CHAPTER 8 The hip and thigh
The hip joint
Whereas the glenohumeral joint functions mainly in an open kinetic chain position, the hip (coxofemoral) joint functions mainly in a closed chain position. For this reason, its structure is one of stability for weight bearing. In the standing position, however, the joint is not fully congruent, the anterosuperior portion of the cartilage of the head being exposed. It is only when the joint is taken into a position equivalent to that of the quadruped (90° flexion, 5° abduction, and 10° lateral rotation) that maximum articular contact of the head with the acetabulum occurs (Palastanga, Field and Soames, 1994).
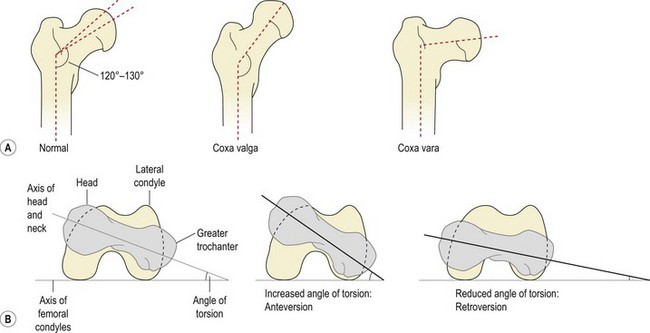
The femoral neck makes an angle (the angle of inclination) with the shaft of 120–130° in the adult, representing the adaptation of the femur to the parallel position of the legs in gait (Fig. 8.1A). This changes from 150° in the newborn to 142° by age 5, 133° by age 15, and 125° in the adult (Reid, 1992; Palastanga, Field and Soames, 1994). Greater angles than these are termed coxa valga, lesser angles as coxa vara.
Similarly, the axis of the femoral head and neck make an angle with the axis of the femoral condyles (Fig. 8.1B). This angle (angle of torsion, or angle of anteversion) is normally 10° in the adult, having reduced from 25° in the infant. Increased anteversion is linked to squinting or kissing patellae and this condition is twice as common in girls as in boys.
Craig’s test may be used to assess the angle of anteversion; it compares the angle of the femoral neck to that of the femoral condyles at the knee. The patient lies prone on a couch with the knee flexed to 90°. The therapist palpates the greater trochanter (posterior aspect), and the femur is medially and laterally rotated until the trochanter is parallel with the horizontal plane. The angle of anteversion is estimated from the angle of the lower leg to the vertical, and angles greater than 15° are considered abnormal (Sahrmann, 2002). Interestingly, this test has been found to be more reliable than radiological assessment (Ruwe et al., 1992).
Weight bearing
In standing, each hip takes roughly 0.3 times bodyweight, increased to 2.4 times body weight when standing on one leg. Weight-bearing forces of up to 4.5 times bodyweight may be taken on the hip in running (Magee, 2002). In order to take weight most effectively, bony trabeculae line up in the direction of imposed stress. Two major systems exist within the femur (Fig. 8.2). The medial trabecular system travels from the medial cortex of the upper femoral shaft to the superior aspect of the head. This system takes vertically aligned forces created by weight bearing, and is aligned with the superior aspect of the acetabulum, the main weight-bearing region. The lateral trabecular system begins from the lateral cortex of the upper femoral shaft, crosses the medial system, and terminates in the cortical bone on the inferior aspect of the head. The lateral system is aligned to take oblique forces created by contraction of the hip abductors during gait.
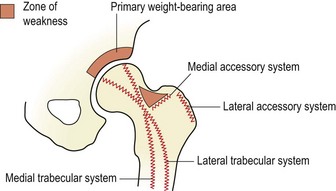
Figure 8.2 Bony trabeculae of the upper femur.
After Norkin, C.C. and Levangie, P.K. (1992) Joint Structure and Function, 2nd edn. FA Davis, Philadelphia. With permission of the publisher FA Davis.
In addition to the medial and lateral trabecular systems, the upper femur is reinforced by medial and lateral accessory systems which take forces created about the trochanters. A zone of weakness is left within the femoral neck which is susceptible to bending forces and is the site of femoral neck fracture (Norkin and Levangie, 1992).
Hip ligaments
The hip joint is strengthened by three capsular ligaments: the iliofemoral ligament and the pubofemoral ligament are on the anterior aspect of the joint, while the ischiofemoral ligament is on the posterior aspect (Fig. 8.3). As the hip is flexed, all three ligaments relax. However, in extension all three ligaments are tight, with the inferior band of the iliofemoral ligament being placed under greatest tension as it runs almost vertically. It is this ligamentous band which limits posterior tilt of the pelvis (Palastanga, Field and Soames, 1994).
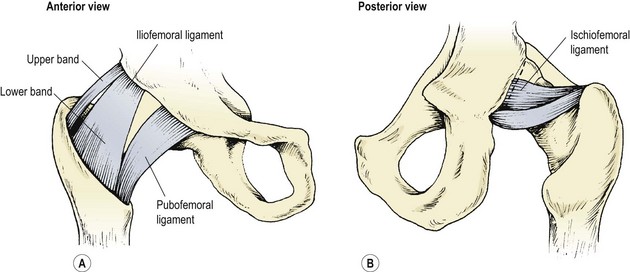
Figure 8.3 Capsular ligaments of the hip joint.
After Palastanga, Field and Soames (1994), with permission.
Screening examination
Compression of the joint through the flexed knee and circumduction with compression to ‘scour’ the femoral head into the acetabulum is an important assessment for arthritic changes. Both the lumbar spine and the sacroiliac joints must be examined, to eliminate them as a potential cause of pain referral. The straight leg raise and slump test should be used to eliminate the possible involvement of neural tissue. Cyriax (1982) warned that serious pathology may be present if the sign of the buttock is positive. Here, hip flexion with the knee bent is more painful and more limited than straight leg raising. A non-capsular limitation is present, and pain may make the end-feel empty. As hip flexion in straight leg raising is full range the sciatic nerve is unimpinged, and the non-capsular limitation precludes the hip joint. Possibilities include an inflammatory disease state, neoplasm and fracture.
Muscle imbalance around the hip
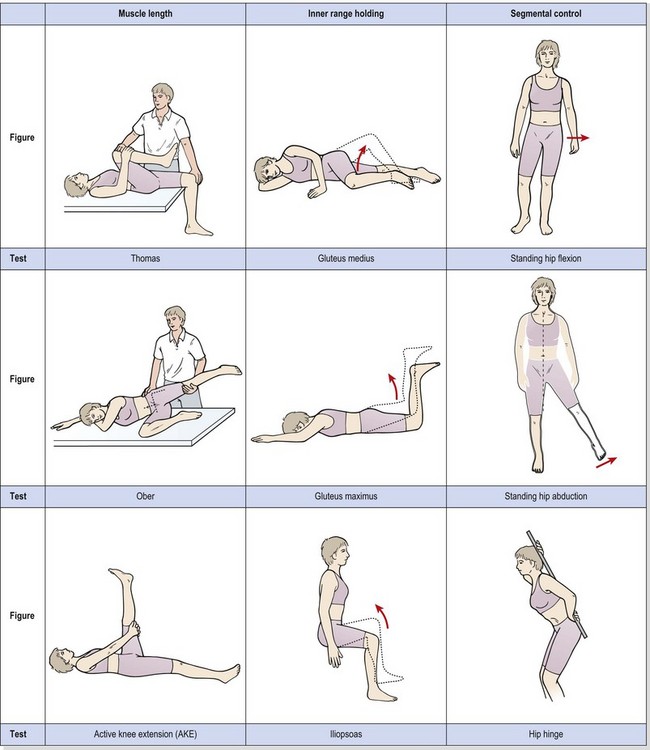
The concept of muscle imbalance was covered in Chapter 5. In the hip region, the Thomas test and the Ober manoeuvre are used to assess for muscle tightness of the hip flexors (rectus femoris and iliopsoas) and hip abductors (tensor fascia lata and iliotibial band – TFL/ITB). Inner range holding ability of the gluteus medius is assessed with side-lying hip abduction and of the gluteus maximus with the prone-lying hip extension movement described below. Segmental control tests include standing hip flexion, standing hip abduction and the hip hinge (Table 8.1). All tests are described in Chapter 5.
Table 8.1 Muscle imbalance around the hip
Muscle injuries
Quadriceps
Initially, there is local swelling over the front of the thigh, with some superficial bruising appearing later, often tracking down to the knee. The main danger with this injury is the development of myositis ossificans traumatica (MOT). Thigh contusions may be rated as grade 1 (mild), in which knee flexion beyond 90° is possible, grade 2 (moderate), in which motion is restricted to 45–90°, or grade 3 (severe), in which swelling and pain limit movement to less than 45°. This grading system can be an accurate predictor of the likelihood of MOT development. Jackson and Feagin (1973) assessed quadriceps contusions in 65 subjects, and found that none of the subjects with grade 1 injuries had developed MOT. However, 13 out of 18 subjects who had been graded 2 or 3 later went on to develop the condition, so the amount of movement present in the initial stages is an important indicator of the severity of the lesion, and the prognosis.
It is important to limit movement in grade 1 and 2 injuries and to discourage the use of massage, vigorous stretching or exercise and ultrasound, as these are contraindicated in the early post-injury stage. The RICE protocol is used to limit the tissue damage. Ice is applied with compression with the knee and hip flexed as far as is comfortable. Internal compression is therefore applied by fascial tightening (Reid, 1992), while external compression comes from the elastic bandage.
In cases of MOT, calcification is slow, with fibroblasts beginning to differentiate into osteoblasts about 1 week after injury. Radiographic evidence of bone formation is usually visible after 3 weeks (Fig. 8.4). By 6–7 weeks after injury, the calcified mass generally stops growing. Total reabsorption may occur with minor lesions, but more major conditions may continue to show remnants of the mass. The mass rarely interferes with muscle contraction, so excision is not normally required (Estwanik and McAlister, 1990).
Rectus femoris
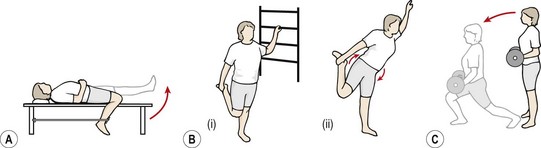
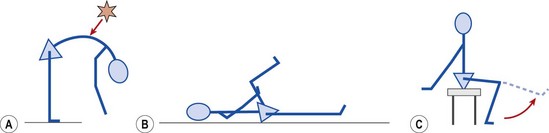
The rectus femoris can be worked concentrically by flexing the hip against a resistance supplied by a weight bag attached to the knee. Two-joint action of the muscle can be worked with the athlete in supine with the injured leg over the couch side, flexed at both the knee and hip. Manual resistance is applied to the foot of the athlete as he or she extends the knee and flexes the hip simultaneously (Fig. 8.5A).
Stretching must involve both knee flexion and hip extension and can be carried out in a side-lying position by the athlete, or by the therapist. When performing a rectus femoris stretch in standing (Fig. 8.5B), the abdominal muscles must be tightened to stabilize the pelvis before the hip stretch is applied. Failure to do so will increase the apparent range of motion by anterior tilt of the pelvis with stress thrown on the lumbar spine. Lunging actions are also useful, for both general flexibility and eccentric control (Fig. 8.5C).
Results are generally very good, even with complete tears (Fig. 8.6), where full function may be regained even though a marked muscle deformity is present.
Sartorius
Injury to the sartorius is usually an avulsion from the anterior superior iliac spine. There is usually immediate pain, often radiating into the anterior thigh. Swelling and bruising is seen over the iliac crest, often tracking down the thigh. Flexion/adduction of the hip with flexion of the knee causes pain. Displacement of the bone fragment may be from a few mm to 3 cm, but although surgical reattachment of the bone fragment has been described (Veselko and Smrkolj, 1994), conservative treatment normally suffices. The athlete should be non-weight bearing initially, followed by partial weight bearing ambulation for 3–6 weeks, depending on the intensity of pain. Full strength and flexibility must be regained before competitive sport is resumed.
The hamstrings
To palpation, the structure of the muscles differentiates them. The semitendinosus and long head of biceps have a combined attachment on the lower medial facet of the ischial tuberosity, the two muscles travelling together for a short distance until they form fusiform muscle bellies. The semitendinosus almost instantly forms into a long slender tendon, and travels around the medial condyle of the tibia to attach to the medial surface of the tibia below gracilis. The biceps has two proximal attachments; the long head, as described, and the short head from the lower linea aspera. The muscle swings downwards and laterally across the posterior aspect of the thigh and around the lateral ligament to insert into the head of the fibula. The biceps has a dual innervation, and asynchronous stimulation of the two heads has been described as a factor in injury (Burkett, 1975). The semimembranosus comes from the lateral facet of the ischial tuberosity and travels down and medially, becoming flattened and broader as it does so. The semimembranosus is deep to both the semitendinosus and biceps, and divides into five components when it reaches the knee. The principal insertion is to the posterior aspect of the medial tibial tubercle.
Biomechanics and hamstring injury
During the running cycle, the hamstrings contract eccentrically to decelerate the leg in late forward swing. This action also helps to stabilize the knee. During the support phase, the hamstrings act concentrically to extend the hip, and continue to stabilize the knee by preventing knee extension. During push-off, the hamstrings and gastrocnemius, both two-joint muscles, paradoxically extend the knee. This action is necessary because the mechanical efficiency of the quadriceps is reducing at this point (Sutton, 1984).
The ratio of the strength of the hamstrings to that of the quadriceps muscles (HQ ratio) is important. Normally, the quadriceps is the stronger of the two muscle groups (Table 8.2), as demonstrated by its greater volume. However, any disturbance to this natural balance may leave the weaker muscle group open to injury. The optimum value of the HQ ratio varies from 50% to 80% (Kannus, 1989), with average values in the region of 60%. After knee injury, quadriceps wasting may result in the two muscle groups producing the same power, giving an HQ ratio of 100% (Burnie and Brodie, 1986a).
Table 8.2 Percentage of strength relative to quadriceps at 100%
| Hamstrings | 50–60% |
| Adductors | 90% |
| Abductors | 60% |
| Hip flexors | 55% |
From Reid (1992).
Strength measures comparing quadriceps to hamstrings are traditionally carried out with an isometric dynamometer. However, the disadvantages of joint specificity and lack of movement make isokinetic testing more desirable. During isokinetic testing the speed of movement should match the speed of the sport as closely as possible. The speed must be quoted, as the absolute value of the HQ ratio increases as velocity of movement increases (Burnie and Brodie, 1986b). Slow speeds (45°/s) have been shown to give ratios of 60% and high speeds (300°/s) ratios of 80% (Sutton, 1984). Isokinetic testing in the standard sitting position does not allow hip motion, and movement of the limb does not occur in a closed kinetic chain, so testing is not ideal.
Aetiology of hamstring injury
Tears tend to occur when there is a breakdown in the reciprocal action of the quadriceps and hamstrings, and happen at one of two instances in the running cycle. First, during late forward swing as the hamstrings are decelerating the limb and the athlete feels the muscle ‘stretch’, and secondly, during the take off phase as the athlete ‘pushes’. Changes in muscle coordination as a result of an alteration in the sensitivity of muscle spindles have been cited as a contributory factor to injury. It has been suggested (Sutton, 1984) that an athlete who is fatigued unconsciously increases the sensitivity of the muscle spindles, which respond to stretch with an exaggerated contraction, and this in turn causes injury.
Lack of flexibility may predispose to hamstring injury, and may be assessed with the athlete lying supine with one hip flexed to 90°. Maintaining this position by gripping the leg with the hands, the athlete attempts to straighten the leg with quadriceps power only (AKE test). Adequate flexibility is indicated by an ability to lock the leg out while maintaining 90° hip flexion. Alterations in the normal 60% strength ratio between the quadriceps and hamstrings and a deficit greater than 10% between the two sets of hamstrings has also been cited as a predisposing factor (Burkett, 1970).
Many hamstring injuries tend to recur, and lack of full rehabilitation may be one cause. After injury, athletes are usually aware of lack of mobility in the hamstrings and are often conscientious about stretching exercises. However, muscle wasting is not so obvious in the hamstrings as it is in the quadriceps, and so many athletes forget to spend time regaining hamstring strength. In addition, using eccentric exercises as part of a general leg conditioning programme may strengthen the series of elastic components within the hamstrings (the non-contractile portion of the muscle, including the muscle tendon and the connective tissue framework of the muscle itself), making them better equipped to withstand loading at heel strike (Stanton and Purdam, 1989). The inclusion of plyometric training in late stage rehabilitation of hamstring injury is therefore essential.
A systematic review of the causation of hamstring injuries in sport (Foreman et al., 2006) was not able to reveal a single factor to be consistently associated with hamstring injury due to the wide variety of research methodologies used in studies. However six common themes were identified (Table 8.3).
Table 8.3 Factors associated with hamstring injury causation
| Factor | Implication |
|---|---|
| Muscle strength & imbalance | Reduced hamstring strength may not be able to counteract quadriceps force during knee extension in swing phase |
| Muscle control | Poor neuromuscular control may affect interaction of thigh muscles |
| Flexibility | Reflects on ability of muscle to absorb shock |
| Previous injury | Rehabilitation may have been inadequate or risk factors still present |
| Anthropometry | Age, race, number of type II fibres and anterior pelvic tilt all implicated |
| Muscle fatigue | Injuries more common while athletes fatigued, running gait change suggested |
From Foreman et al. (2006).
Exercise therapy following hamstring injury
Strength
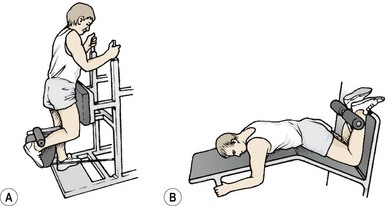
Where isokinetics are available, a variation of speeds is important. Slow speeds of 60° and 120°/s may be used to begin with, progressing to 240° and 300°/s as pain allows. Hamstring isolation exercises, such as leg curls in lying and standing (Fig. 8.7), have their place in initial rehabilitation to ensure maximal muscle broadening, but have distinct limitations which must be recognized. First, these exercises work only the knee flexion function of the hamstrings, with little activity over the hip. Second, the action is open chain only, when the predominant function of the hamstrings occurs in closed chain format. Third, the exercises are often performed with the emphasis placed on inner-range contraction, which may tend to shorten the muscle. The hamstrings are unlikely to be posturally lengthened so that they require shortening. It is more likely that the muscles will already lack flexibility, so full range resisted work is preferable.
Eccentric training
Eccentric training of the hamstrings is an important component of rehabilitation. At the end of the swing phase of gait, the hamstrings decelerate the limb by eccentric action, and so preparing the athlete for this action is essential. Eccentric training has been shown to favourably affect the length−tension curve of the hamstrings measured on an isokinetic dynamometer (Clark et al., 2005). Subjects showed a 19.4% change in the position of peak force creation towards the extended knee which may protect against eccentric overload at the end of the swing phase. Eccentric hamstring training of this type has been shown to reduce the incidence of injury in elite soccer (Arnason et al., 2008), and to successfully rehabilitate Australian rules football players (Brughelli, Nosaka and Cronin, 2009). Eccentric exercises include box drops, negative lunges and eccentric leg extension from high kneeling (Nordic hamstring exercise) (Fig. 8.8).
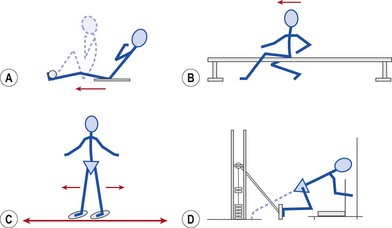
Closed chain actions
Closed chain exercises may be performed by modifying many common exercises. Leg rowing (Fig. 8.9A) is a useful exercise. The athlete sits on a towel (on a wooden floor) or plastic tray (on a carpeted floor) with the feet fixed. The action is to pull the body forwards by hamstring action, mimicking a rowing position. Sitting astride a gym bench or ‘form’ (Fig. 8.9B), the athlete digs the heels into the ground and again pulls the body forwards using leg strength alone. Both of these actions may be performed unilaterally or bilaterally. The slide trainer may also be used for sagittal leg pumping actions with the knees straight or bent (Fig. 8.9C). The sitting leg press weight training apparatus may be used for the sprint kick exercise (Fig. 8.9D). Instead of sitting on the bench, the athlete turns around and places the shoulder against the chair back, and the ball of the foot on the machine pedal. The action is to press the machine pedal with a combined hip and knee extension action.
Speed, power and flexibility
Flexibility exercises for the hamstrings must take account of pelvic action and the action of the two-joint muscle. In addition, relative flexibility may dictate that the majority of the stretching force is imposed on the lumbar spine in toe-touching type movements (Fig. 8.10A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree