximal clavicle carries with it similar complications to that of the sternoclavicular (SC) joint. Fractures to the extreme proximal end of the clavicle may be misdiagnosed as SC dislocations, and in the younger individual epiphyseal injury should be considered in this region. It should be noted that the sternoclavicular epiphysis may remain open until the age of 25 (Zachazewski, Magee and Quillen, 1996), so radiological examination must be accurate.
Winged scapula
During normal scapulohumeral rhythm, the scapula slides over the ribcage, and is held in place by the serratus anterior. If weakness or paralysis of the serratus anterior occurs, the scapula will stand prominent from the ribcage when the arm is protracted against resistance. In addition to muscular weakness, there are a number of other causes including damage to the long thoracic nerve, brachial plexus injury, conditions affecting the fifth, sixth and seventh cervical nerve roots, and certain types of muscular dystrophy (Apley and Solomon, 1989).
Apparent winging may occur when the scapulae abduct through lengthening of the scapular retractors and tightening of the protractors. As the scapulae move away from the mid-line, they roll around the ribcage, lifting their medial border. This is not true winging, however, because the condition is present at rest and during muscle contraction. Treatment note 17.1 shows exercise therapy and manual therapy techniques used in the restoration of scapulothoracic stability.
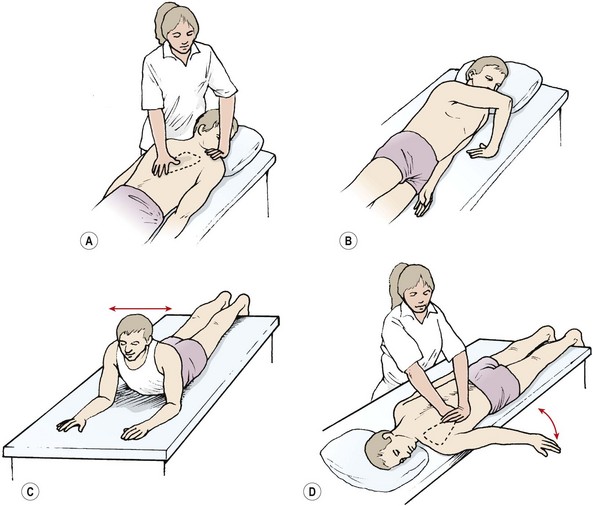
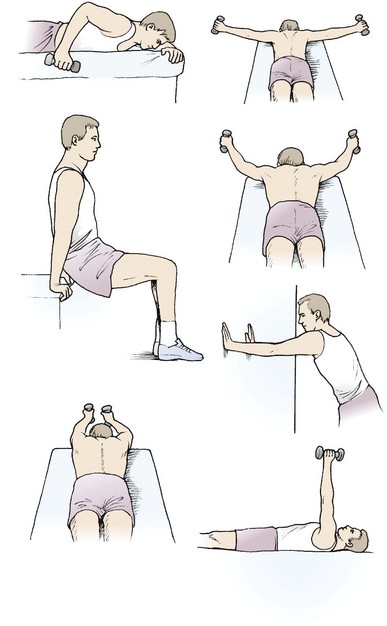
Treatment note 17.1 Restoraton of scapulothoracic stability
Scapular stability is enhanced by restoring the functional capacity of the lower trapezius and serratus anterior, which, as stability muscles, often show reduced activity and lengthening. Surface electromyography (sEMG) may be used with the active electrode placed over the lower trapezius or serratus anterior. The patient is placed in prone lying and the scapula is passively positioned into its neutral position by the therapist. This often requires retraction and depression to neutralize the protraction/elevation often found (Fig. 17.14). The patient is encouraged to hold this position through his or her own muscle activity, gaining feedback from the sEMG readout. Enough muscle activity should be used to keep the anterior aspect of the shoulder off the treatment couch, but not to retract the scapulae. Once this position can be maintained actively, the holding time is built up until the patient can perform 10 repetitions, holding each for 10 seconds.
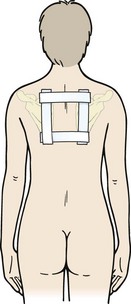
Taping may be used to give feedback about the position of the scapula and lengthened muscle. A positional box tape may be used to facilitate position of the scapula (Fig. 17.15). The tape has two horizontal strips to draw the medial borders of the scapulae together and two vertical strips to facilitate thoracic extension. Non-elastic taping is used to take up skin tension and act as a feedback system for the patient. Facilitatory taping may be used over the serratus anterior (Fig. 17.16A), lower trapezius (Fig. 17.16B) or to increase patient awareness of body segment position and facilitate underlying muscle action.
The scapular force couples may be maximally challenged using a side lying, braced position (Wilk and Arrigo, 1993). The patient begins in side lying with the arm flexed/ abducted to 90° and internally rotated. The hand is now flat on the couch with the fingers pointing towards the patient. Scapular fixation is maintained against the rhythmic stabilization provided by the therapist in all planes.
The scapulothoracic muscles may be selectively strengthened using the individual exercises shown in Figure 17.17.
Impingement syndrome
The subacromial space (Fig. 17.18) lies beneath the coracoacromial arch formed by the coracoacromial ligament together with the coracoid and acromion the so-called ‘roof of the joint’. The coracoacromial arch is covered by the deltoid, and inferiorly its fascia is continuous with that of the supraspinatus. The arch prevents upward dislocation of the glenohumeral joint. The supraspinatus passes beneath the arch, being separated from it by the subacromial bursa. The subacromial distance (space between the inferior acromion and the head of the humerus) is normally about 1cm (Petersson and Redlund-Johnell, 1984). If the supraspinatus tendon has ruptured, or the muscle is no longer active, this space will reduce by as much as 50% due to the unopposed pull of the deltoid.
Keypoint
The subacromial space may reduce by as much as 50% if the supraspinatus muscle is dysfunctional.
During elevation and internal rotation, the greater tuberosity, with the supraspinatus riding on top, may press against the anterior edge of the underside of the acromion (or a spur from a degenerating AC joint) causing impingement pain. During flexion, impingement may also involve the long head of biceps (Peat and Culham, 1994). At the point where the greater tuberosity comes close to the acromion (70–120° abduction), a number of structures may be pinched between the involved bones or the tuberosity and the coracoclavicular ligament. Normally, the structures affected are the suprasinatus tendon, the long head of biceps and the subacromial bursa.
Movement dysfunction
The action of abduction involves a complex series of movements. Impingement is associated with a change in the muscle action involved in the abduction sequence. Most commonly there is a reduction in the stabilizing action of the serratus anterior muscle with other muscles (especially the upper trapezius) compensating. The result is an altered scapular position relative to the humerus during abduction. This movement dysfunction has been termed scapula dyskinesia (Paterson, 2008). EMG studies of patients with impingement pain have shown a reduction in serratus anterior muscle action and a change in scapula position (Ludewig and Cook, 2000). The scapula is more anteriorly tipped drawing it closer to the approaching humeral head, and upward rotation during the early stages of abduction is delayed. Decreased force output in the both the serratus anterior and lower trapezius has also been shown with overhead athletes demonstrating shoulder impingement (Cools et al., 2004).
Examination
The screening examination is used initially, followed by observation of both static and dynamic position of the scapula and humerus. Two further tests are useful which are specific to impingement. In test one (Fig. 17.19A) the arm is fully abducted and overpressure is put onto the internally rotated (thumb forwards) shoulder. For test two (Fig. 17.19B), the glenohumeral joint is flexed and internally rotated (Hawkins test). Overpressure is then added to internal rotation and abduction or horizontal flexion. Resisting flexion by placing pressure over the elbow may also bring on the athlete’s pain (Hawkins and Hobeika, 1983; Reid, 1992).
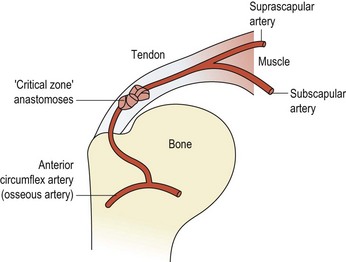
In addition to a purely mechanical impingement, changes in the microvascular supply to the area have been noted. Pressure exerted by the humeral head on the supraspinatus tendon, has the effect of ‘wringing out’ the tendon vessels and creating an avascular zone (Rathbun and Macnab, 1970). This area, known as the critical zone (Fig. 17.20), is an anastomosis between the osseous vessels and the tendinous vessels (Moseley and Goldie, 1963). Furthermore, repeated microtrauma results in local oedema within the tendon and an increase in tissue volume. This in turn makes the structures more susceptible to impingement by reducing the subacromial space and so perpetuates the problem.
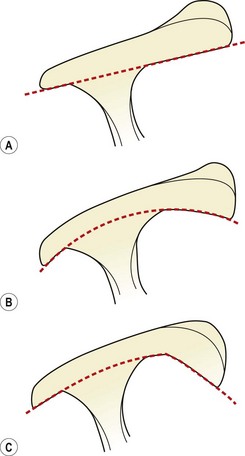
A reduction in the subacromial space may be the result of individual variation in the anatomical architecture of this region, with some individuals more prone to impingement than others (Ticker and Bigliani, 1994). Cadaveric studies of 140 specimens have identified three types of acromion associated with full thickness tears of the rotator cuff (Bigliani, Morrison and April, 1986).
The flat (type I) acromion occurred in 17% of subjects, the curved (type II) acromion was seen in 43%, and the hooked (type III) type in 39% (Fig. 17.21). The hooked acromion was present in 70% of rotator cuff tears whereas the flat type was only seen in 3%. By assessing the supraspinatus outlet view x-ray, Morrison and Bigliani (1987) showed 80% of those with positive arthrograms to have a hooked acromion. The same authors showed that 66% of patients who underwent open subacromial decompression had a hooked acromion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree