51 Temporomandibular Joint Pain
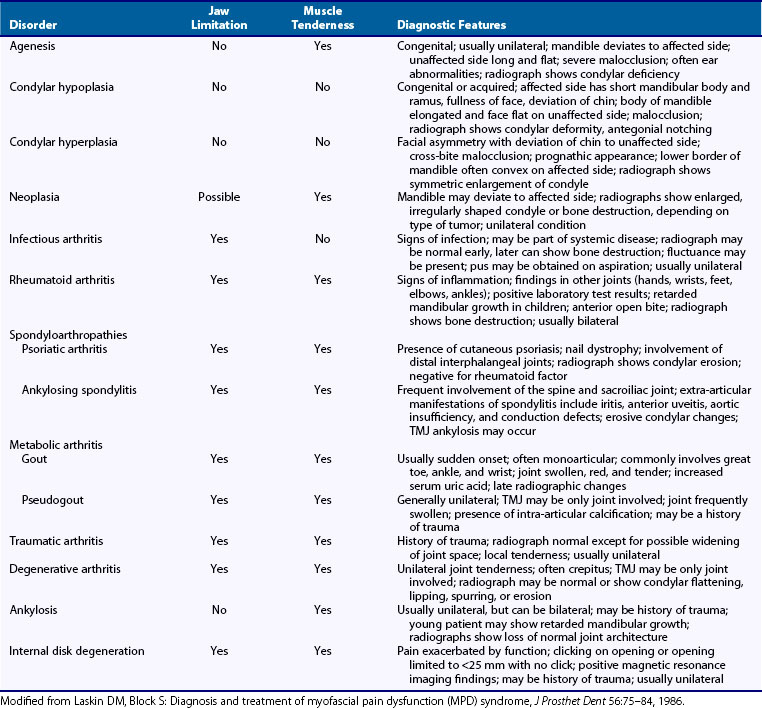
Because patients with primary TMJ disease often have secondary myofascial pain in the muscles of mastication, and because patients with primary myofascial pain problems in the masticatory muscles can develop secondary TMJ disease, the generally accepted term used to describe this overlapping group of conditions is temporomandibular disorders. These conditions are subdivided for purposes of diagnosis and treatment into conditions that primarily involve the TMJ (TMJ problems) and conditions that primarily involve the muscles of mastication (myofascial pain and dysfunction [MPD], masticatory myalgia). From a diagnostic standpoint, it is important to consider the numerous conditions that mimic the temporomandibular disorders or MPD by producing similar signs and symptoms (Tables 51-1 and 51-2).
Table 51-1 Differential Diagnosis of Nonarticular Conditions Mimicking Temporomandibular Joint Pain or Myofascial Pain in the Masticatory Muscles
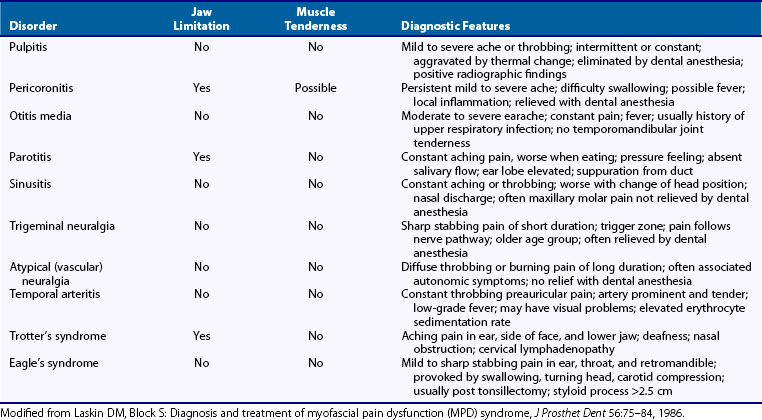
Table 51-2 Differential Diagnosis of Nonarticular Conditions Producing Limitation of Mandibular Movement
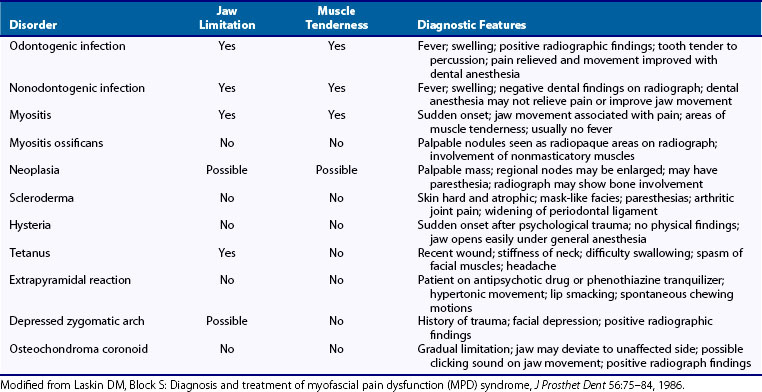
Table 51-3 lists the various pathologic entities that commonly involve the TMJ. Although a variety of conditions are known, only three types are considered to generally produce pain: the various arthritides, derangements of the intra-articular disk, and certain neoplasms.
Arthritis of the Temporomandibular Joint
Osteoarthritis
Osteoarthritis is the most common type of arthritis involving the TMJ and the most frequent cause of pain in that region. Clinical symptoms of the disease have been reported in 16% of the general population,1 but radiographic features have been found in 44% of asymptomatic individuals.2 Although the TMJ is not a weight-bearing joint in the same sense as the joints of the long bones, the stresses associated with such parafunctional habits as clenching and grinding of the teeth are sufficient to contribute to similar degenerative changes in some patients.3 Acute and chronic trauma and derangements of the intra-articular disk also are common causes of secondary degenerative arthritis.
Treatment
Treatment of degenerative arthritis of the TMJ is usually medical, as in other joints of the body. It involves the use of nonsteroidal anti-inflammatory drugs, application of heat, eating a soft diet, limitation of jaw function, and use of a bite appliance to control parafunction if the patient has a chronic habit of clenching or grinding the teeth. Arthrocentesis has also been shown to be helpful.4,5 Physical therapy with thermal agents, ultrasound, and iontophoresis also can be beneficial, and isotonic and isometric exercises are used to improve joint stability after acute symptoms have subsided. The use of intra-articular steroid injections is controversial; they should be used only in patients with acute symptoms that do not respond to other forms of medical management. Because of the potentially damaging effects of long-acting steroids,4,6 they should be limited to no more than three or four single injections given at 3-month intervals. Intra-articular injection of high-molecular-weight sodium hyaluronate given twice, 2 weeks apart, has been shown to have essentially the same therapeutic effect as a steroid injection, without the potential adverse effects.5,7
When the acute symptoms have been controlled, therapy is directed toward control of factors possibly contributing to the degenerative process. Unfavorable loading of the joint is eliminated by replacement of missing teeth to establish a good, functional occlusion; by correction of any severe dental malrelationships through orthodontics or orthognathic surgery; and by continued use of a bite appliance at night to control teeth-clenching or teeth-grinding habits.6,8
Rheumatoid Arthritis
More than 50% of patients with rheumatoid arthritis have involvement of the TMJ.9 Although the TMJ may be affected early in the course of the disease, other joints in the body usually are involved first. The general female-to-male ratio is 3 : 1. TMJ involvement may also characterize juvenile inflammatory arthritis. In children, destruction of the mandibular condyle by the disease process results in growth retardation and facial deformity characterized by a severely retruded chin. Fibrous or bony ankylosis is a possible sequel at all ages.
Diagnosis
Rheumatoid arthritis is diagnosed on the basis of the history, clinical and radiographic findings, and confirmatory laboratory tests. Distinguishing features for rheumatoid arthritis and degenerative arthritis of the TMJ are shown in Table 51-3.
Treatment
Treatment of rheumatoid arthritis of the TMJ is similar to that provided for other joints.7,10 Anti-inflammatory drugs are used during the acute phases, and mild jaw exercises are used to prevent excessive loss of motion when acute symptoms subside. In severe cases, disease-modifying drugs, such as methotrexate, and biologic agents, including etanercept, infliximab, adalimumab, certolizumab, golimumab, abatacept, tocilizumab, and rituximab, may be used pending systemic presentation. Orthognathic surgery may be necessary in patients with an anterior open bite after the disease goes into remission, or in patients in whom ankylosis develops after that condition is corrected.
Spondyloarthropathies
In addition to the adult and juvenile forms of rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and reactive arthritis also can involve the TMJ.8–13
Psoriatic Arthritis
Psoriatic arthritis occurs in approximately one-third of patients who have cutaneous psoriasis. It can have a sudden onset, can be episodic in nature, and may show spontaneous remission.9,12 Often only one TMJ is involved. Symptoms include TMJ pain and tenderness, restricted jaw movement, and crepitation, mimicking the symptoms of rheumatoid arthritis.9,12 Radiographic changes are nonspecific and cannot be distinguished easily from those of other types of arthritis, particularly rheumatoid arthritis and ankylosing spondylitis.13,14 They usually involve erosive changes in the condyle and glenoid fossa associated with extreme narrowing of the joint space.11,15,16 In severe cases, ankylosis may develop, reflected occasionally in new bone formation at earlier stages.12,17
Treatment of psoriatic arthritis of the TMJ is similar to that of rheumatoid arthritis, and is driven essentially by the imperative to treat the systemic inflammatory disease process.13,18–21 Surgery is necessary if ankylosis occurs.
Ankylosing Spondylitis
About one-third of patients with ankylosing spondylitis develop TMJ involvement several years after onset of the disease. Pain and limitation of jaw movement are the most common symptoms, and ankylosis can develop in advanced cases.8,11,14,22 On radiographic examination, about 30% of patients show erosive changes in the condyle and fossa and narrowing of the joint space.15,23 In long-standing cases, a more florid osteophytic response is sometimes seen during quiescent periods. The severity of the changes seems to be related to the severity of the disease. Treatment of ankylosing spondylitis of the TMJ is generally medical and is part of the total management of the patient. Physical therapy is used to improve jaw mobility, and bite appliances are used, when indicated, to reduce parafunctional stress on the joint. If ankylosis develops, surgery is the treatment of choice.24
Reactive Arthritis
Reactive arthritis of the temporomandibular joint is more common in males than in females. It is characterized by recurrent pain, swelling, and limitation of mouth opening.25 Radiographically, condylar erosion may be evident.26 Treatment is similar to that of the other seronegative spondyloarthropathies, consisting of nonsteroidal anti-inflammatory drugs, intra-articular steroids, and disease-modifying drugs. If a specific triggering bacterial infection can be identified, an appropriate antibiotic should be prescribed.
Traumatic Arthritis
Acute trauma to the mandible that does not result in a fracture can still produce injury to the TMJ. When this occurs in a child, it is essential to warn the parents about the possibility of future retardation of mandibular growth and associated facial deformity resulting from damage to the articular cartilage, which is an important growth site.16,27
Infectious Arthritis
Infectious arthritis rarely involves the TMJ. Although it can affect the joint as part of such systemic diseases as gonorrhea, syphilis, tuberculosis, and Lyme disease,17,18,28,29 the most common way is by direct extension of an adjacent infection of dental, parotid gland, or otic origin.19,30 Occasionally, it also may occur from localization of blood-borne organisms in the joint after a traumatic injury or by direct involvement through a penetrating wound.20,30 The most common pathogens are Staphylococcus aureus, Haemophilus influenzae, and Streptococcus species.31
Clinical Findings
Infectious arthritis generally results in unilateral pain, tenderness, swelling, and redness in the region of the TMJ. Chills, fever, sweating, and systemic findings characteristic of the specific type of infection also are present. Often the teeth cannot be occluded because of swelling within the joint. In pyogenic forms of infectious arthritis, fluctuation may be noted in the joint region. Patients with Lyme disease show characteristic skin lesions and often positive serology.18,29
Treatment
Treatment of infectious arthritis includes the use of appropriate antibiotics, proper hydration, control of pain, and limitation of jaw movement. Arthrocentesis with Ringer’s solution one to three times weekly until acute symptoms subside has also been recommended.32 Suppurative infections may require aspiration, incision, and drainage, or sequestrectomy. When bone loss has been extensive, reconstructive procedures may be necessary. In children in whom mandibular growth has been affected, a costochondral graft can be used to correct facial asymmetry and re-establish growth of the mandible.
Metabolic Arthritis
Metabolic arthritis, which can accompany gout or pseudogout (calcium pyrophosphate dehydrate arthropathy), is rare in the TMJ.21,33
Gout
When attacks are infrequent, radiographic changes may not be noted for a long time. Because so few cases have been reported, the precise radiographic changes that occur have not been well documented. Calcified areas in the disk, destruction of the hard tissues of the joint, condylar exostoses and spurring, and the presence of tophi have been described.21,33–35 The initial approach to treatment of gout involving the TMJ is medical. If symptoms are not controlled, however, surgical débridement of the joint and arthroplasty may be indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree