Fig. 15.1
Bigliani classification of acromial shape: type I (flat), type II (curved), and type III (hooked) (Figure adapted from Kevin D. Plancher, MD)
The subacromial bursa lies between the undersurface of the acromion and the superior surface of the rotator cuff. The subacromial bursa does not have a sturdy ligamentous capsule, and the fascicle attachments are often quite thin. This anatomy can lead to fluid extravasation into the muscle and subcutaneous envelope of the shoulder. Surgical time should be limited and the fluid pump pressure and flow should be kept to a minimum when operating in this area.
Coracoid impingement, while less common, occurs between the anteromedial portion of the coracoid process and the lesser tuberosity of the humerus [6]. The coracoacromial ligament extends from the coracoid process to the anterior aspect of the acromion; thickening of the coracoacromial ligament can also reduce the size of this space.
15.4 Biomechanics
Functional range of motion of the shoulder can alter the dimensions of the subacromial space and contribute to clinical signs of impingement syndrome, specifically, shoulder abduction and rotation [7, 8]. As the shoulder moves from 30° to 120° of abduction, the distance between the humerus and the acromion significantly decreases by almost 50 % [8]. The minimum distance between the acromion and the humerus is also smallest with arm in external rotation at 90° [8]. Grachien and colleagues reported that when the arm is in 90° of abduction and 45° of internal rotation, the supraspinatus is closest to the anteroinferior border of the acromion [8]. Furthermore, while arm elevation leads to a decrease in subacromial space width, adduction muscle forces substantially increase the acromiohumeral distance and claviculohumeral distance compared to abduction muscle forces (138 % at 90° relative to abduction forces). The biomechanics support strengthening of the adductor muscles, including the latissimus dorsi, subscapularis, and teres major and minor, in both conservative and postoperative rehabilitation programs to avoid and lessen the symptoms of impingement syndrome [9].
Pressure in the subacromial bursa also changes with arm position as well as with changes in the demand of the activity. Sigholm et al. monitored pressure in the subacromial bursa using a microcapillary infusion technique with the arm at rest by the side, with the arm abducted to 45°, and with the arm abducted to 45° holding a 1 kg weight [10]. Subacromial bursal pressure increased fourfold from 8 to 32 mmHg when changing the arm from 0° to 45° of abduction and increased sixfold when holding a 1 kg weight.
Scapular dyskinesis or dynamic scapular winging, seen on evaluation of the scapula during overhead range of motion, may contribute to clinical signs of impingement as a result of abnormal scapular muscle activity and subsequent abnormal scapular kinematics. Patients with impingement demonstrate decreased output force, muscle balance, electromyographical activity, and activation latency of the trapezius and serratus anterior muscles which stabilize the scapula and control scapular rotation. A study by Silva et al. [11] revealed that the subacromial space is smaller in patients with scapular dyskinesia than in control patients, and that the subacromial space undergoes greater reduction when the shoulder is moved from neutral abduction to 60° of elevation in patients with scapular dyskinesia than in control patients. Additionally, weakness of the rotator cuff can lead to abnormal glenohumeral and scapulothoracic kinematics and subsequent narrowing of the subacromial space [3].
15.5 Variations
There are several anatomic variants that can influence the development of subacromial impingement. The acromion has three cartilaginous growth centers that ossify during development. In up to 15 % of people, one or more of these growth centers do not ossify [12]. A persistent growth center in the acromion is referred to as the os acromiale. The presence of an os acromiale may increase the risk of subacromial impingement syndrome as failure of this growth plate to close allows for some motion of the acromion which may impinge on the rotator cuff tendons or bursa. Additionally, variations in the coracoacromial ligament, the direction of the slope or angle of the acromion, the inferior aspect of the acromioclavicular joint, and the shape of the acromion all contribute to narrowing of the subacromial space and outlet of the rotator cuff tendons [3].
15.6 Physical Examination: Special Tests
Several key maneuvers are essential to include in physical examination to aid in the diagnosis of subacromial impingement syndrome. The likelihood of a diagnosis of impingement is >95 % when a specific battery of tests are positive, including the Hawkins-Kennedy impingement test, painful arc, and infraspinatus test [13]. When this battery of tests is negative, the likelihood of impingement is <24 %.
The Neer impingement sign causes provocation of pain at the anterolateral edge of the acromion when the examiner passively forward flexes the arm greater than 120° with the humerus internally rotated and the scapula stabilized (Fig. 15.2). The Neer sign has a sensitivity and specificity of 68.0 and 68.7 %, respectively [13]. Hawkins and Kennedy also described an alternative impingement test which elicits symptoms when the arm is placed in 90° forward elevation and then gently internally rotated (Fig. 15.3). The Hawkins-Kennedy sign has a sensitivity and specificity of 71.5 and 66.3 %, respectively [13]. These impingement tests place the greater tuberosity, rotator cuff, or biceps tendon against the undersurface of the acromion or coracoacromial ligament causing aggravation of an inflamed bursa.
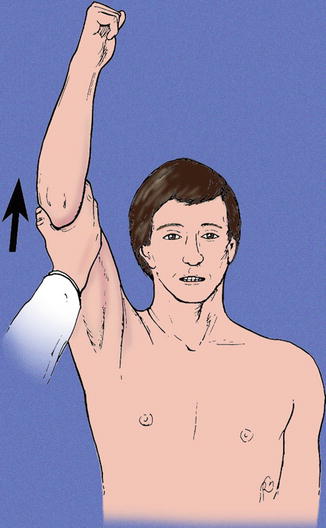
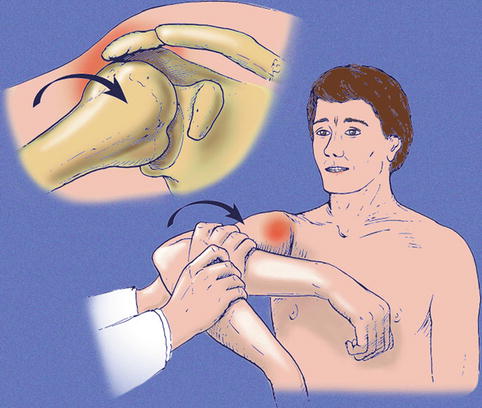
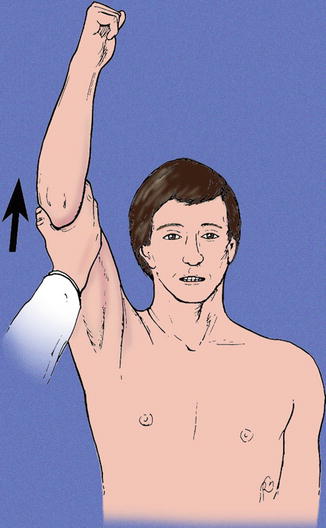
Fig. 15.2
Neer impingement sign. The examiner stabilizes the scapula and passively flexes the arm greater than 120° with the arm internally rotated. Provocation of pain at the anterolateral edge of the acromion is indicative of subacromial impingement (Copyright Kevin D. Plancher)
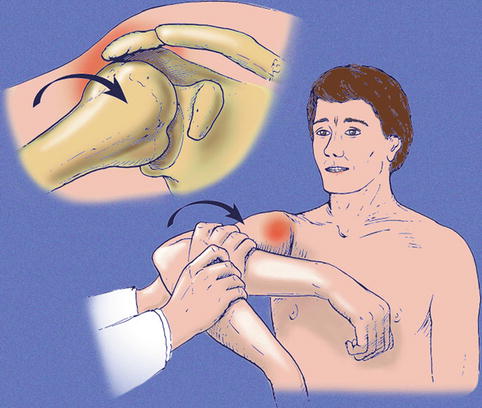
Fig. 15.3
Hawkins-Kennedy impingement sign. The patient’s arm is positioned in 90° of forward elevation with the elbow flexed to 90°. The examiner then gently internally rotates the arm. Provocation of pain at the anterolateral edge of the acromion is indicative of subacromial impingement (Copyright Kevin D. Plancher)
A painful arc of motion between 60° and 120° of active forward elevation in the plane of the scapula is indicative of impingement. The patient often reports pain or painful catching in the shoulder. This test has a sensitivity of 73.5 % and specificity of 81.1 % [13]. Lastly, the infraspinatus muscle test performed with the arm at the side and the elbow flexed to 90° elicits pain when the patient resists against an internal rotation force.
Many disorders of the shoulder present similar to subacromial impingement syndrome. A diagnostic lidocaine anesthetic injection into the subacromial space can improve the accuracy of the diagnosis of subacromial impingement syndrome. We instill 10 mL of 1 % lidocaine using a 25-gauge, 1½-inch needle into the subacromial space through an anterior approach. Ultrasound can be used as an adjunct to guide the needle to ensure accuracy. Alternatively, the needle can be placed 1 cm inferior to the posterolateral corner of the acromion directed toward the coracoid. Provocative maneuvers should be performed following the injection to confirm the diagnosis. Alleviation of symptoms on impingement tests is highly indicative of subacromial impingement syndrome. The authors believe that a 1½-inch needle is essential if using a posterior approach to avoid a false negative result.
15.7 Diagnostic Imaging
The specificity of special tests on physical examination is low; therefore, imaging of the shoulder should also be utilized in the diagnostic process in order to make an accurate and complete assessment of the underlying pathology [11]. Radiographs can aid in evaluating the concavity of the undersurface of the acromion, assessing for the presence of subacromial spurs, and for the presence of degenerative changes at the greater tuberosity, the acromioclavicular joint, or anterior acromion. A supraspinatus outlet view radiograph is best to evaluate acromial shape. The scapular outlet view, on the other hand, best evaluates the anteroinferior acromion (Fig. 15.4). This view is a true scapulolateral with the x-ray tube angled 5–10° caudally. An AP view of the shoulder with the x-ray tube angled 30° caudally can also be used to evaluate the anteroinferior acromion as well as for the presence of a calcified coracoacromial ligament (Fig. 15.5). This AP caudal tilt view has been shown to have the highest interobserver reliability [14].


Fig. 15.4
Scapular outlet view demonstrating a type III, hooked, acromion. The scapular outlet view best evaluates acromial morphology (Copyright Kevin D. Plancher)
Fig. 15.5
(a) Artwork demonstrating the difference and correct way to obtain a true versus routine AP view of the shoulder (Figure adapted from Kevin D. Plancher, MD). (b) Routine AP shoulder. (c) True AP (Grashey) shoulder
This radiographic series is extremely useful in surgical planning to determine the amount of undersurface of the acromion to be surgically resected to establish a flat acromion. A study by Kitay et al. demonstrated that the distance from the acromial cortex to the end of the acromial spur on x-ray significantly correlated with intraoperative spur length [14]. Acromial slope measured on the supraspinatus outlet view, which was shown to have less intraobserver reliability than the caudal tilt view, significantly correlated with intraoperative acromial thickness. Therefore, the authors believe these views should be included in routine radiographic evaluation and surgical planning when presented with suspected subacromial impingement or rotator cuff involvement prior to acromioplasty.
Magnetic resonance imaging (MRI) can also be useful to evaluate the bony pathology associated with rotator cuff pathology and assess the subacromial-subdeltoid bursa. Evaluation of subacromial spurs as well as for the presence of a type III or hooked acromion is best visualized on the coronal or sagittal oblique cuts (Fig. 15.6). Small spurs appear black (hypointensity) on T2-weighted images, whereas larger spurs appear as high signal on both T1-weighted and T2-weighted images because they contain marrow. Degenerative changes of the acromioclavicular joint can also be visualized on MRI, indicated by hypertrophy of the joint capsule as a medium signal intensity surrounding the acromioclavicular joint on pulse sequences with short repetition time (TR) and short echo time (TE). Changes in the subacromial-subdeltoid bursa and peribursal fat are signs of a rotator cuff tear as a complete tear allows extension of intra-articular fluid in the bursa. This is represented as high signal intensity or white within the bursa on T2-weighted images. The use of ultrasound, computed tomography (CT), and MRI have been shown to be reliable methods for measuring acromiohumeral distance [15]. Normal acromiohumeral distance is approximately 10.5–11 mm and is smaller in females compared to males [16, 17]. The distance is also dependent on arm position and has been shown to be smallest (8.1–9.9 mm) when the arm is flexed to 90° and in neutral rotation and is largest (11.2–12.2 mm) in positions of internal rotation [17]. Additionally, an acromiohumeral distance less than 7 mm has been correlated with a complete rotator cuff tear [18–20].
Fig. 15.6
MRI evaluation of acromial morphology. (a) Type I, flat. (b) Type II, curved. (c) Type III, hooked (Copyright Kevin D. Plancher)
15.8 Sports Significance of the Anatomy
Overhead and throwing athletes often experience a loss of internal rotation range of motion in the dominant arm, ultimately affecting the biomechanics of the shoulder girdle. This loss of internal rotation has been correlated with loss of subacromial space, which may contribute to subacromial impingement syndrome in these overhead athletes known as internal impingement [21]. The cause may be related to either bony adaptations or inflammation in the shoulder or the result of instability, muscle imbalances, or abnormal scapulohumeral mechanics. This has been demonstrated in junior elite tennis players by Silva and colleagues [11]. They found that scapular dyskinesia was more prevalent among tennis players compared to a control group. Tennis players with dyskinesia had a significantly larger reduction in the subacromial space when moving the arm from 0° to 60° of abduction, a common arc of motion in tennis. Similar subacromial space changes have also been documented in basketball players [22]. Changes in subacromial space may predispose athletes to subacromial impingement syndrome and subsequent pathologies.
15.9 Surgical Significance of the Anatomy
Arthroscopic subacromial decompression is a safe and efficacious procedure to treat subacromial impingement syndrome. Resection of the anteroinferior acromion, subacromial bursa, and release of the coracoacromial ligament all lead to an increase in volume of the subacromial space. The anatomy of the subacromial bursa can make it difficult for the surgeon to navigate because of the lack of easily identifiable landmarks. Furthermore, its weak ligamentous capsule can lead to fluid extravasation into the muscle and subcutaneous envelope of the shoulder. Therefore, surgical time should be limited and the fluid pump pressure and flow should be kept to a minimum.
For optimal visualization of the subacromial bursa, the arm should be positioned in 20° of abduction and 5° of forward elevation. Less than 15 lb (6.8 kg) of traction are needed to move the greater tuberosity inferiorly and laterally out of the way to open the subacromial space. To perform a diagnostic burscoscopy, the arthroscopic cannula should be placed into the posterior portal aiming for the posterolateral border of the acromion and advanced to the posterior acromial edge. The 30° arthroscope is inserted into the subacromial space and directed to the tip of the cannula. A radiofrequency device can be used to ablate and debride the bursal adhesions and the posterior bursal curtain (posterior “veil of tears”). Visualization can be hindered throughout the procedure without debridement of this posterior bursal curtain. A medial to lateral “sweep” is performed from the medial border of the acromion to the level of the lateral portal to break up any bursal adhesions and create a “room with a view”.
In order to delineate the subacromial space and widen it, the anterior and lateral borders of the acromion should be defined and the undersurface of the acromion should be debrided using a radiofrequency device. The remaining bursa can then be debrided using a full-radius motorized shaver (Fig. 15.7). It is the preference of the senior author to debride the entire bursa until the blood vessels overlying the superior rotator cuff can be clearly seen (Fig. 15.8). Use of the motorized shaver medial to the supraspinatus myotendinous junction should be avoided due to bleeding. When releasing the coracoacromial ligament, bleeding from the acromial branch of the thoracoacromial artery should be ablated with a radiofrequency device. The coracoacromial ligament should be performed at the most lateral aspect to avoid this vessel.
Fig. 15.7
Arthroscopic view using an arthroscopic shaver to completely debride the subacromial bursa (Copyright Kevin D. Plancher)