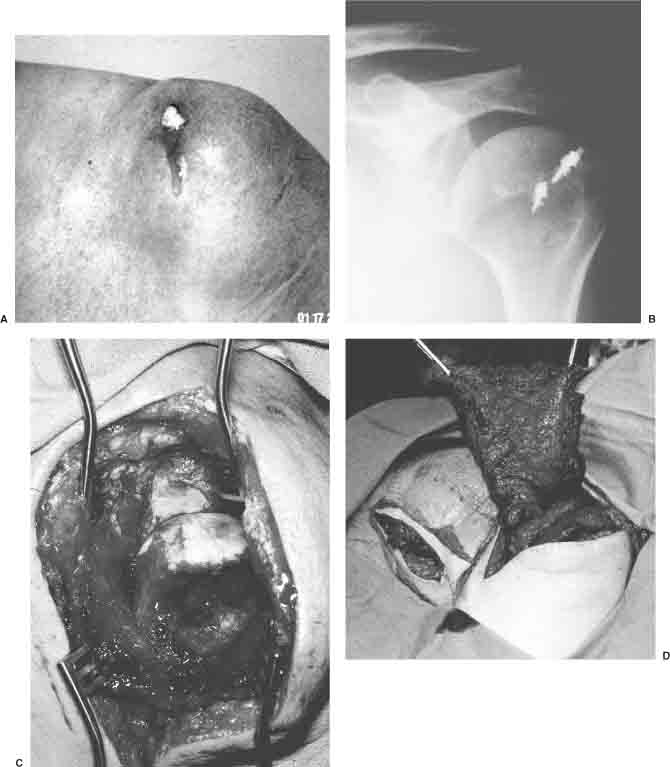
15 Traumatic shoulder injuries are common. However, shoulder injuries associated with soft tissue loss requiring reconstruction are rare. The shoulder joint is covered by a thick soft tissue envelope. The acromion and distal clavicle are the only bony anatomic structures that are not well protected. Extensive soft tissue loss about the shoulder most commonly results from gunshot wounds, direct crush or avulsion injuries, or post-traumatic infection. These injuries rarely occur in isolation but more often with underlying bone, nerve, or vascular injury. The trauma patient must be evaluated and stabilized before addressing the soft tissue defect. Vascular injuries are repaired immediately. Bone, articular, and nerve repair and reconstruction should be addressed simultaneously with soft tissue coverage. Early and reliable soft tissue coverage allows for early joint mobilization and rehabilitation. Selection of the type of coverage to be used must consider the wide range of motion of the shoulder girdle and should be supple enough to accommodate these requirements. Although small soft tissue defects about the shoulder may be amenable to local rotational flaps or skin grafts, this chapter will focus on large defects requiring large muscle or fasciocutaneous rotational flaps or free tissue transfer. The use of functional tissue transfer in conjunction with soft tissue coverage will also be discussed. Soft tissue defects about the shoulder that require surgical intervention are those with exposed fracture, joint, hardware, or prosthesis. Soft tissue injury with associated functional loss may also be a relative indication for soft tissue reconstruction about the shoulder girdle. Planning the reconstruction includes careful evaluation of the zone of injury and any functional losses. The remaining intact structures that might be used for reconstruction need to be evaluated carefully for any signs of injury to the anticipated donor site. The underlying bone, joint, or nerve injury must be considered in planning. These underlying injuries may limit the anticipated goals of functional recovery and may affect the selection of the donor tissue. Planning the reconstruction includes careful evaluation of the zone of injury. Local structures that may be used for coverage might also be involved in the zone of injury. Severely contused muscle has a higher risk of failure, even when used as a rotational flap. Functional losses due to muscle or nerve injury can be reconstructed simultaneously with soft tissue coverage. Nerve injuries may be less obvious when bone, joint, and/or muscle injury is severe. Careful examination in conjunction with a high index of suspicion can aid in identifying injured structures and in selecting the best type of coverage. Small soft tissue defects about the shoulder can often be treated with random fasciocutaneous rotational flaps or skin grafts. Defects that result in exposed bone, joint, or neurovascular structures more often need larger fasciocutaneous flaps, muscle rotational flaps, or free tissue transfer. Several muscle and fasciocutaneous flaps have been described to provide coverage about the shoulder. Rotational fasciocutanous flaps include the lateral arm flap, the medial arm flap, the lateral thoracic flap, and the scapular and parascapular flaps. With the exception of the lateral arm and the parascapular flap, the rotational fasciocutaneous flaps principally provide coverage of the axilla.1–7 Muscle flaps that have been described include the deltoid, caudal trapezius, triceps, serratus anterior, pectoralis minor, pectoralis major, and latissimus dorsi.8–17 The most versatile flaps with the least donor site morbidity are the latissimus dorsi, pectoralis major, and parascapular flaps. In general, shoulder girdle defects are easily managed with local rotational flaps. When this is not possible, free tissue transfer can be used for coverage or functional reconstruction. Available donor sites include the contralateral latissimus dorsi and the parascapular flaps off the subscapular arterial system. A functional free gracilis can provide coverage and simultaneously restore function. Many other free muscle and fasciocutaneous flaps have been described but are beyond the scope of this chapter. Available recipient vessels include the thoracodorsal artery, the thoracoacromial trunk, the profunda brachii, and the transverse cervical artery. For venous outflow, venae comitantes or the cephalic vein or its tributary branches can be used. The latissimus dorsi is the most useful and versatile pedicle muscle flap. It is the largest available muscle that can be used as a rotational or free flap. The area of coverage can be extended by including the inferior three slips of the serratus anterior.11,18 The latissimus can be harvested with limited donor site morbidity.19,20 It can be used solely as a muscle flap or as a myocutaneous flap. When significant skin loss is present, a myocutaneous flap can be used to provide not only coverage of underlying structures but also a more cosmetic reconstruction (Figure 15-1). The latissimus is supplied by the thoracodorsal artery, which arises from the subscapular artery. The pedicle length ranges from 8 to 11 cm, with vessel diameter between 2 and 4 mm. The muscle can be fully mobilized on its pedicle and rotated to cover defects on the anterior, posterior, and superior aspects of the shoulder. When reconstruction of functional loss is needed in conjunction with soft tissue reconstruction, the latissimus is a useful rotational donor for reconstruction of the anterior deltoid, biceps, or triceps.21–24 It can be mobilized and transferred to reconstruct rotator cuff function. However, when used in this manner, the latissimus provides little coverage of the shoulder girdle. The traumatic wound at the shoulder should be thoroughly debrided. Successful soft tissue coverage requires a clean, infection-free bed. A muscle flap or a musculocutaneous flap is selected based on the defect that is to be covered. The skin incision follows the course of the latissimus along its midline axis. The incision extends from the axilla to approximately four fingerbreadths cephalad to the posterior iliac crest. If a skin paddle is to be used, it is designed to fit the skin defect at the shoulder. It is important to measure the size of the defect at the completion of the debridement of the traumatic wound. During the dissection of the skin paddle, the incision is beveled away from the skin incision. The incision is carried down to the muscle fascia. Skin flaps are elevated in the suprafascial plane first toward the anterior margin of the latissimus and then toward the posterior margin. The anterior margin of the latissimus is most easily identified and separated from adjacent muscles in the midpoint of the muscle. The anterior margin is mobilized and traced toward its caudal origin. As the iliac crest is approached, the fibrous origin of the latissimus must be tediously dissected from the fibers of the abdominal oblique muscles at the thoracodorsal fascia. The fibrous origin of the latissimus is released from the thoracodorsal fascia, and the muscle is elevated along its deep surface from caudad to cephalad. Deep perforating branches should be identified and cauterized or ligated. As the dissection continues cephalad, care should be taken to identify and protect the distal slips of the serratus anterior and the teres major muscle. The latissimus may be tightly adherent to the chest wall origin of the serratus anterior and to the scapular origin of the teres major, making it difficult to distinguish between the muscle planes. Electrical stimulation of the muscle fibers of the latissimus can help distinguish between the fibers of the latissimus and adjacent muscles. During the dissection toward the axilla, the branch of the thoracodorsal artery, which supplies the distal slips of the serratus anterior, should be identified. The branch origin is variable in location. If the distal slips of the serratus are not to be included in the rotational flap, the branch is ligated close to its take-off from the thoracodorsal artery. We recommend the use of a 2-0 suture-ligature rather than hemoclips, as these may loosen or dislodge leading to significant bleeding. Small perforating branches of the thoracodorsal artery are also ligated. The thoracodorsal artery must be protected from stretching or twisting during the remainder of the dissection. Attention is then directed cephalad to the insertion of the latissimus on the proximal humerus. Releasing the humeral insertion of the latissimus allows greater mobilization of the muscle. Even when greater mobilization is not required, we still release 80% of the insertion. This changes the muscle-resting length and prevents muscle contraction that might disrupt the muscle after it is inset. The remaining intact 20% of the insertion helps prevent traction injury to the pedicle. FIGURE 15-1. Latissimus dorsi flap. A 60-year-old man sustained a shotgun wound to the left shoulder during a hunting trip. He suffered severe injuries, including an axillary artery injury, neuropraxia of the brachial plexus, and bone and soft tissue loss. The axillary artery was primarily repaired with a vein graft. The soft tissue injury was not addressed primarily, and he developed a chronic draining sinus. After serial debridements, a latissimus dorsi myocutaneous flap was rotated to cover the soft tissue defect at the shoulder. (A). Appearance of the shoulder 2 months from injury. (B). Close-up view of the soft tissue defect. (C). Dissected latissimus myocutaneous flap. (D). Appearance at 1-year follow-up, with no evidence of residual infection. The thoracodorsal pedicle is mobilized. We do not separately identify the thoracodorsal nerve. Although some surgeons do sacrifice the nerve when not performing a functional transfer, we spare the nerve in order to preserve some of the muscle thickness and elasticity and limit some of the fibrotic changes that occur in denervated flaps. The muscle can now be rotated on its pedicle to cover defects either on the anterior, posterior, superior, or inferior aspects of the shoulder. The pedicle should not be twisted, and there should be no tension on the pedicle at the time of insetting. The muscle is then inset to cover the area of the defect and to fill any dead space. The muscle margin is inset approximately 1 cm below the surrounding skin flaps. Exposed muscle is covered with split-thickness skin graft. If the latissimus has been harvested as a musculocutaneous flap, the skin paddle is inset to cover the area of skin defect. If the latissimus is to be used for functional reconstruction, prior to releasing the muscle origin or insertion, the resting length of the muscle is marked by placing the arm in full flexion and placing marking sutures in the muscle belly at 5 cm intervals, starting from the muscle insertion and measuring toward the origin. Specific to using the latissimus for functional reconstruction of the anterior deltoid, the muscle should be rotated 180 degrees, such that the latissimus origin is attached to the lateral clavicle, and its insertion is attached to the lateral humerus. When the muscle is inset for functional reconstruction, the resting length must be restored. This is done by insetting the muscle, such that the marking sutures placed at the time of harvesting the muscle are restored to 5 cm intervals. Excess muscle is amputated. The skin paddle, if used, is inset. Otherwise, exposed muscle is covered with split-thickness skin graft. The pectoralis major is most useful for coverage of anterior and superior shoulder defects.25–27 It is a flat, fan-shaped muscle with an average size of 15 by 23 cm. The muscle has sternal and clavicular origins. The tendinous insertion is on the proximal humerus on the lateral lip of the bicipital groove, lateral to the insertion of the latissimus and teres major. The dominant pedicle is the pectoral branch of the thoracoacromial artery. The average pedicle length is 4 cm, and pedicle diameter ranges between 2.0 and 2.5 mm. The pectoralis major is innervated from both the medial and lateral cords of the brachial plexus. The lateral pectoral nerve enters the muscle on its deep surface adjacent to the dominant arterial pedicle. This innervates the clavicular head of the pectoralis and the anteromedial portion of the sternal head of the muscle. The medal pectoral nerve arises as a direct branch from the medial cord, which first innervates the pectoralis minor. After passing through the pectoralis minor, two or three branches are given off to innervate the posterolateral portion of the pectoralis major. Once fully mobilized on the dominant thoracoacromial pedicle, the pectoralis major muscle will easily cover the clavicle, acromion, and anterolateral proximal humerus (Figure 15-2). The surface landmarks for the pectoralis major are the clavicle, which marks the superior border; the sternum, which marks the medial border; and the seventh rib, which marks the inferior border. The anterior axillary fold marks the anterolateral border of the pectoralis. The dominant pedicle enters the deep surface of the muscle approximately 4 cm distal to the clavicle in the line of the junction of the middle and lateral thirds of the clavicle. The patient is placed in the supine position. A small folded towel is placed behind the scapula to elevate the shoulder joint. The chest wall is prepared to the opposite midclavicular line, distally to the umbilicus, and posteriorly to the posterior axillary line. The axilla and entire arm are included in the preparation so that the arm position can be adjusted throughout the procedure. The first skin incision is made transversely on the chest wall between the sixth and seventh ribs. Skin and subcutaneous tissue are lifted as a single layer flap in the plane above the muscle fascia. The entire pectoralis muscle is exposed medially to the sternum and cephalad to the clavicle. The dissection is facilitated by the use of a lighted mammary retractor. When the muscle is completely exposed, the inferior margin of the pectoralis is elevated over a 2 to 5 cm distance from the seventh rib. The interval between the pectoralis major and minor is identified by finding the intermuscular plane along the lateral inferior margin of the pectoralis major. Once this plane is identified, continued elevation of the pectoralis major is continued medially off the chest wall. Again, this is aided by the use of the lighted mammary retractor. The sternal origin is then released as far cephalad as can be safely seen. The more cephalad portion of the pectoralis major has several perforating branches from the internal mammary artery. These enter the muscle around 2 to 3 cm from the midline. For better control of the dissection in this area, a 4 to 6 cm longitudinal incision is made along the lateral border of the sternum just below the clavicle. Through this incision, the medial origin of the pectoralis from the medial clavicle and the cephalad origin of the pectoralis from the sternum can be released. Perforating branches from the internal mammary artery can be cauterized or ligated as necessary and with good visualization and control.
Soft Tissue Coverage of the Shoulder
Treatment
Indications for Surgery
Preoperative Planning
Coverage Options
Surgical Technique
Latissimus Dorsi
Detailed Technique

Pectoralis Major
Detailed Technique
< div class='tao-gold-member'>
Soft Tissue Coverage of the Shoulder
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree