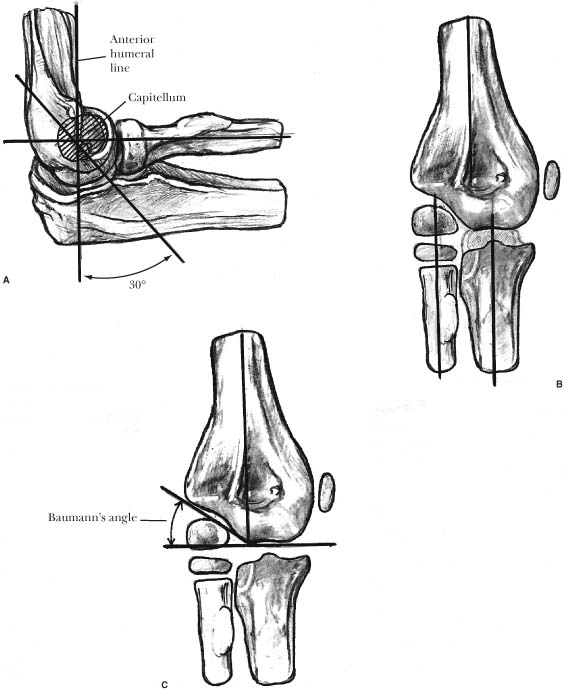
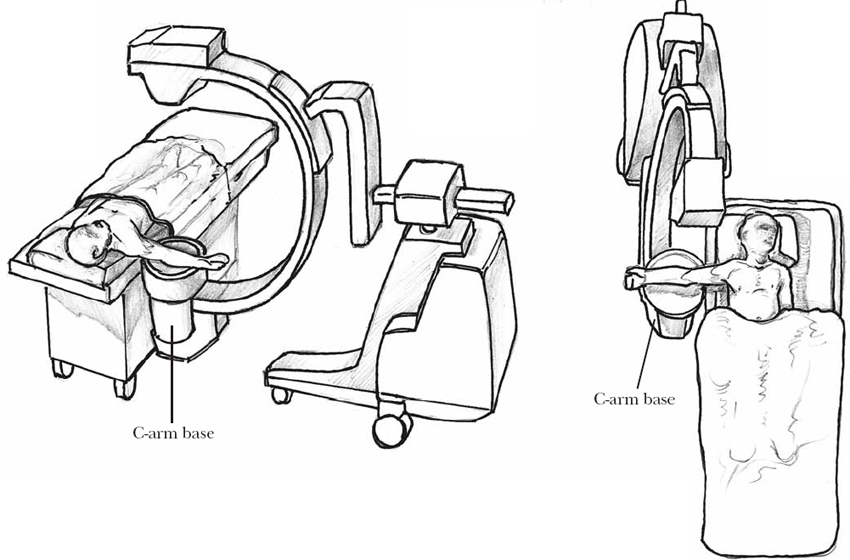
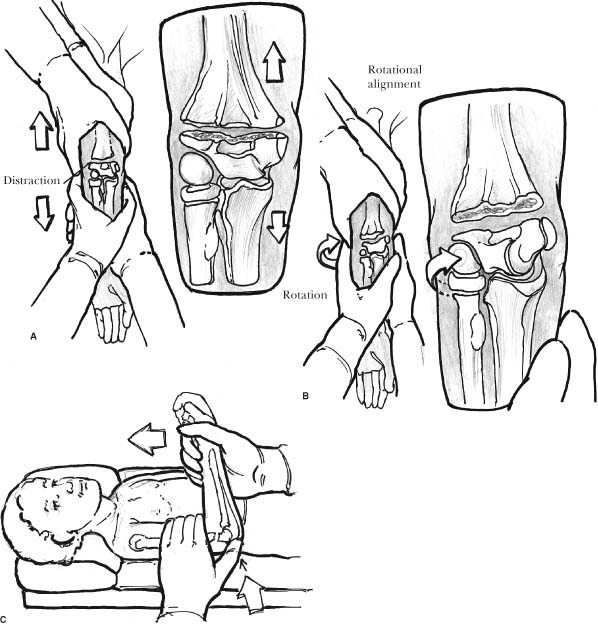
9 Elbow fractures are very common in children and often pose significant treatment challenges. Physical examination can be difficult, given the large amount of swelling present and the challenges with patient cooperation, especially in very young children. The developing ossification patterns and variable fusion of secondary growth centers can complicate radio-graphic analysis. Both acute and long-term complications abound, including neurovascular injury, compartment syndrome, malunion, loss of motion, and post-traumatic arthritis. These potential pitfalls may be responsible for the shift away from nonoperative treatment toward increased percutaneous or open methods of fixation. Despite trends to more aggressive treatment, techniques vary drastically from those used to treat adult elbow fractures. As with any fracture about the elbow, standard antero-posterior (AP) and lateral projections are mandatory for accurate diagnosis. Oblique views can help delineate the pattern of complex fractures or assist in determining absolute fragment displacement. On rare occasions preoperative ultrasound, CT scan, or intraoperative arthrogram can be of further benefit. The secondary centers of ossification about the elbow appear and fuse in a predictable pattern. Although there is patient variation in exact age of appearance, the general order of ossification is unchanged and can be remembered by the mnemonic CRITOE (capitellum, radial head, internal (medial) condyle, trochlea, olecranon, external/lateral condyle). Understanding the osseous development of the elbow can prevent misdi-agnosing an ossification center for a fracture, while also allowing one to detect a change in the normal relationship between these growth centers. When doubt exists, comparison views of the contralateral, uninjured elbow can help distinguish injury from a normal ossification center. Anatomic relationships of the distal humerus, proximal radius, and proximal ulna must be critically evaluated, especially in very immature patients, to ensure a fracture of nonossified cartilage is not missed. These relationships are also critical when evaluating the quality of fracture reduction (Figure 9-1). The anterior humeral line should bisect the capitellum on a lateral projection. The proximal radius should point to the center of the capitellum in all views. Any displacement is abnormal and warrants further evaluation for congenital abnormality, fracture, or dislocation. Similarly, the long axis of the ulna should be parallel and slightly medial to the long axis of the humerus on a true AP radiograph. The Baumann’s angle is most useful for judging postreduction alignment and should be 10 to 25 degrees in most patients.1 Comparison views of the contralateral uninjured extremity can help control for individual variations in alignment and bony development. The visualization of the fat pads can also hint at an occult fracture. Skaggs and Mirzayan2 have shown that 76% of children with a history of elbow trauma and an elevated posterior fat pad had radiographic evidence of fracture healing at an average of 3 weeks after injury despite the fact that the AP, lateral, and oblique radiographs at the time of injury showed no sign of fractures. FIGURE 9-1. Osseous anatomy of the elbow. (A). A line drawn along the anterior cortex of the humerus should bisect the capitellum. A line drawn along the proximal radius, in any projection, should bisect the capitellum. (B). On anteroposterior projection, a line through the ulnar or radial shaft should be parallel to a line through the humeral shaft. (C). On anteroposterior projection, a line drawn along the capitellar physis and a line perpendicular to the humeral shaft form Baumann’s angle. Fractures of the supracondylar humerus are the third most common fracture in children, following fractures of the hand and distal radius. Nevertheless, supracondylar humerus fractures remain the most commonly operated fracture in pediatric patients. Operative fixation is now the mainstay of treatment for displaced fractures, to prevent malunion in extension and resultant loss of elbow flexion, as well as cubitus varus. Surgical stabilization decreases hospital stay, but more importantly it allows splinting in extension. This relieves pressure in the antecubital fossa, decreasing the risk of neurovascular compromise, compartment syndrome, and Volkmann’s ischemic contracture. The incidence of supracondylar humerus fractures is greatest in the first decade of life, with a peak between the ages of 5 and 8 years. The vast majority of supracondylar humerus fractures occur during a fall on the outstretched hand, with elbow hyperextension, resulting in posterior displacement and the classic extension-type injury. Rarely the fracture is caused by a direct fall on the posterior elbow, resulting in an anteriorly displaced flexion-type injury. Displacement tends to be greater in older children because of the larger injury force required to result in fracture. Physical examination will demonstrate mild to severe swelling about both the medial and lateral elbow. With higher energy injuries, ecchymosis may be present in the anterior or posterior elbow. Neurovascular examination is critical, as both neurologic and vascular insults can occur. The anterior interosseous branch of the median nerve is most commonly injured, followed by the radial nerve. Compression or injury of the brachial artery can occur with widely displaced fractures. Radiographic evaluation includes both AP and true lateral projections of the elbow. Oblique views can be helpful in nondisplaced fractures, as can the presence of a posterior fat-pad sign. The modified Gartland classification is most commonly used to guide treatment. It is based on the amount of displacement seen on orthogonal radiographic projections. Nondisplaced Gartland type I fractures are treated for 3 weeks with cast immobilization at 90 degrees of elbow flexion. Gartland type II fractures are posteriorly displaced on an intact posterior periosteal hinge. Although these fractures can be treated with reduction and cast immobilization, the elbow must be in extreme flexion to prevent redisplacement of the distal fragment. This significant flexion, combined with the soft tissue swelling that often results from the injury, jeopardizes the vascularity of the forearm and hand.3 Thus, the vast majority of these injuries are treated surgically with closed reduction and percutaneous pin fixation.4 Gartland type III fractures are both posteriorly and rotationally displaced, without an intact periosteal hinge, necessitating closed reduction and pin fixation in most patients. A small percentage of patients will require open reduction for an extension-type injury. The need for open reduction may be increased in flexion-type fractures. Patients with open fractures require surgical debridement and fracture fixation. Those with vascular insult that does not improve with fracture reduction and stabilization may warrant surgical exploration and vascular repair.5 Closed manipulation is nearly always sufficient to obtain reduction of supracondylar fractures, but it does require general anesthesia and image intensification. The room setup and C-arm positioning should be carefully planned for all upper extremity fracture reductions, especially in those patients with unstable fractures (Figure 9-2). The method of reduction is similar for both Gartland type II and III extension fractures. After gradual longitudinal traction has been applied to restore length, an AP image of the elbow is performed (Figure 9-3). Residual medial or lateral displacement, varus or valgus angulation, and malrotation are corrected during maintenance of longitudinal traction. Concomitant hyper-extension through the fracture site can help unlock interdigitation of the proximal and distal fragments. The Baumann’s angle, as well as comparison of the carrying angle with the contralateral uninjured extremity, can be used to judge acceptability of coronal plane alignment. Only after length and coronal alignment are restored is the elbow flexed. Longitudinal traction is maintained during flexion. A thumb can be placed on the olecranon to help with reduction of the distal fragment in the sagittal plane. The triceps acts as a temporary posterior tension band, while forearm pronation helps lock the fragments and maintain reduction. Image intensification is necessary to verify the coronal and sagittal plane alignment prior to pin fixation. A Jones view allows evaluation of the medial and lateral columns of the distal humerus. The arm, or with more unstable injuries the image intensifier, can be rotated to obtain a true lateral projection. If rotating the arm, external rotation is preferred to prevent loss of reduction. Two divergent laterally placed 0.062 inch Kirschner wires are the preferred method of stabilization in the vast majority of patients. Stability of the distal fragment is then assessed using fluoroscopic imaging. A third lateral Kirschner wire can be added to enhance fixation strength (Figure 9-4). To avoid iatrogenic injury to the ulnar nerve, a medial Kirschner wire is used only in the most severe fractures, when isolated lateral fixation provides insufficient stability.6 If a medial Kirschner wire is deemed necessary, it should be placed with the elbow in relative extension (15–30 degrees of flexion) to prevent the ulnar nerve from subluxating anteriorly or draping tightly against the medial epicondyle. When the ulnar nerve is palpable, it can be protected from Kirschner wire impalement by the surgeon’s thumb. When not palpable, a small incision can be made at the medial epicondyle to ensure protection of the nerve during Kirschner wire fixation. FIGURE 9-2. Room setup. The C arm is placed parallel to the operating table and can easily rotate around the extremity to provide anteroposterior, lateral, or oblique projections. This is particularly useful with unstable fractures in which movement of the extremity may cause loss of reduction. In those fractures where closed manipulation is unsuccessful, soft tissue is often interposed in the fracture site. A buttonholed brachialis muscle can be “milked” away from the proximal fragment to allow closed reduction. When this fails, open reduction is necessary. A longitudinal medial or lateral approach, centered at the apex of the subcutaneous proximal fragment, allows excellent exposure to remove the block to reduction. When incising the skin, care must be taken to ensure no neurovascular structures are injured, as they can often be draped over the proximal fragment just below the dermis. After clearing the fragment of interposed soft tissue, the standard closed reduction maneuvers can be applied. A more formal open reduction may be needed if there is poor fragment stability. For open fractures, extension of the traumatic wound provides ample exposure for debridement and fracture reduction. A standard anterior approach is used for cases requiring vascular repair due to a poorly perfused hand. Flexion-type injuries can be more difficult to reduce. Longitudinal traction allows restoration of length and coronal plane alignment as in extension-type injuries. Flexion of the elbow, as would be done for an extension type injury, results in further fracture displacement. Thus, an extension force is placed on the distal fragment, over a posterior bump, to restore sagittal alignment. Widely displaced fractures often require open reduction through either a medial or a lateral approach. Percutaneous Kirschner wire fixation is identical to that used in extension-type injuries. FIGURE 9-3. Reduction maneuver for supracondylar humerus fracture. (A). Longitudinal traction is used to gain length with the elbow in full extension and the forearm supinated. (B). Varus/valgus or rotational malalignment is then corrected. (C). The elbow is flexed while maintaining longitudinal traction. The thumb can be used to apply an anterior force on the distal segment to help reduce fracture. Following fixation, the extremity is immobilized in a well-padded cast or posterior splint in 45 degrees of elbow flexion. This prevents compression of the neurovascular structures in the antecubital fossa. Patients with severe swelling are elevated in an Osbourne sling for 24 to 48 hours. Immobilization is removed after 3 weeks, at which time radiographic callus is sufficient to allow Kirschner wire removal in the office. Active range of motion is started, but sports are restricted for an additional month. Six weeks after pin removal the vast majority of children have regained full, symmetric elbow range of motion. Physical therapy can be beneficial in the few patients with stiffness. FIGURE 9-4. Supracondylar humerus fracture. Preoperative anteroposterior (A) and lateral (B) radiographs. Postoperative anteroposterior (C) and lateral (D) radiographs. Note placement of three lateral pins (rather than use of a medial pin) to improve fixation strength. Neurologic injury and malunion are potential pitfalls for which one must be vigilant. Although the incidence of neurologic injury in displaced extension-type fractures may be as high as 10 to 20%, most recover spontaneously over 6 to 12 weeks.4,5 The anterior interosseous branch of the median nerve is most commonly injured (with posterolateral displacement), followed by the radial nerve, which is at greatest risk with posteromedial displacement. Iatrogenic ulnar nerve injury can occur from medial Kirschner wire placement. Should this occur, the Kirschner wire can be left in place until sufficient callus is present to provide fragment stability, with expectant recovery of nerve function after wire removal. Malunion most commonly occurs due to malreduction or poor fixation stability, rather than to growth arrest. Mild displacement (anterior-posterior) or translation (medial-lateral) can be expected to remodel. However, remodeling will rarely improve residual angulation. Persistent posterior angulation will lead to a loss of flexion, although function may not be impaired. Cubitus varus will also not remodel, but it is usually nonpainful and rarely impacts function. Although there may be an increased risk of future lateral condyle fracture, families are most often concerned with the “gunstock deformity” of the elbow.7 Late osteotomy can be performed to correct such deformity. Transphyseal fractures are a variant of the supracondylar humerus fracture, usually seen in children less than 4 years of age, although they have been reported up to age 6. The most common mechanism of injury is a rotatory shear force, either at birth (due to a difficult or traumatic delivery), due to an unusual fall on the extremity, or as the result of nonaccidental trauma. Abuse must be suspected in any patient with a transphyseal fracture in whom birth injury is not the cause. The vast majority of these fractures are Salter-Harris type I injuries, although Salter-Harris type II fractures can occur. Physical examination reveals moderate soft tissue swelling about the elbow with characteristic “muffled crepitus” on palpation. Complete examination of the child must be performed to rule out signs of abuse. Anteroposterior and lateral radiographs of the elbow are required for diagnosis. Skeletal survey is mandatory if abuse is suspected. Radiographs will resemble those of an elbow dislocation. On AP projection, the proximal radius and ulna maintain their normal relationship with each other but are displaced medially with respect to the distal humerus. On lateral projection, there is posterior displacement of the forearm (Figure 9-5). Although Salter-Harris type I fractures are most common, x-rays should be scrutinized for signs of a metaphyseal fragment indicating a Salter-Harris type II fracture. Posteromedial displacement of the distal fragment or forearm in a child under 4 years of age must be treated as a transphyseal fracture until proven otherwise. If diagnosis is uncertain, comparison views of the contralateral elbow, ultrasound, or intraoperative arthrogram can help further delineate the pattern of injury. Treatment of the displaced transphyseal fracture is similar to that for supracondylar humerus fractures. Closed reduction is performed under anesthesia, utilizing the same reduction maneuver as for supracondylar humerus fractures, and can be held with a cast if there is minimal soft tissue swelling. Our treatment of choice is to stabilize the fracture with two laterally placed, divergent Kirschner wires. Intraoperative arthrogram is performed to confirm reduction (Figure 9-5A,B). Postoperatively, the extremity is immobilized for 3 weeks. When radiographs demonstrate sufficient callus, the pins are removed in the office, and the child is allowed to begin elbow motion. Lateral condyle fractures account for 15 to 20% of all distal humeral fractures in children. They are the second most common pediatric elbow fracture requiring surgical treatment. The most common mechanism of injury is a fall onto the upper extremity, with a varus moment at the elbow and forearm supination. This results in avulsion of the lateral condyle by the extensor muscles and lateral collateral ligament complex. A second mechanism occurs after a fall on a flexed elbow, resulting in compression or shearing of the lateral condyle and fragment displacement. There may be an increased risk of fracture, due to this mechanism, in patients with residual cubitus varus following malunion of a supracondylar humerus fracture.6 Diagnosis can often be made by physical examination. There is isolated lateral elbow swelling without tenderness about the medial aspect of the distal humerus. Anteroposterior and lateral radiographs are generally sufficient for diagnosis. Oblique views can help delineate the true degree of displacement. Milch8 classified lateral condyle fractures based on the location of the fracture line (Figure 9-6). Milch type I fractures are true Salter-Harris type II injuries that cross the ossification center of the lateral condyle. Milch type II fractures extend along the lateral condylar physis and exit medially in the trochlea, similar to a Salter-Harris type IV fracture. Both fractures must be treated with anatomic reduction, if displaced, to restore the articular surface, realign the physis, and reduce the incidence of malunion, nonunion, or growth disturbance. The degree of fragment displacement, rather than the Milch type, is the most useful guide to treatment. Fractures with less than 2 mm of displacement can be treated with cast immobilization.9,10 The elbow is held in 90 degrees of flexion with the forearm pronated and the wrist in relaxed extension. Anteroposterior, lateral, and internal and external oblique views must be obtained after a week in the cast to ensure that no displacement has occurred with resolution of fracture edema. If the overlying cast obstructs radiographic evaluation of the reduction, the cast must be removed, and radiographs must be repeated. The cast is worn for at least 3 weeks or until fracture union is noted.
Pediatric Elbow Fractures
Radiographic Anatomy
Incidence and Mechanism
Classification and Treatment
Surgical Technique
Transphyseal Fractures
Lateral Condyle Fracture
< div class='tao-gold-member'>
Pediatric Elbow Fractures
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree