CHAPTER 14 The thorax and thoracic spine
Thoracic spine
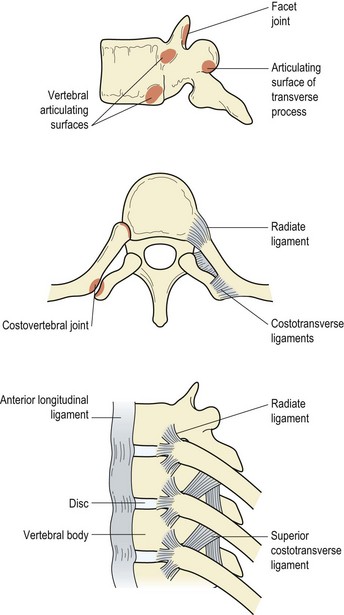
The unique feature of the vertebrae in the thoracic region is the presence of facets, both on the sides of the vertebral bodies and the transverse processes. These are for articulation with the ribs, forming the costovertebral and costotransverse joints (Fig. 14.1). Most of the ribs articulate with two adjacent vertebral bodies and one transverse process. The facets on the head of the ribs articulate in turn with demi-facets on the upper and lower borders of the vertebrae, and the crest on the rib head butts onto the intervertebral disc. The joint capsule is loose and strengthened anteriorly to form the three portions of the radiate ligament. The costovertebral joint cavity is divided into two by the intra-articular ligament, except for ribs one, ten, eleven and twelve which articulate with a single vertebra and have a single joint cavity.
Rib movements
Ribcage shape at rest
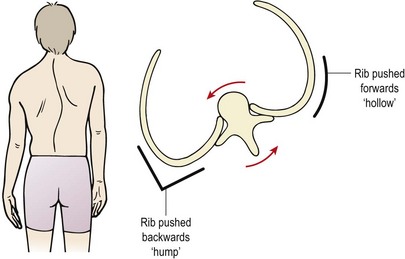
The ribcage will also alter shape in cases of scoliosis. The vertebral bodies rotate towards the convexity of the curve, dragging the ribs with them. The ribs on the convex side of the curve are pushed backwards creating a ‘hump’ and those on the concave side of the curve move anteriorly causing a ‘hollow’ (Fig. 14.2). Rotation of the vertebral body causes the spinous processes to move away from the mid-line, in the opposite direction to the scoliosis. Right rotation of the vertebra therefore sees the spinous process deviating to the left.
Examination
Palpation takes in the vertebrae, rib joints and ribs themselves, and is carried out with the patient in a prone position with the arms over the couch side to move the scapulae apart. Alternatively, posteroanterior (PA) pressures may be used with the thoracic spine extended using the elbow support prone-lying starting position. In a prone-lying position the spinous processes of the thoracic vertebrae are angled downwards like the scales of a fish. The thoracic vertebrae may be considered in threes, with the transverse processes being found relative to the spinous processes as shown in Table 14.1.
Table 14.1 Palpation of the thoracic vertebrae
| T1, 2, 3 | At the same level as spinous process |
| T4, 5, 6 | Between two successive levels |
| T7, 8, 9 | Level with spinous process of vertebra below |
| T10 | Level with vertebra below |
| T11 | Between two successive levels |
| T12 | At same level |
The rib angles gradually spread out from the spine with the eighth rib being furthest (about 6 cm) from the mid-line. The rib angles can be palpated at the same levels as the transverse processes down to the T8/T9, by pushing the soft tissue to one side. The facet joints lie in the paravertebral sulci, and the transverse processes, which overlie the costotransverse joints, are found 3–4 cm from the mid-line. Guidelines for rib palpation are shown in Table 14.2.
| Rib structure | Region of palpation |
|---|---|
| 1st rib | Above clavicle, within supraclavicular fossa |
| 2nd | End level with manubriosternal joint (angle of Louis) |
| 4th | Lies on nipple line |
| 7th | End level with xiphisternal joint |
| 11th | Tip lies in mid-axillary line |
| 12th | Tip level with L1 |
| Rib angle | 3–4 cm lateral to end of transverse process |
| Costochondral (CC) joint | 3 cm lateral to parasternal line at 2nd rib, 12 cm lateral at 7th rib, 18 cm lateral at 10th rib |
| Costotransverse (CT) joint | Depression between transverse process and rib |
Modifications to the slump test for the thoracic spine
A variation of this test for the cervical and thoracic spine is to perform it in the long sitting position (Fig. 14.3A). From this position thoracic and lumbar flexion are added followed by cervical flexion (Fig. 14.3B). Altering the order of movement will change the neurodynamic demands (Butler and Slater, 1994), enabling the practitioner to refine the test. For example, performing cervical flexion before lumbar and thoracic flexion will challenge the cervical neural tissues more. The test can be further refined to place emphasis on the sympathetic trunk (Slater, Butler and Shacklock, 1994). This is especially relevant in the presence of sympathetic signs in conditions such as T4 syndrome, thoracic outlet syndrome and Raynaud’s syndrome, and in cases where cervicothoracic conditions mimic cardiac disease. Sympathetic testing is achieved by adding components of lateral flexion and rotation of the thoracic spine and lateral flexion of the cervical spine. Additional stress may be imposed by adding a minimal straight leg raise (SLR).
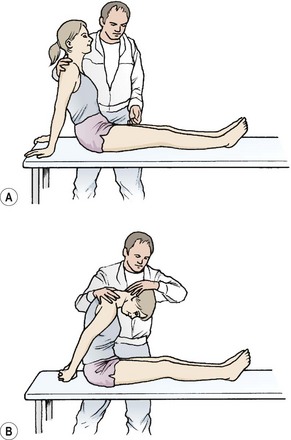
Figure 14.3 The slump test (long sitting). (A) Start. (B) Finish.
From Butler (1991) with permission.
Injury to the ribcage
Rib fracture
With rib fracture it is the tearing of the intercostal muscles which gives the pain rather than the fracture itself (Cyriax, 1982). The acute pain may be relieved by local strapping. Pre-stretched elastic adhesive strapping is applied across the area to restrict ribcage expansion and give the athlete a feeling of support. In the subacute phase active mobilization is required. If scar tissue formation is excessive and the source of pain, transverse frictions to the intercostal muscles along the line of the ribs are helpful. In addition, holding the rib down with the fingertips and practising deep inspiration will help to stretch the injured area. Exercises to expand the ribcage, such as deep inspiration and overhead reaching, or trunk lateral flexion to the contralateral side with or without rotation is also helpful to stretch the area.
First rib injury
The first is the shortest and roundest of the ribs. It slopes downwards and forwards from its attachment to the first thoracic vertebra. It forms attachment for the scalene muscles, serratus anterior, and subclavius. Its superior surface bears a deep groove for the subclavian artery (posterior) and the subclavian vein (anterior). The arterial groove is the weakest part of the rib (Gurtler, Pavlov and Torg, 1985).
Fractures of the first rib may either be traumatic or the result of overuse. Overuse injuries have been reported as a result of repeated arm movements, such as heavy lifting and pitching (Bailey, 1985; Lankenner and Micheli, 1985; Gurtler, Pavlov and Torg, 1985). Symptoms are of pain associated with deep breathing, tenderness in the root of the neck, posterior aspect of the shoulder or axilla. Often the patient hears or feels a snap in the shoulder as when performing a sudden violent movement. Range of shoulder movement will usually be full but painful, especially to extension. Accurate diagnosis by radiographs in traumatic lesions is essential because of the proximity of the major vessels, nerves and lung. Bailey (1985) recommended serial radiographs for up to 6 months after stress fracture.
Rib displacement
Movement may also be forward or backward. An anterior displacement may occur with a subluxation of the costovertebral joint, and the rib is sheared forwards. The rib will appear more prominent than its neighbour. This can occur in sport due to a blow to the back, typically when a knee hits the player on the back of the chest in rugby. A posterior displacement is more common and presents as a prominence of the rib angle. This is normally due to a blow to the chest, again from a tackle or through seatbelt or steering-wheel trauma in a road traffic accident (RTA). Management of rib displacement is by the use of muscle energy techniques (MET) and rib joint mobilization (see Treatment note 14.1).
Treatment note 14.1 Manual therapy techniques for rib displacement
Elevation
An elevated rib does not move down far enough during expiration. The aim is to encourage this movement and draw the rib down as the patient breathes out. For the 1st rib pressure is placed over the rib with the knuckle (key grip) (Fig. 14.4). The head is side flexed to relax the anterior scalene and the rib is pressed downwards with expiration. The 2nd rib is gripped within the axilla and pulled downwards as the patient exhales powerfully (Fig. 14.5). The remaining ribs may be gripped with the fingertips or pushed downwards using the knife edge of the hand (Fig. 14.6).
Depresssion
The depressed rib is bound down and stops moving upwards during inspiration. The aim is therefore to encourage further upward movement as the patient breathes in. For the 1st rib, stretch of the anterior scalenes is used (side flex the neck to the opposite side) to pull the rib upwards (Fig. 14.7). For the 2nd rib the finger or thumb pads press on the rib within the axilla (Fig. 14.8), and for the remaining ribs the thumb pad or pisiform presses on the rib undersurface within the intercostal space (Fig. 14.9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree