CHAPTER 18 The elbow
Structure and function
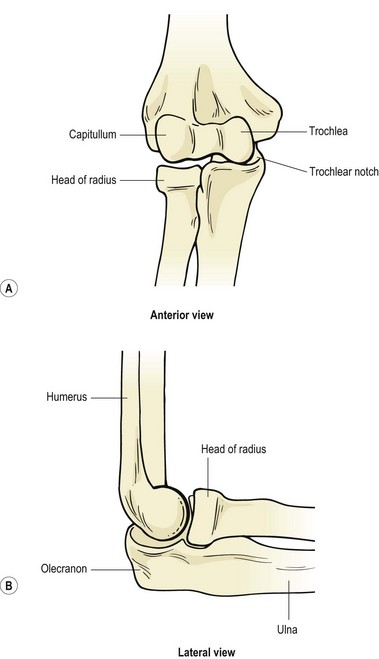
The primary purpose of the shoulder is often described as positioning the arm to facilitate hand action. The elbow, in turn, functions to shorten or lengthen the arm, largely to allow the hand to be brought to the mouth. The elbow complex consists of the humeroulnar and humeroradial articulations and the superior radioulnar joint, all of which share the same capsule (Fig. 18.1).
Bony alignment and joint contact areas
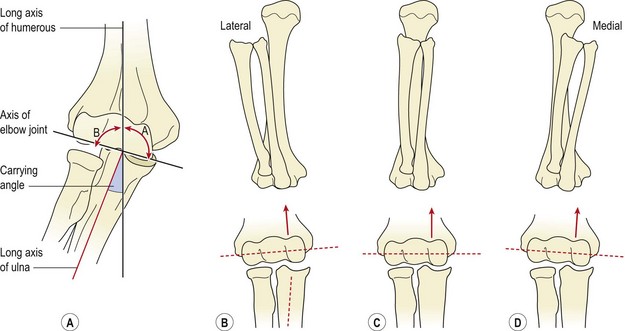
Viewed from the front, the radius and ulna are slanted laterally to the shaft of the humerus, the angulation forming the carrying angle (Fig. 18.2A). This is approximately 10–15° for men, increasing to 20–25° for women. This bony alignment means that normally, as the arm is flexed the hand moves towards the shoulder, and the radius and ulna end up in line with the humerus (Fig. 18.2C). Variations in carrying angle between individuals, mainly due to altered configuration of the trochlear groove, may occur and will alter the resting position of the radius and ulnar at full flexion (Fig. 18.2B,D). Changes in bony alignment may also occur after injury – an important factor in rehabilitation following elbow fractures.
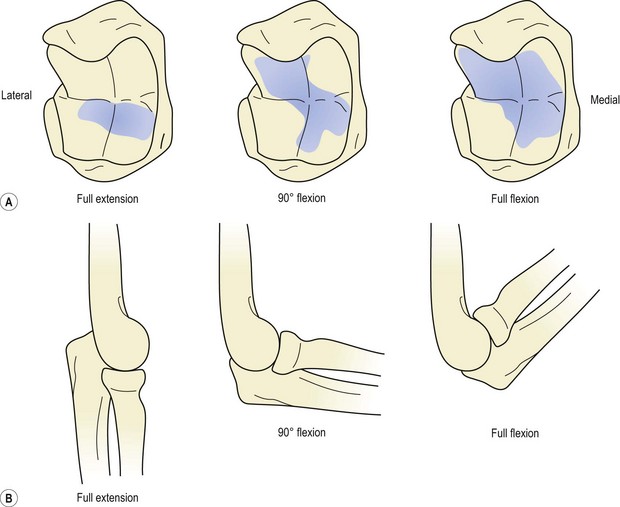
The contact area between the joint surfaces of the elbow complex increases throughout flexion. In full extension the lower medial part of the trochlear notch of the ulna is used, with no contact occurring between the radius and ulna. At 90° the contact area is a diagonal (lower medial to upper lateral) across the trochlear surface, with only slight pressure between the humerus and radial head. In full flexion definite contact occurs between the radius and ulna, and the trochlear contact areas increase (Fig. 18.3). Full flexion is thus required to ensure adequate nutrition of the whole articular cartilage, a situation sometimes not possible in obese or heavily muscled individuals due to the approximation of the flexor soft tissues.
Collateral ligaments
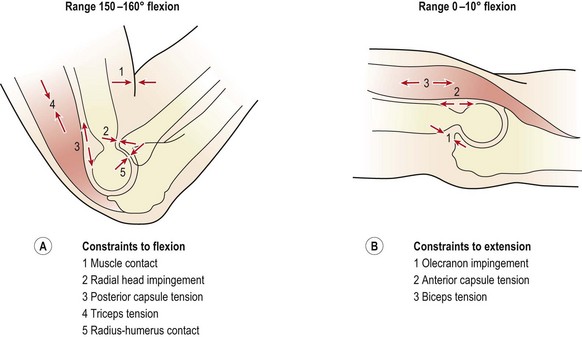
Flexion is limited by muscle contact and impingement of the radial head on to the radial fossa. In addition, tension occurs in the triceps and posterior joint capsule, and finally, in lean individuals, the shafts of the radius and humerus themselves come into contact (Fig. 18.4A).
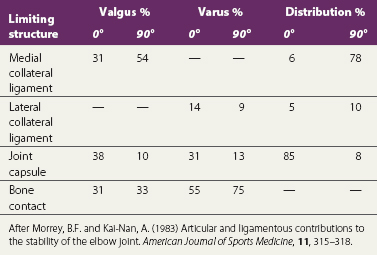
In extension, when the muscles are relaxed, valgus stability is provided by the medial collateral ligament, anterior capsule and bony configuration. As the elbow flexes, the anterior capsule relaxes, and its role is taken on by the medial collateral ligament, which provides 31% of joint stability in extension and 54% at 90° flexion (Table 18.1). In contrast, varus stress is resisted in the main by bone contact supplemented by the anterior capsule. The lateral collateral ligament only contributes 14% of the total stability of the joint with the elbow in full extension, and 9% with it flexed to 90° (Morrey and Kai-Nan, 1983). With joint distraction, the main limiting factor in extension is the joint capsule, and with the joint flexed to 90°, the medial collateral ligament. End-range is limited by a combination of the olecranon impinging into the olecranon fossa, and tension in the anterior capsule and biceps (Fig. 18.4B).
Pronation and supination of the forearm involve not just the superior and inferior radioulnar joints, but also the ulnohumeral, radiohumeral and radiocarpal joints. With pronation, the head of the radius twists on the capitulum and swings on the radial notch of the ulna, tightening the quadrate ligament. The radial head tilts, and is pulled into the capitulotrochlear groove, and the ulna moves into slight extension and abduction at the ulnohumeral joint (Lee, 1986). Consequent to this, at the inferior radioulnar joint the ulnar notch of the radius swings medially over the ulnar head. A traumatic injury to the elbow is therefore likely to affect the wrist, and, to be complete, clinical examination should include both joints.
Screening examination
Following inspection, objective examination begins with flexion and extension, each performed to full range, noting the joint end-feel. The normal end-feel to extension is hard while that to flexion is soft. Pronation and supination are performed with the elbow held to the side of the body and arm flexed to 90°. The end-feel should be springy. Further differentiation may be obtained by combining flexion and extension with abduction and adduction (valgus/varus) stresses, and by assessing gliding motions of the individual component joints of the elbow complex (Fig. 18.5). The capsular pattern is of flexion more limited than extension, and rotations relatively free.
Lateral pain
The term ‘tennis elbow’ is often used colloquially as a blanket description for any soft tissue pain between the shoulder and wrist, and there has been little agreement in the past as to the exact site of the lesion. The condition was first documented in the late 1800s when it was described as ‘lawn tennis arm’. Cyriax (1936) described 26 different lesions to which the condition had been attributed, while Lee (1986) cited 12 more general causes, as shown in Table 18.2. The terms ‘lateral’ and ‘medial tennis elbow’ have been used (Nirschl, 1986), but in this book the name tennis elbow is used to describe lateral epicondylitis while ‘golfer’s elbow’ refers to medial epicondylitis. The ratio of lateral to medial epicondylitis encountered clinically has been shown to be 7 : 1 (Leach and Miller, 1987).
Table 18.2 General causes of tennis elbow
From Lee, D.G. (1986) Tennis elbow: a manual therapist’s perspective. Journal of Orthopaedic and Sports Physical Therapy, 12(2), 81–87. With permission.
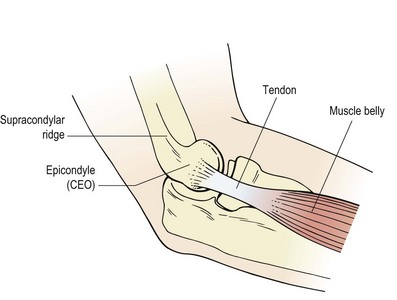
Tennis elbow (lateral epicondylalgia) is a lesion to the common extensor origin (CEO), with the primary site being the tendon of extensor carpi radialis brevis (ECRB) and/or the extensor carpi radialis longus (ECRL). ECRL attaches to the lateral supracondylar ridge (lower third) and travels to the base of the 2nd metacarpal, while ECRB attaches more distally to the lateral epicondyle itself via the common extensor tendon where it spreads onto the lateral ligament of the elbow. From here the muscle inserts into the base of the 3rd metacarpal. When testing for tennis elbow (see below) the muscles may be differentiated by placing resistance over the 2nd and 3rd metacarpals. Pain with rested middle finger extension (3rd metacarpal) suggests ECRB. Most commonly, the injury is at the tenoperiosteal junction of the tendons, but scar tissue may form onto the tendons themselves or the musculotendinous junction (Fig. 18.6).
Pathophysiology
The pathological features of tendinopathy have been covered in previous chapters for the Achilles (Chapter 10), patellar tendon (Chapter 9) and rotator cuff (Chapter 17). In the case of tennis elbow local tendon pathology is that of immature and dysfunctional healing called angiofibroblastic hyperplasia. This process has four key elements: (i) Collagen cell numbers and the amount of ground substance increase, (ii) vascular hyperplasia (neovascularization) is seen, (iii) there is an increase in the concentration of local neurochemicals and (iv) collagen is both disorganized and immature (Coombes, Bissel and Vicenzino, 2009). In line with other types of tendinopathy, standard inflammatory markers are not present, although neurogenic inflammation has been identified (Fredberg and Stengaard-Pedersen, 2008).
In addition to tendon pathology both pain system change and motor impairment have been proposed as important for a multimodal treatment approach (Coombes, Bissel and Vicenzino, 2009). As with many painful conditions tennis elbow is characterized by an exaggerated response to noxious stimuli (hyperalgesia). Testing local pain response using pressure, tennis elbow sufferers have been shown to have a lower pain threshold (66%) on the injured side compared to the uninjured side (Pienimäki et al., 2002). This change in pain threshold is often bilateral implying an alteration in central sensitization. In addition tennis elbow sufferers often have positive cervical joint signs and/or positive radial nerve bias upper limb tension test (ULTT), suggesting that neural involvement is not restricted to the local tissues.
Morphological changes in the muscles affected by tennis elbow include fibre necrosis, increased fast twitch fibre ratio and muscle fibre regeneration (Coombes, Bissel and Vicenzino, 2009), consistent with the finding that grip strength is reduced in tennis elbow patients. In addition motor control changes occur with wrist position changing during standard grip task with less extension being present. Normal grip requires the wrist extensors to stabilize the wrist against the strong pull of the long finger flexors which tend to flex the wrist. In a group of 40 subjects Bisset et al. (2006) showed wrist postures that were less extended (mean value 11°) and upper-limb reaction times which were significantly altered.
Clinical presentation
Tennis elbow usually presents as pain over the region of the lateral epicondyle, extending distally. The pain may build up slowly (overuse) or be the result of a single incident (trauma). Pain is usually increased with resisted wrist extension. Depending on the site of the lesion, pain can be made worse by adding forearm supination (but see radial tunnel syndrome, below), and radial deviation of the wrist (Halle, Franklin and Karalfa, 1986). Performing resisted wrist extension with the elbow fully extended will usually elicit pain, even in mild cases. Resisting the 3rd metacarpal places the emphasis on ECRB rather than ECRL which attaches to the base of the 2nd metacarpal (Maudsley’s test).
Treatment
Acute phase
Treatment aims initially to reduce pain and swelling. The PRICE protocol is used, and several authors have reported good results by using ultrasound, alone or with hydrocortisone gel (Griffen and Touchstone, 1963; Kleinkort and Wood, 1975; Halle, Franklin and Karalfa, 1986). Reducing the stress applied to the tendon is important. Rest from exacerbating activities and the use of counterforce bracing are effective. The counterforce brace consists of a tight strap which is placed around the upper forearm to create a lateral pressure when an object is gripped. The aim is to redirect and disperse overload to healthy tissue or to the band itself, and in so doing reduce painful inhibition and permit a more forceful contraction. Using this technique, grip strength has been shown to improve (Burton, 1985; Wadsworth et al., 1989), and a positive effect has been shown using biomechanical analysis and technique correction of tennis serves and backhand strokes (Groppel and Nirschl, 1986).
The use of nitric oxide given in a transdermal patch as glyceryl trinitrate (GTN) has been described in the treatment of tennis elbow (Paoloni et al., 2003). When compared to placebo patients in the glyceryl trinitrate group had significantly reduced pain with activity, reduced epicondylar tenderness and increased wrist extensor force. A concentration of 1.25 mg/24 hours is traditionally used, cutting a 0.5 mg patch into four and applying this quarter of a patch each day. However, a more recent study (Paoloni et al., 2009) did not support these earlier results, showing a significant decrease in elbow pain with activity using GTN at a concentration of 0.72 mg/day compared to placebo, but not with 1.25 mg/24 hours, 1.44 mg/24 hours or 3.6 mg/24 hours. In addition GTN patches can give complications including headache, weakness, dizziness and skin irritation causing 12% of patients to discontinue treatment as a result of these side effects (Coombes, Bissel and Vicenzino, 2009).
Exercise
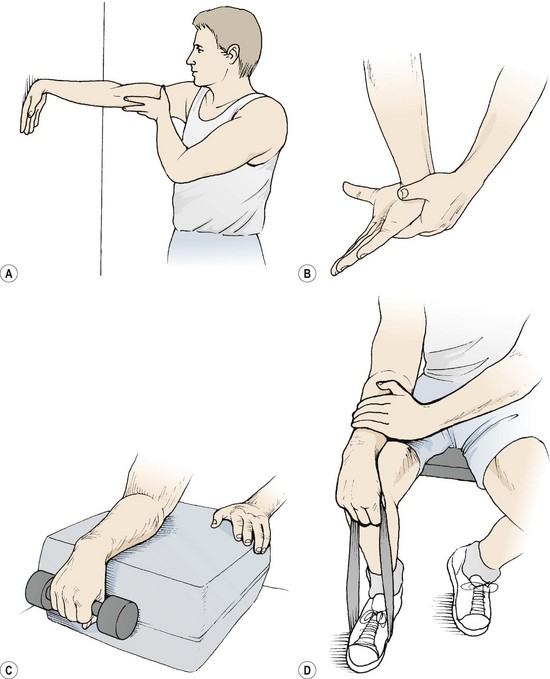
As the local swelling adheres and shrinks, inelastic scar tissue is formed. Stretching exercises are therefore of particular value. A useful forearm extensor stretch may be performed with the athlete facing a wall (Fig. 18.7A). The dorsum of the hand is placed flat onto the wall, and the elbow remains locked. By leaning forwards the wrist is forced into 90° flexion, stretching the posterior forearm tissues. Wrist flexion may be combined with a pronation stretch (Fig. 18.7B). Keeping the elbow locked, the forearm is maximally pronated and the wrist flexed. Overpressure is applied with the other hand and a static stretch performed. The scar tissue is more pliable when warm and so the athlete is advised to practise stretching after a hot bath or shower. Resistance exercises (weight or powerband) are used to re-strengthen the forearm extensors. Wrist extension may be performed holding a small (2 kg) dumb-bell. The forearm is supported on a block or over the couch side and full range movement is attempted (Fig. 18.7C). Initially this is performed with the elbow flexed to reduce pain on the affected muscle (ECRL), and as pain allows the elbow is extended. Powerband extension is performed with the athlete sitting. One end of the band is placed beneath the foot and the other end gripped. The forearm is supported along the athlete’s thigh (Fig. 18.7D). Initially, eccentric contractions are likely to be less painful than concentric, and the use of ice massage to produce a temporary anaesthesia before exercise is applied (cryokinetics) is often used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree