CHAPTER 15 The cervical spine
The cervical spine consists of eight mobile segments generally categorized into two functional units. The first comprises the occiput, C1 and C2 (the suboccipital region) and the second the segments from C2 to T1 (the lower cervical region) (see Fig. 5.33).
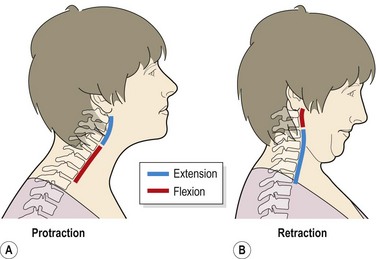
Within the total range of any cervical movement some regions move more than others. The upper cervical segments allow more rotation than the lower, but less lateral flexion. With head retraction the upper segments flex while the lower ones extend (Fig. 15.1). In fact, with this movement a greater range of upper cervical flexion is obtained than with neck flexion itself (McKenzie, 1990). As flexion occurs, the spinal canal lengthens, stretching the cord and nerve roots. Extension reverses this effect relaxing the spinal structures.
Treatment note 15.1 Surface marking of the cervicothoracic region
Cervical vertebrae
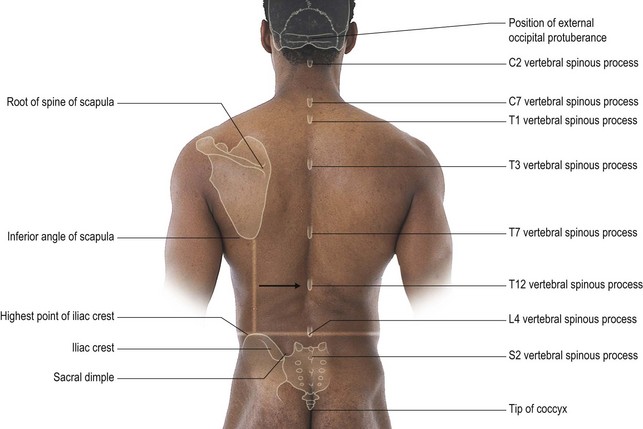
Most of the spinous processes of the vertebrae may be readily palpated (Fig. 15.2). Palpation is facilitated by having the patient draw their chin in and look down slightly (upper cervical flexion). The prominent point on the back of the skull is the external occipital protuberance (EOP), and below this the external occipital crest.
Moving the finger sideways, the mastoid process may be palpated behind the ear.
Ribs
Anteriorly the costal cartilages of the 8th, 9th and 10th ribs merge to join the sternum at the xiphoid process; the ends of the 11th and 12th ribs are free, hence the name ‘floating ribs’. The sternum itself is easily palpated on the anterior chest wall. Superiorly the suprasternal notch is found, and further down the manubrium (upper portion of sternum) joins the main body of the sternum at the sternal angle. The sternal angle is slightly flexible, exhibiting 5−7° of motion between full inspiration and full expiration (Field and Hutchison, 2006). The 2nd rib attaches to the sternum at this level, and the 7th rib is level with the xiphoid process.
Vertebral arteries
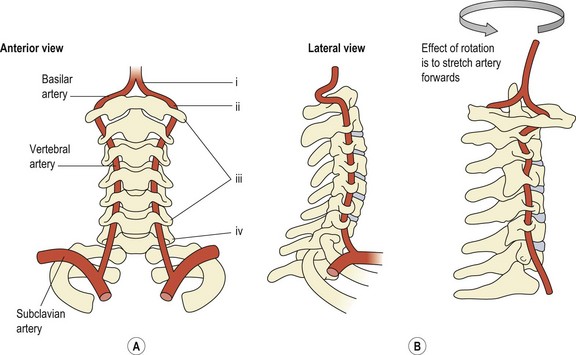
One important difference between the cervical and other spinal areas is the presence of the vertebral arteries. These branch from the subclavian artery (Fig. 15.3A (i)) and pass through the foramina transversaria of each cervical vertebra from C6 and above (Fig. 15.3A (ii)). When the artery reaches the atlas, it runs almost horizontally (Fig. 15.3A (iii)) and then enters the foramen magnum to join with its neighbour and form the basilar artery (Fig. 15.3A (iv)). The vertebral arteries supply about 11% of the cerebral blood flow, the carotid system supplying 89% (Grant, 1994a).
Variations in the diameter of the vertebral arteries are common, and in some cases the basilar artery is supplied almost entirely by one dominant vertebral artery (Bogduk, 1986). During its course, the artery is in close relation to a number of structures, including the scalenus anterior and longus colli muscles, the uninate processes, the superior surface of the facet joint, and of course the transverse process itself.
Vertebrobasilar insufficiency (VBI) may occur with occlusion, in which case the predominant symptom is dizziness, although other symptoms may be seen (Table 15.1). Occlusion may be either intrinsic or extrinsic. Intrinsic causes include atherosclerosis blocking the artery, causing either focal narrowing, or more extensive constriction over the whole length of the artery. Extrinsic causes of occlusion occur by compression to the vessel wall. This is most commonly caused during rotation of the neck if an anomaly of the artery exists. Three such anomalies have been described in the lower part of the artery (Bogduk, 1986). First, an irregularity in the origin of the artery from the subclavian, secondly, bands of deep cervical fascia crossing the artery which tighten on rotation, and thirdly squeezing of the artery within the fascicles of either longus colli or scalenus anterior.
Table 15.1 Symptoms of vertebrobasilar insufficiency (VBI)
From Grant (1994b), with permission.
The major vertical portion of the artery (Fig. 15.3A) is most commonly affected by osteophytes and adhesive scar tissue, with neck rotation compromising the ipsilateral vessel. In the upper region (Fig. 15.3B), the artery may be occluded should the atlas move on the axis, through trauma, rheumatoid arthritis or abnormalities of the odontoid. Passive rotation of the neck can shut the contralateral artery by stretching it (Brown and Tatlow, 1963). Extension reduces cerebral blood flow less than rotation, but combined rotation–extension in the presence of traction increases the rate of occlusion significantly (Brown and Tatlow, 1963).
Vertebrobasilar insufficiency is a potential danger of any manual therapy to the neck, particularly rotation, with some 60 cases of stroke being reported following neck manipulation (Bogduk, 1986). Twenty-six cases reported in one series were subjected to x-ray following the incident. Of these, 23 were reported as normal or showing only minor degenerative changes (Grant, 1994b). In addition, major vascular complications occur predominantly in young (35–40 years) adults, suggesting that bony degenerative changes are not responsible for VBI. Trauma following manipulation occurs predominantly in the atlantoaxial component of the artery, which is stretched forwards during rotation. The more mobile neck of a younger adult will allow a greater range of rotatory motion and therefore greater stretch. Mechanical stress to the vertebral artery may lead to spasm (transient or persistent), subintimal tearing, perivascular haemorrhage or embolus formation leading to brainstem ischaemia. Repeated rotatory manipulation is especially dangerous as it builds on trauma which may already have occurred. In the UK between 1995 and 2003, 300 patients had adverse effects from cervical manual therapy with the most frequent incident being stroke (Ernst, 2004). Injury occurs typically through dissection of the internal carotid artery (ICA) or vertebral artery (VA) and may include cerebral ischaemia, stroke or death (Kerry et al., 2008).
Pre-manipulative testing of the cervical spine
Testing for VBI should be carried out for all patients undergoing cervical manipulation (APA, 1989, 2006; Grant, 1994a, 1994b). Aspects of these tests (especially subjective history) will be relevant for all manual therapy procedures. Initially, subjective examination is used to determine the presence of dizziness or other symptoms suggesting VBI. The frequency of these symptoms and aggravating and alleviating factors are noted, especially with relevance to the neck. Any previous treatment (particularly multiple rotatory manipulation or manipulation under strong axial traction) is noted.
Physical examination includes sustained movements (10 s or less if symptoms are provoked) of extension, rotation, and combined extension/rotation (Table 15.2). Where there is no history of VBI, the patient is positioned in a simulated manipulation position which is again sustained. If the subjective examination suggests dizziness, the position which provokes this symptom is used in a sustained fashion. In addition, rapid head movement is used to distinguish between dizziness due to VBI and that due to vestibular origin. This is especially relevant where the patient describes rapid movement as a precipitating factor in the subjective examination. The therapist holds the patient’s head (but not covering the ears) and body rotation is performed (for example in a swivel chair, or trunk twisting in standing) to both sides and held for 10 seconds. As the head itself is not moving, any symptoms are due to cervical rotation rather than vestibular disturbance.
Table 15.2 Physical examination for vertebrobasilar insufficiency (VBI)
| No history of VBI | History of VBI (dizziness) |
|---|---|
| Sustained extension | Sustained extension |
| Sustained rotation (left and right) | Sustained rotation (left and right) |
| Sustained rotation with extension (left and right) | Sustained rotation with extension (left and right) |
| Simulated manipulation position | Test position or movement which provokes dizziness Rapid movement of relevant head position within available range |
After Grant (1994b).
Measurement of vertebral artery blood flow using ultrasound can also be a useful clinical tool (Johnson et al., 2000). Reliability is high when testing the vertebral artery at C5–C6 level singly (volume flow rate) and using a mean of three tests at C1–C2 (peak velocity).
Keypoint
The clinical guidelines for assessing VBI in the management of cervical spine disorders are available to download free of charge at the Australian Physiotherapy Association website on http://www.physiotherapy.asn.au/images/Document_Library/Clinical_Guidelines/guidelines%20spine%20disorders.pdf
Testing for VBI has been critisized on a haemodynamics basis. Tests have been shown to alter blood flow within the VA and ICA, but changes in blood flow do not correlate well with VBI symptoms (Kerry et al., 2008). Subjective examination of the patient must therefore be used to support VBI manual assessment, and should focus on determining the presence of dizziness and associated symptoms shown in Table 15.3.
Table 15.3 Subjective examination prior to cervical manual therapy
From Rivett et al. (2006).
Nature of cervical injury in sport
The most common mechanism of severe cervical injury is axial loading (Torg et al., 1985). This may be caused as a player hits another by using his or her head as a battering ram (spearing), or if the athlete falls on to his or her head or runs into an object head-first. In this situation, the neck is slightly flexed, flattening the cervical lordosis. Now, the cervical spine absorbs considerably less energy than it would in its normal state as a flexible column. Initially, maximal discal compression occurs, and then the spine rapidly buckles and fails in flexion, resulting in fracture, subluxation or dislocation.
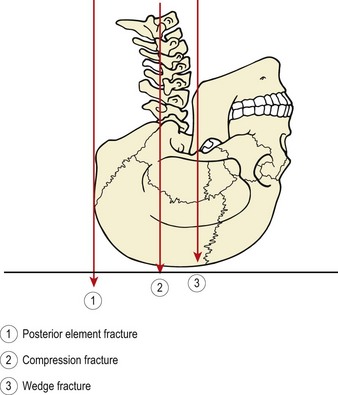
The contact area of the axial load on the skull can determine the nature and extent of cervical injury (Winkelstein and Myers, 1997). Where the contact area is on the skull vertex, compression and cervical crush injury is likely to occur even at slow velocities. The trunk continues to move while the head motion is abruptly stopped through ground contact. Where the ground contact area is at a distance from the skull vertex, the head will be forced into flexion or extension – the so called ‘escape direction’. In this case direct compression along the length of the neck is reduced through cervical flexibility. Posterior element fracture more commonly occurs where force is directed behind the vertebral body while direct compression forces acting through the vertebral body give rise to compression fracture. Anterior burst or wedge compression fractures occur where the cervical spine is forced into extension (Fig. 15.4).
An illustration of the importance of this mechanism and its preventive possibilities is found in American football. The incidence of cervical quadriplegia in this sport dropped dramatically from a peak of 34 cases per year to 5 since head-first tackling and blocking were forbidden with the aim of reducing axial load injury (Torg et al., 1985).
A similar mechanism has been described in rugby football. Cord injuries have occurred in scrum, ruck and maul situations when a player was attempting to pick the ball up from the ground (Silver and Gill, 1988), and as two forwards engage (Taylor and Coolican, 1987). The vertex of the head is restrained, either against another player or the ground, and the trunk continues to move forwards forcing the cervical spine into flexion and dislocation (McCoy, Piggot and Macafee, 1984).
In ice hockey, axial loading is again the culprit, when a player hits the boards or an opponent with his helmeted head while the neck is slightly flexed (Tator and Edmonds, 1986).
Where significant axial loading has occurred, permanent abnormalities exist within the cervical spine (Torg et al., 1993). These may include interspace narrowing at C5–C6 with deformity of the C5 end plate due to Schmorl’s node formation. In addition, reversal of the cervical spine lordosis with fixation from C2 to C6 may be seen. Where these changes are present, they should preclude an athlete from participation in sports involving collision activities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree