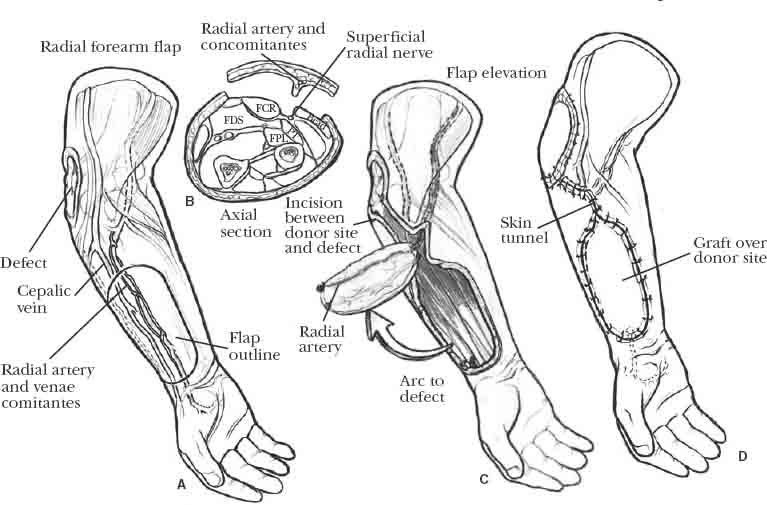
7 Soft tissue defects about the elbow are potentially disabling injuries, leaving exposed bone, joint, or tendon. Muscle or tendon substance loss or nerve injury can result in functional loss at the elbow. Because local tissue may be involved in the zone of injury, it is useful to have several reconstructive options available for the treatment of soft tissue loss about the elbow. The particular method of coverage should be tailored to the size and etiology of the defect, in addition to the general health and needs of the patient. The goals in treating soft tissue defects are to provide wound closure, decrease risks of infection, decrease tissue edema, and allow early mobilization and rehabilitation of the elbow. The elbow is a difficult joint to rehabilitate, even after minor trauma. In the face of injury associated with soft tissue loss, functional rehabilitation becomes more difficult because of the wider zone of injury, increased edema, and structural injury or loss. Early reconstruction of all injured structures, including the soft tissue defect, is of paramount importance in maximizing functional recovery. This chapter addresses the treatment of large soft tissue defects, which cannot be addressed by skin grafts or local random fasciocutaneous flaps. The role of prophylactic tissue transfer in addressing the soft tissue envelope of the elbow will be discussed. Soft tissue coverage about the elbow is indicated for cases of extensive soft tissue loss, particularly those injuries associated with functional losses or exposed bone, joint, or implant. There are a few clinical situations where we feel the use of supplemental soft tissue coverage may be beneficial, even though primary skin closure can be achieved. These cases include severely contused skin directly overlying hardware or prostheses and if the quality of tissue is thin, scarred, or poorly compliant. This may occur in the multiply operated elbow, where the subcutaneous tissue has become progressively more thin and less mobile, and in cases of previously irradiated tissue. The pedicled latissimus dorsi is an excellent donor for prophylactic soft tissue augmentation. The use of the latissimus as a prophylactic rotational muscle about the elbow is similar to the use of the prophylactic gastrocnemius rotational flap for reconstructive procedures about the knee.1 Providing a muscular soft tissue envelope at the elbow reduces the risks of tissue breakdown over prominent bone or implants, promotes bone and tissue healing by improved vascularity, and reduces risks of deep infection by improved vascularity and improved tissue durability overlying the implants, as well as improved antibiotic delivery.2–6 In selecting a method of coverage, surgical considerations include wound factors, donor site factors, and the general health of the patient. Wound factors include not only the size and depth of the defect, but also the cause of the soft tissue injury and any structural or functional losses. Local tissue flaps may be included in the zone of injury and cannot be used in reconstruction. Skeletal injuries requiring stabilization often lead to exposed or prominent implants. Muscle or nerve injury may result in functional deficits, which should be simultaneously treated with the soft tissue reconstruction. Donor site considerations include tissue availability, suitability of the donor tissue in providing adequate coverage for the size of the defect, tissue thickness, and tissue mobility. Donor site cosmesis and acceptable functional loss are important factors in deciding the method of treatment. Whatever the selected donor site, it should ideally allow early motion at the elbow.7,8 Primary closure or delayed primary closure is useful for small soft tissue defects, where there is no immediately underlying bone, joint, dead space, or implant. Primary closure is limited by the size of the defect and the elasticity and vascularity of the surrounding skin. When the skin cannot be approximated by undermining skin edges, commercially available skin closure devices allow gradual tissue stretching over a period of minutes to hours. Split-thickness or full-thickness skin grafting is appropriate for any size defect that has a tissue bed that will accept a graft. Skin graft will reliably provide coverage over exposed subcutaneous tissue, muscle, tendon with paratenon, or bone with periosteum. The latter two conditions may be undesirable as recipient tissue bed because skin graft directly overlying tendon or bone can result in an unstable scar susceptible to breakdown. At the dorsal surface of the elbow, split-thickness skin graft should be used with caution because this does not provide durable coverage. Local skin flaps can be used to close small defects when primary closure creates excessive tension on tissue margins or where a small defect is not amenable to skin grafting, for example, an area over a bony prominence or over an exposed tendon. Although these flaps have the advantage of providing wound closure with similar texture skin, they have limited applicability in the upper extremity due to the relatively poor vascularity and limited tissue mobility. Local random flaps are not based on any vascular pattern or pedicle but are perfused through dermal and subdermal plexi. The types of local cutaneous flaps include the triangulation of adjacent parallelogram, Z-plasty, or double rhomboid Z-plasty. The double-rhomboid Z-plasty helps to decrease tension along the line of closure of the donor site and at the flap corners. All local flaps are limited by the mobility, elasticity, and vascularity of the adjacent skin. Creating flaps with greater than 1:1 length to width ratio can lead to edge necrosis of the flap.8,9 Axial fasciocutaneous flaps are based on recognized arteriovenous systems, which supply a defined territory of skin and subcutaneous tissue. These can be harvested as wide-based peninsular flaps or as island flaps, where the pedicle is fully mobilized. Peninsular flaps do not require isolation of the pedicle and are usually used as transposition flaps. Because they are aligned along a vascular pedicle, a longer length to width ratio flap can be safely elevated. Several of these flaps have been described in the upper extremity.10–16 These flaps can be harvested quickly and use similar textured skin for covering the defect. They can often include a sensory nerve, creating a sensate flap. Island flaps are similar to the peninsular flap; however, the vascular pedicle is isolated and mobilized. This allows greater versatility in coverage because of the increased arc of rotation. Most of these flaps also can be taken as free flaps. Examples in the arm and forearm include the lateral arm flap,12,15,17–24 the posterior interosseous flap,12,15,17–26 the ulnar artery flap,27 and the radial forearm flap.28–30 Distant pedicle flaps are one of the most reliable means of coverage of large soft tissue defects when recipient vessels are not available or when the patient is a poor candidate for other types of reconstruction. These flaps rely on the vascularity of the recipient tissue bed and do not bring a permanent independent blood supply to the defect. They have been reported to cover defects as large as 22 cm in length.31 Although seldom used, they remain an important reconstructive option in select patients. The main limitations of these flaps are related to the prolonged immobilization required for two-stage procedures, which significantly compromises functional recovery. Increased difficulties are encountered not only with stiffness and contracture at the elbow and shoulder, but also with edema and stiffness of the hand and fingers. Distant pedicle random pattern flaps from the chest wall or upper abdomen have been largely replaced by the use of axial patterned flaps. Because of the random pattern of vascularity, the length of these flaps usually is limited to 10 cm, requiring close approximation of the arm against the chest. Flap division is performed at 3 weeks.32 Distant pedicle axial patterned flaps from the abdomen also have been described.31–36 The thoracoepigastric flap is a fasciocutaneous flap, designed along the internal mammary and superior epigastric arteries. The flap is anteriorly based and is oriented with its superior border along the inferior mammary crease. Because it is anteriorly based, it is best used to cover anterior soft tissue loss around the elbow. The flap is limited to approximately 25 cm in length (not to extend posterior to the posterior axillary fold). Widths less than 8 to10 cm usually can be closed primarily.33,35 The external oblique fasciocutaneous flap provides a thin posteriorly based flap. The flap size is limited to 6 to 8 cm in width (to allow primary closure of the donor site) and 16 to 18 cm in length. The blood supply is through segmental vascular pedicles entering the lateral aspect of the external abdominal oblique muscle, sending perforators into the fascia and subcutaneous tissue layers. Usually two pedicles are incorporated into the flap, which can be divided at 2 to 3 weeks. Because of its posteriorly based pedicle, it is well suited to cover defects along the posterior aspect of the elbow.34 The transverse rectus island flap has been more recently described for elbow joint salvage. A musculocutaneous flap based on the superior epigastric artery is harvested. The fasciocutaneous portion of the flap is inset, providing the soft tissue coverage. The rectus muscle acts as a leash for the pedicle, allowing a greater pedicle length and arc of rotation.31,36 Additional surgical requirements for flap division and subsequent flap contouring are another source of morbidity. At the time of flap division, if there is any suspicion of compromised circulation to the flap, a 7- to 10-day delay in final insetting at the recipient site will reduce the risk of flap necrosis. Donor site cosmesis is of greater concern when the donor site cannot be closed primarily. These flaps also have been critiqued for their bulk and need for secondary surgeries for contouring. Local muscle rotational flaps can be used to cover small defects about the elbow where there is exposed nerve, vessel, tendon, bone, or implant. Their arc of rotation generally allows for coverage of anterior and posterior wounds. Several local muscle rotational flaps have been described in small series, often only as case reports.37 These include the brachioradialis,37–40 the extensor carpi radialis longus,41,42 the anconeus,37,43 and the flexor carpi ulnaris.37,44 The brachioradialis and the extensor carpi radialis longus also have been used as musculocutaneous flaps. These local flaps are limited to relatively small defects. When not released from the proximal origin, the arc of rotation and ability to achieve posterior coverage are reduced. These muscles often lie within the zone of injury, limiting their use in these situations. The functional deficit at the donor site is not trivial, especially when using the flexor carpi ulnaris, which is the strongest flexor and ulnar deviator at the wrist. The latissimus dorsi rotational flap is the only distant pedicled muscle rotational flap that consistently provides coverage of moderate to large soft tissue defects about the elbow.1,2,45–56 It has been shown in a cadaveric study to consistently provide soft tissue coverage on average 6.5 to 8 cm distal to the olecranon. When released from humeral insertion, an additional 2 to 3 cm of distal coverage often can be achieved.48 The muscle and its neurovascular pedicle lie well away from the elbow and are generally outside the zone of injury. Because this is a one-stage procedure, rehabilitation can be started within the first week of reconstruction. When local rotational flaps or distant one-stage pedicle flaps are not suitable for soft tissue reconstruction, free tissue transfer should be considered. Free tissue transfer may provide the best functional and cosmetic outcome and can be performed as a single-stage reconstruction, allowing early rehabilitation of the elbow.5,51,57–59 Selection of the donor site depends on several factors. These include the size and location of the defect, any underlying structural or functional deficit, the presence of exposed or prominent implants, and the general health status of the patient. For example, functional morbidity at the donor site is more critical in the polytrauma patient, who is already functionally compromised. Many options for free tissue transfer exist; these include fascial, fasciocutaneous, muscle, and musculocutaneous flaps. Fascial free flaps can be used for small defects that do not require the filling of a dead space. More commonly used fascial flaps include the temporoparietal fascia, radial forearm fascia, and parascapular fascia. They are particularly useful in the hand, where they provide thin, pliable coverage and allow tendon gliding. Around the elbow, however, they do not have adequate durability to withstand the mechanical stresses around the posterior aspect of the elbow. Several fasciocutaneous flaps are available, many of which already have been described. These include the lateral arm flap,60 radial or ulnar forearm flap,61,62 groin flap, scapular and parascapular flaps,6 and medial and lateral thigh fasciocutaneous flaps.63 The lateral arm and radial and ulnar forearm flaps can be taken as sensory flaps, which can be important in providing protective sensation over areas subject to pressure breakdown. Despite this advantage, these flaps have some donor site morbidity, with complaints of chronic aching, dysesthesias, and poor cosmetic appearance.20,28,64 Muscle free flaps can be used to cover large defects about the elbow. When covered with split-thickness skin graft taken as a sheet (nonmeshed), they have excellent cosmetic results at both the donor and the recipient sites. They also provide a rich and independent blood supply, improving vascularity, promoting healing, and reducing the risk of sepsis. Several donor muscles are available. Selection of the donor muscle depends on the size of the soft tissue defect, the requirements to fill dead space, cover implants, the need for functional restoration, and the patient comorbidities. Options include the latissimus dorsi, serratus anterior, rectus abdominus, and gracilis. The most commonly used flaps are the latissimus dorsi and the rectus abdominus, based on their limited donor site morbidity, vascular reliability, and accessibility (Figure 7-1). Disadvantages of muscle flaps include longer and more complex surgery, functional loss at the donor sites, and risk of flap failure. The risk of flap failure is especially important in the patient with multiple injuries, where every functional unit should be preserved. FIGURE 7-1. Free rectus transfer. A 27-year-old woman sustained a shotgun injury to her right elbow with anterior and anterolateral soft tissue loss. The joint, proximal radius, and radial neck fracture were exposed. The proximal extensors and distal biceps were absent. The radial nerve was disrupted over a long segment. The patient was treated with irrigation and debridement, open reduction and internal fixation of the radial neck fracture, repair with grafting of the distal biceps insertion, and primary soft tissue coverage with a free rectus abdominus muscle flap. (A). Appearance of the soft tissue injury. (B). Appearance following coverage with a free rectus abdominus (prior to skin grafting). (C). Radiograph at 6 months following stabilization, showing union of the radial neck fracture. (D). Six-month follow-up with final flexion and (E) extension shown. Composite free flaps can be useful in providing soft tissue coverage in conjunction with reconstruction of structural or functional losses. Both the composite lateral arm flap and the composite radial forearm flap can include both vascularized tendon and bone along with the fasciocutaneous graft.18,65,66 Larger bone defects can be reconstructed with the vascularized osteofasciocutaneous free fibula graft.67,68 The flexor carpi ulnaris (FCU) muscle for use as a rotational flap has been well described in anatomical studies.25,37 Its clinical use has been described principally in case reports.44 This flap has been described as both a muscle rotational flap and a musculocutaneous flap. As the dominant wrist flexor and ulnar deviator, it should not be sacrificed routinely and in general should be used only when other alternatives do not exist. The principal indications for use of the FCU muscle include coverage of the anterior elbow joint, coverage of neurovascular structures or arteriovenous shunts, and coverage of vascular prosthetic grafts. The use of this muscle for soft tissue coverage is better indicated in patients with diabetes and/or end-stage renal disease. The FCU is the most medial of the superficial flexors of the forearm. It has two heads of origin, the ulnar and the humeral. The humeral origin is on the medial epicondyle. The ulnar origin arises from the proximal posterior border of the ulna. The FCU inserts distally on the pisiform. The dominant pedicle is the posterior ulnar recurrent artery. This branch of the ulnar artery is given off near the level of the bicipital tuberosity of the radius and enters the FCU muscle approximately four finger-breadths below the medial epicondyle. The length of the pedicle is 2 to 3 cm, with a diameter of 1 to 2 mm. One to two minor pedicles are present distally. These are also branches of the ulnar artery. These minor branches can be sacrificed when the muscle is used as a rotational flap. The muscle is innervated by branches of the ulnar nerve, given off below the medial epicondyle. When harvested as a musculocutaneous flap, the overlying skin paddle is supplied by the medial antebrachial cutaneous nerve. The average muscle belly measures 5 cm in width by 20 cm in length. The muscle belly extends to the distal third of the forearm, around 7 to 8 cm proximal to the wrist crease. Based on the dominant pedicle, this muscle can be rotated to cover the anterior surface of the elbow. The posterior surface of the elbow can also be reached, though with greater difficulty. The patient is placed in the supine position. The arm and shoulder girdle are included in the surgical preparation. A sterile tourniquet is used on the proximal arm. The surgical incision is made along a line drawn between the medial epicondyle and the forearm. The middle third of this line is incised, and the musculotendinous junction of the FCU is identified. The muscle is cut at the musculotendinous junction and elevated from distal to proximal. The skin incision is tailored proximally to fit the area of soft tissue deficit. The muscle is mobilized proximally until the length is sufficient to cover the defect. The pedicle does not need to be dissected. The muscle is inset into the defect, and split-thickness skin graft is used to cover the exposed muscle belly. The FCU can also be harvested as a musculocutaneous flap. The area of donor skin lies along the midforearm overlying the FCU muscle belly. A skin paddle up to 6 cm by 10 cm can be harvested together with the muscle, provided that the fasciocutaneous perforators are intact. The skin paddle can be islandized on its perforators to allow greater versatility of coverage. However, this large skin defect can result in poor cosmesis at the donor site. In general, we prefer to use muscle alone and use split-thickness skin graft to cover exposed muscle belly. The brachioradialis rotational flap has been described in case studies for use of coverage about the elbow.38–40 It is best suited to cover small defects along the anterolateral or posterolateral border of the distal arm and proximal forearm. It can be sacrificed with minimal donor site morbidity or functional loss. The muscle has been described as a muscle or musculocutaneous flap. The cutaneous territory lies on the proximal radial forearm between the lateral epicondyle and midforearm and is supplied by perforating musculocutaneous vessels from the underlying muscle. We prefer not to use this as a musculocutaneous flap, as this commonly results in a bulky disfigured appearance to the forearm. The brachioradialis should not be sacrificed in the absence of the dominant elbow flexors. The brachioradialis is the most superficial muscle on the lateral side of the forearm. At its origin, it lies between the brachialis and triceps muscles. It arises from the upper two thirds of the lateral supracondylar ridge of the humerus and from the anterior aspect of the lateral intermuscular septum. The muscle inserts on the radial styloid. The muscle belly extends to the midforearm, at which point it becomes a thin, flat tendon. It acts as a weak elbow flexor, with its strongest action when the forearm is at midpronation. It can initiate both pronation and supination. It is innervated by a branch of the radial nerve, which is given off above the elbow joint. The dominant pedicle is a branch of the radial recurrent artery, close to its origin from the radial artery. The pedicle length is approximately 3 cm, with a diameter of 1 mm. Minor pedicles arise more distally as branches from the radial recurrent artery but are smaller and less consistent. A sterile tourniquet is used for the dissection. The skin incision is made along a line drawn from the lateral epicondyle to the radial styloid. The initial incision begins proximally and extends to the midforearm. Branches of the lateral antebrachial cutaneous and dorsal ante-brachial cutaneous nerves lie on the superficial surface of the muscle belly. These are identified and preserved and mobilized with the skin flaps. The muscle is exposed both dorsally and volarly, then traced to its musculotendinous junction. The superficial radial nerve and the radial artery are located just volar and deep to the brachioradialis. These should be identified and protected through the remainder of the dissection. The muscle is then released just distal to the musculotendinous junction, leaving a small cuff of tendon to use for insetting the flap. Several small muscle-perforating branches from the radial artery can be safely ligated. This will increase the arc of rotation as the muscle is mobilized proximally. The radial recurrent branch of the radial artery is given off near the bicipital tuberosity of the radius. It is not necessary to identify the dominant pedicle or to release the origin of the brachioradialis. The muscle is rotated to cover the area of soft tissue defect. A subcutaneous tunnel may be useful to reach the defect. This may, however, compress the muscle flap. In general, we prefer to extend the surgical incision and skin graft over exposed muscle belly. The anconeus is a small triangular muscle crossing the lateral elbow. Its function is still debated, although it seems to play a role in elbow stabilization.43,69 Because of its small size, this muscle is rarely used for elbow defects. Schmidt et al43 described three areas of coverage, which include the lateral radiocapitellar joint, the distal triceps tendon at its insertion, and the olecranon. The anconeus can be expected to reliably cover a 5 to 7 cm2 defect. It can be harvested without measurable functional deficit. The muscle origin is located on the posterior aspect of the lateral epicondyle of the humerus. It inserts on the lateral aspect of the olecranon and the adjacent posterolateral olecranon. The muscle size along its maximum dimensions is approximately 3 to 4 cm by 8 to 10 cm. The muscle is supplied through two constant arterial pedicles, the medial collateral artery and the recurrent posterior interosseous artery, which anastomose within the muscle belly. The medial collateral artery is a terminal branch of the profunda brachii. It always travels with the radial nerve branch to the anconeus and enters the muscle on its proximal deep surface. From an arterial standpoint, the anconeus can be mobilized on either its proximal or distal pedicle. However, mobilization on the distal pedicle (recurrent posterior interosseous artery) requires sacrifice of the nerve. The skin incision is centered over the lateral epicondyle and extends obliquely to the lateral border of the olecranon, near the distal insertion of the anconeus. The antebrachial fascia is exposed, and the interval between the anconeus and the FCU is opened. The dissection of the anconeus must be carried to its distal-most insertion, which lies approximately 10 cm from the lateral epicondyle. The tip of the anconeus is subperiosteally elevated from its insertion along the inferior border of the ulna, with attention to preservation of the radiocapitellar joint capsule. The recurrent posterior interosseous arterial pedicle is ligated, and the muscle is mobilized to its origin. The origin can also be released to increase the arc of rotation on its proximal pedicle, the medial collateral artery. If the muscle origin off the lateral epicondyle is released, the proximal pedicle (medial collateral artery) should be identified and protected. Split-thickness skin graft is used to cover any exposed muscle. The radial forearm flap, first described in 1981,70 is the most versatile rotational flap for hand and elbow soft tissue reconstruction. The flap provides thin, durable coverage, which can be a sensate flap when used for elbow coverage. A large skin flap can be harvested alone or with vascularized tendon and/or bone graft.22 Alternately, vascularized fascia alone can be taken as free or rotational tissue.71 The long pedicle provides a wide arc of rotation, allowing for easy circumferential coverage of the elbow (Figure 7-2). A large skin flap can be harvested from the volar aspect of the forearm, from the antecubital fossa to the wrist joint. The flap dimensions depend on the size of the forearm. Most forearms will accommodate a 6 by 15 cm donor area. Two sensory nerves innervate the radial forearm flap: the lateral antebrachial cutaneous nerve, which is a continuation of the musculocutaneous nerve, and the medial antebrachial cutaneous nerve, which is a terminal branch of the medial cord of the brachial plexus. The flap is supplied by perforating branches of the radial artery. These septocutaneous branches arise principally in the distal half of the artery and are capable of supplying the entire skin of the volar surface of the forearm. The venous drainage of this flap occurs through both a deep (venae comitantes of the radial artery) and superficial system (cephalic vein and its tributaries). For a proximally based rotational flap, as would be used for elbow coverage, venous drainage relies on both the deep and the superficial systems. If the flap is rotated distally, the venous drainage relies only on the deep system.72 Before using the radial forearm flap, a careful preoperative assessment is necessary to evaluate the blood supply to the hand. An Allen’s test and Doppler examination of the radial and ulnar arteries should be performed. An incomplete superficial arch or an absent ulnar artery are absolute contraindications for use of this flap. The flap is designed on the volar aspect of the forearm. The flap size and design depend on the size and shape of the defect to be covered. The position of the skin island on the forearm depends on the location of the defect. It should be positioned sufficiently distal to allow the skin island to be rotated to the area needing coverage. The dissection is performed under tourniquet. The course of the radial artery is approximated along a line drawn from the biceps tendon to the radial side of the flexor carpi radialis tendon at the proximal wrist crease. The skin island is marked. The incision is started distally, identifying the cephalic vein, brachioradialis, radial artery, and flexor carpi radialis. The skin paddle is incised down to the antebrachial fascia. The fascia is sharply divided in line with the skin incision. The fascia is tacked to the subdermal layer with a 4-0 absorbable suture to prevent shearing injuries to the fascial perforators. Dissection is then continued in the sub-fascial plane, beginning on the ulnar side of the flap. The flap is elevated to the radial artery. It is critical to stay above the paratenon throughout the dissection. As the dissection approaches the radial artery, the intermuscular septum must be included in the dissection to preserve the septocutaneous perforators, which supply the skin paddle. The flap is then elevated from the radial side in the same fashion. If there is any concern about vascularity to the hand, prior to ligating the radial artery, the artery may be provisionally clamped with a microvascular clamp and the tourniquet released. The perfusion of the hand is checked, and if satisfactory, the arm is re-exsanguinated and the tourniquet is rein-flated. The radial artery and cephalic vein are ligated in the distal incision site, and the remainder of the flap is elevated together with the radial artery and cephalic vein. Depending on the distance to the defect, the radial artery and its venae comitantes can be traced proximally as far as the bifurcation of the brachial artery to allow a greater arc of rotation. The flap is inset into the defect in a standard manner.
Soft Tissue Coverage of the Elbow
Treatment
Indications
Preoperative Planning
Coverage Options
Primary Closure
Skin Grafting
Local Random Flaps
Axial Fasciocutaneous Flaps
Distant Pedicle Flaps: Two-Stage Flaps (TemporaryPedicle Flaps)
Local Muscle Pedicle Flaps
Distant Muscle Pedicle Flaps: One Stage
Free Tissue Transfer

Surgical Technique
Flexor Carpi Ulnaris
Specific Technique
Brachioradialis
Specific Technique
Anconeus
Radial Forearm Rotational Flap
Specific Technique
Soft Tissue Coverage of the Elbow
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








