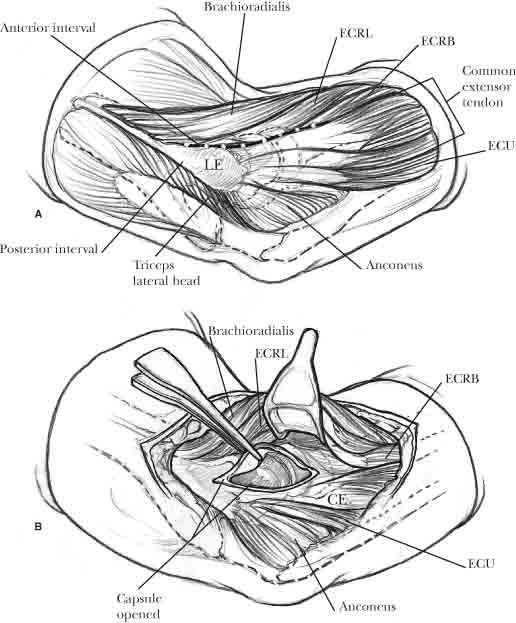
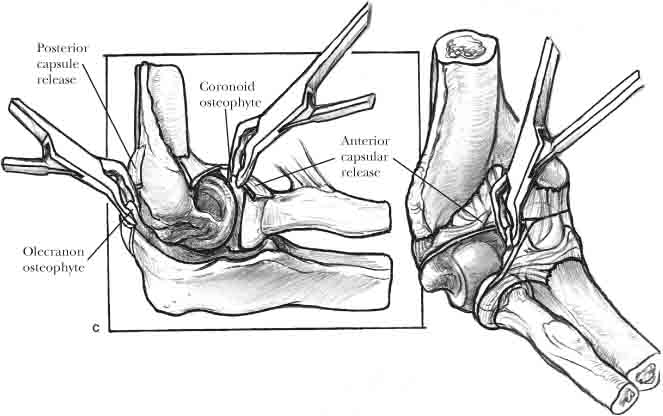
8 Upper extremity function is largely dependent on a functional elbow joint, as the elbow serves to position and stabilize the hand in space in addition to serving as a fulcrum for the forearm and as a load-carrying joint. Terminal hand function is highly dependent on elbow flexion and extension as well as forearm rotation. Subsequently, because of the lack of compensatory motion in the adjacent joints, elbow stiffness is not well tolerated. The elbow possesses a normal range of motion (ROM) from approximately 0 to 145 degrees of flexion, although the functional ROM needed to accomplish 90% of the activities of daily living has been documented to encompass a 100 degree flexion arc (30–130 degrees of flexion) as well as a 100 degree forearm rotation arc (50 degrees of pronation and 50 degrees of supination).1 However, there is significant variability in the ROM needed for different athletic, recreational, and professional activities, and motion beyond these ranges may be required. Flexion contractures of the elbow greater than 40 to 45 degrees usually significantly limit function. A 50% reduction of elbow motion reduces upper extremity function by up to 80%, with significant impairment of hand function.2 However, varying degrees of functional impairment result for different individuals depending on numerous factors such as patient occupation, patient activity level and functional requirements, and the magnitude of the contracture, as well as the location of the contracture in the arc of motion. Certain occupations and activities require more elbow extension than others, and as a result, an arc of motion of 80 degrees between 55 and 135 degrees may be more functionally disabling than the same arc of motion located between 30 and 110 degrees. The normal elbow capsule is thin and filamentous and normally possesses a capacity of approximately 25 ml, rupturing from distention at pressures approaching 80 mm Hg.3 The maximum capsular capacity is present at approximately 80 degrees of flexion, the position in which minimal intra-articular pressure and tension coupled with maximal capsular compliance exist.3,4 In contrast, the stiff elbow capsule possesses a capacity of approximately only 40% that of normal elbows; in addition, capsular compliance is also decreased to less than 15 to 20% of normal.3,4 The significance of this is that the stiff elbow capsule is not merely contracted, but is biomechanically and structurally altered as well. The exact incidence and frequency of elbow contractures is difficult to determine, but it is well documented that trauma is the leading cause of acquired elbow contractures.5,6 Mohan6 published his findings on a series of 200 patients with elbow stiffness and ankylosis and found 38% to be secondary to elbow fracture/dislocations, with another 30% secondary to isolated elbow fractures alone. Other causes of acquired contractures include arthritis (degenerative and inflammatory), burns, infection, and joint paralysis.5 Congenital causes of elbow contractures are far less common and involve numerous conditions such as arthrogryposis, cerebral palsy, and hemophilia, which can cause secondary contractures as a result of recurrent hemarthrosis.5 Elbow contractures typically affect males between the ages of 20 and 65 and usually involve the dominant extremity. Loss of extension is usually the presenting symptom, as pronation and supination may not be significantly limited. In addition, mild to moderate pain is usually present, depending on the extent of underlying degenerative changes. The severity of contractures appears to be highly correlated with the length of elbow immobilization. As a result, there is a trend toward early, protected joint motion that has led to a reduction in the incidence of elbow stiffness. However, residual loss of motion, especially extension, is still common, regardless of the underlying elbow disorder or treatment. Anatomic fracture reduction, coupled with a brief period of immobilization (7–10 days) and a well-supervised physical therapy protocol, is necessary in preventing or limiting the extent of elbow contractures. Gentle active and active-assisted range of motion within the confines of a pain-free range is helpful in maintaining elbow motion. Aggressive passive manipulation is not recommended, as it may potentially lead to the development of heterotopic ossification.5 The post-traumatic stiff elbow can further be classified according to the anatomic location of the underlying contracture(s): extrinsic, intrinsic, and mixed.7 Extrinsic elbow contractures refer to involvement of the anatomic structures outside the joint and include capsular contractures, contractures of the surrounding ligaments, and heterotopic ossification. Intrinsic contractures, on the other hand, involve the intra-articular structures and include osteophytes, intra-articular adhesions, articular incongruity, and degenerative changes of the articular surfaces. Most contractures, however, are of the mixed category, consisting of a combination of both extrinsic and intrinsic involvement.5,7 Morrey7 reported that almost all stiff elbows, regardless of etiology, have thickened and contracted capsules along with secondary contractures of the collateral ligaments and surrounding muscles. All of the potential anatomic locations of involvement need to be considered and evaluated to properly treat the stiff elbow. The treatment of the stiff elbow begins with a thorough evaluation of the patient, including a comprehensive history and physical examination. A detailed history must be obtained, including the nature of the initial injury and the associated treatment, the surgical procedures performed (if any), and the timing and nature of any physical therapy undergone by the patient. In addition, any concomitant injuries sustained by the patient—especially the presence of head trauma in the polytraumatized patient—should be determined. The duration of the contracture should also be ascertained, as well as the status of the contracture (improvement vs. deterioration) and the secondary functional impairment. All of the patient’s mitigating factors need to be understood and addressed, such as the patient’s occupation, handedness, and overall activity level. The patient’s understanding of the underlying disability is also extremely important, as patient education and compliance play an important role in the overall treatment of the stiff elbow.5 The next step in the evaluation process is a careful and detailed physical examination. It is important to examine not only the involved elbow, but also the entire extremity and the adjacent joints. The skin and soft tissue surrounding the elbow must be carefully inspected, including any previous incisions utilized, as this has significant ramifications on surgical planning and potential wound complications. The patient’s active and passive ROM must be carefully evaluated and compared with the contralateral extremity. The magnitude and location of the contracture within the arc of motion must be documented as well. Next, an evaluation of elbow stability must be performed to determine the integrity of the capsuloligamentous structures. The presence of valgus or posterolateral rotatory instability needs to be factored into the overall treatment algorithm. Lastly, a thorough neurological examination should be performed to determine the presence of any focal deficits that may potentially compromise overall function of the extremity. Radiographic evaluation of the stiff elbow should begin with standard anteroposterior and lateral views of the elbow. Additional views may be obtained accordingly to provide further details, depending on the nature of the underlying fracture pattern and pathology. Plain radiographs provide an excellent overall picture of the elbow joint, including the ulnohumeral and radiocapitellar articulations. Fracture reduction and hardware position can also be accurately assessed. The presence of marginal osteophytes that commonly occur on the coronoid tip and the olecranon process, as well as ossification of the olecranon and coronoid fossae, can be determined based on proper plain radiographs. Additional radiographic studies may be obtained if more detail is needed. CT scans of the elbow are excellent adjunctive studies that provide a more comprehensive and three-dimensional assessment of overall bony and joint morphology. The presence of osteophytes, loose bodies, degenerative changes, and any articular incongruity can all be well visualized on CT scans. Another benefit of CT scans is the 3D reconstruction, which allows for assessment of joint surface reduction. CT scans accurately characterize the location and extent of heterotopic ossification, which is helpful for preoperative assessment in determining the surgical approach necessary. Bone scans are also used by some surgeons to help determine the maturity of heterotopic ossification, although their use should not be routine. MRI scan of the elbow provide excellent visualization of the soft tissue structures, particularly the musculotendinous and ligamentous structures (e.g., capsular and collateral ligament thickening), as well as visualization of loose bodies.8 MRIs can be a useful adjunctive study but need not be routinely utilized in the management of the stiff elbow. Management of the post-traumatic stiff elbow begins with nonoperative treatment, which has the greatest efficacy within the first 6 to 12 months after onset of the contracture. Contractures with spongy, springy end points at the end ranges of motion—a finding suggestive of soft tissue restraints—are more likely to respond to nonoperative treatment than those with firm end points—a finding indicative of osseous restraints or bony impingement.5 In addition, better responses can be expected with contractures of lesser total duration. The principles and goals of nonoperative management are relatively straightforward and simple. The initial phase of treatment is concentrated on minimizing pain and inflammation in the elbow, followed by a secondary phase aimed at gradually increasing and maintaining a functional ROM. A variety of modalities such as iontophoresis, ultrasound, and electrical stimulation coupled with nonsteroidal anti-inflammatory medications (NSAIDs), ice, and analgesics are used in conjunction with a protracted course of therapy in attempting to achieve those goals. Physical therapy should include active and active-assisted ROM exercises, and should not include forceful or aggressive elbow manipulation, either with or without anesthesia. Aggressive elbow manipulation may lead to capsular tearing and injury with associated local hemorrhage; as a result, patients will subsequently experience increased swelling, inflammation, and pain, and may be at increased risk for the development of heterotropic ossification. In these instances, therapy that is too aggressive will actually be counterproductive in that it may lead to worsening stiffness and pain, creating a vicious cycle of worsening arthrofibrosis.5 Although gentle passive stretching has been shown to have a role in the overall treatment process, physical therapy should not employ aggressive passive stretching of the elbow. Duke et al,9 employing a technique of gentle elbow manipulation in the treatment of 11 patients with contractures, reported no cases of heterotopic ossification with improvement in motion in 6 patients (55%). Splints are a useful adjunct in the overall treatment process that has been shown to have good results.10–13 Dynamic hinged splints are usually not well tolerated by patients because continuous tension is maintained in the soft tissue structures of the elbow, leading to potential muscle spasm and discomfort. Static progressive or “turnbuckle” splints are more commonly used and help to gradually “stretch out” the contracted elbow capsule and surrounding soft tissues. They are adjustable splints that provide patient-controlled gradual stretching and can be used to increase both flexion and extension via an adjustable bolt. These splints are used between therapy sessions, and a 20-hour wear cycle alternating between flexion and extension is generally recommended. Nighttime splinting is an important part of the treatment process and should be focused on the direction (flexion or extension) in which motion is most lacking.5 The results in the literature have generally been encouraging with the proper use of splinting techniques. Green and McCoy10 noted an average increase of 43 degrees in the total arc of motion in 15 patients treated with turnbuckle splinting. Zander and Healy11 reported a decrease in the mean flexion contracture from 44 to 11 degrees that was maintained at 26 months after treatment with a serial casting protocol alternating between flexion and extension. In another study by Bonutti et al12 reporting on 20 patients treated with patient-controlled turnbuckle splints, an average increase of 31 degrees of motion was maintained at 1 year with no complications observed. Gelinas et al13 reported their results of 22 elbow contractures treated with static progressive turnbuckle splinting for a mean duration of 4.5 months, and noted an increase in the mean total arc of motion from 76 to 101 degrees. Nineteen of the 22 patients (86%) had increases in motion, and only 3 patients (14%) went on to require surgical release. The indications for surgery in the treatment of the post-traumatic stiff elbow include failure of nonoperative management, the presence of a chronic contracture greater than 12 months’ duration, and the lack of a functional range of motion, which will vary from individual to individual.5,14 Mansat et al14 have suggested that a flexion contracture greater than 60 degrees or flexion less than 100 degrees constitutes indications for surgery, but in the authors’ experience, the indications will vary and depend on each individual patient’s functional requirements. Some patients with elbow contractures less than 30 degrees that impair occupational functional demands may benefit from surgery if they have failed nonoperative management. In addition, patients with contractures that experience painful popping or locking secondary to intra-articular processes such as loose bodies represent surgical candidates. The surgical alternatives for the treatment of post-traumatic contractures can be categorized according to the underlying nature of the contracture. Extrinsic contractures generally will require open versus arthroscopic capsular releases with or without the adjunctive use of distraction arthroplasty, coupled with excision of heterotopic ossification as needed. Surgical options for intrinsic contractures include open and arthroscopic debridement procedures, ulnohumeral arthroplasty (open vs. arthroscopic), open interpositional arthroplasty, and total elbow arthroplasty. Mixed contractures consisting of both intrinsic and extrinsic causes, as is the case in the majority of post-traumatic contractures, generally will require a combination of the above-listed procedures.5,14 Arthroscopic treatment of the stiff elbow, initially described in a case report by Nowicki and Shall,15 has been made possible by technological advances in elbow arthroscopy. Intra-articular causes of elbow contractures are most amenable to arthroscopic treatment, although many extrinsic causes such as collateral ligament and soft tissue contractures can be adequately treated as well. Arthroscopy is useful for the removal of loose bodies, joint debridement with excision of osteophytes, and capsular releases.16–20 Relative contraindications include any altered neurovascular anatomy such as a subluxating ulnar nerve or the presence of a previous ulnar nerve transposition, as well as any deformities that may have altered the neurovascular anatomy.19 In addition, arthroscopic treatment is extremely technically demanding, and thus limited arthroscopic experience constitutes another relative contraindication. The stiff elbow capsule is noncompliant and thus does not distend as much, decreasing the total capsular volume and placing the neurovascular structures at significantly greater risk during arthroscopy, specifically the radial (posterior interosseous), median, and ulnar nerves.19,20 A diagnostic arthroscopy is first performed following palpation of the anatomical structures and careful portal placement to minimize the risk of neurovascular injury. A systematic approach is then taken, sequentially addressing each of the elbow compartments. Debridement of the posterior compartment involves removal of scar tissue and resection of any osteophytes on the olecranon tip as well as deepening of the olecranon fossa to prevent impingement in terminal extension. Posterosuperior debridement with removal of adhesions between the triceps tendon and the humerus is helpful in increasing elbow flexion. The posteromedial and posterolateral gutters should be addressed to debride potential adhesions as well as to remove any loose bodies that may be present. The radiocapitellar articulation can also be visualized with debridement of any scar tissue or adhesions, as well as excision of the radial head if necessary. Anterior capsular release is another important part of the arthroscopic procedure, with the performance of an anterior capsulectomy to prevent reformation of capsular scarring and to prevent soft tissue barriers to full extension. The coronoid tip can also be debrided anteriorly to remove any osteophytes that may be impinging in terminal flexion.19,20 Jones and Savoie21 reported good results in 12 patients who underwent arthroscopic capsular release for flexion contractures, observing a mean decrease in the overall contracture from 38 to 3 degrees, with mean gains in maximal supination from 45 to 84 degrees and in pronation from 80 to 88 degrees. However, they noted one permanent posterior interosseous nerve palsy in their series.21 In a later study, Savoie and Jones22 presented excellent results of their first 53 patients treated with arthroscopic capsular release and reported an average decrease in the overall flexion contracture from 46 to 5 degrees, with maximum flexion increasing from 96 to 138 degrees, supination from 47 to 86 degrees, and pronation from 75 to 82 degrees. They reported only two failures (4%), one of which required a revision open capsular release. Timmerman and Andrews23 reported similarly encouraging results in 19 patients with post-traumatic arthrofibrosis who underwent arthroscopic debridement and release, noting a mean increase of 29 degrees in the total arc of motion and good to excellent results in 15 patients (79%), with no neurovascular complications. Kim et al24 also presented good results of arthroscopic capsular release and joint debridement in 25 stiff elbows and reported an average gain of 24 degrees of ROM, with 23 patients (92%) reporting satisfaction with their results. In another study, Phillips and Strasburger25 presented 18-month follow-up results of 25 patients—10 with contractures secondary to osteoarthritis and 15 with post-traumatic contractures—who underwent arthroscopic debridement. They noted an average gain in the total arc of motion from 87 to 128 degrees, with no neurovascular injuries and only one patient (4%) requiring an open revision procedure. Kim and Shin20 reported excellent results in 63 patients with elbow contractures treated arthroscopically and noted 92% of patients to have maintained significant gains in ROM at an average follow-up of 42.5 months. The authors noted an improvement in the overall flexion arc from 73 to 123 degrees in cases of post-traumatic stiffness and observed better results in those patients whose duration of symptoms was less than 1 year. In summary, arthroscopic capsular release and joint debridement have been shown to have encouraging results in the treatment of elbow contractures. The advantages of arthroscopy include excellent visualization of the entire joint, as well as maintenance of overall elbow stability secondary to preservation of the collateral ligaments that do not need to be released for the purposes of exposure. Thus, overall morbidity may potentially be decreased. However, arthroscopic capsular release is a very technically demanding procedure with numerous potential pitfalls, especially the risk of neurovascular injury. It should only be performed by surgeons with extensive experience with elbow arthroscopy, and even in those hands must still be performed with meticulous attention to detail. It is a procedure that certainly requires further investigation as long-term studies are not yet available, although technological advances will continue to improve and refine the surgical techniques to maximize functional outcomes. The mainstay of surgical treatment of extrinsic contractures remains open capsular release. There have been a variety of surgical approaches described, although there have been no studies to date comparing the various approaches. The surgical principles, however, remain the same no matter which approach is chosen. The approach(es) utilized must allow access to all relevant pathology within the elbow—all potential structures that restrict motion must be identified and addressed. This includes release of the tight anterior and/or posterior capsule, removal of loose bodies and osteophytes, such as those on the olecranon and coronoid tips that impinge upon terminal extension and flexion, and debridement of all hypertrophic scar tissue and adhesions. Subperiosteal elevation of scarred down muscles (e.g., triceps and brachialis) should be performed to minimize the risk of neurovascular injury while releasing fibrous adhesions that impede motion. The collateral ligaments should be preserved if possible, but severe contractures may require a controlled partial or complete release of the ligaments to gain proper exposure and to perform an adequate soft tissue release. In cases of severe contractures that necessitate a complete or near-complete release of the collateral ligaments, consideration should also be given to the application of an articulating hinged external fixator to maintain joint stability while allowing motion postoperatively.5,14 Removal of hardware and internal fixation should be performed after the capsular releases have been completed to prevent intraoperative fractures that may potentially occur through stress-risers, such as empty screw holes, or through portions of the stress-shielded weakened cortical bone underlying hardware. Fixation from a nonunited fracture should not be removed; rather, the fracture should be rigidly fixed to promote healing and provide osseous stability while allowing elbow motion postoperatively. All heterotopic bone that is restricting motion should be removed as well, and proper hemostasis is important in preventing postoperative bleeding and hematoma formation that may cause pain, swelling, stiffness, and potential further inflammation and ectopic bone formation. It is also important to remember that the range of motion achieved postoperatively is never greater than but is rather almost always less than that obtained in the operating room at the completion of the release.5,14 The volar or Henry approach can be used for cases of elbow flexion contractures without significant posterior compartment involvement. Urbaniak et al26 reported their series of 15 patients in which they performed an anterior capsulotomy for flexion contractures, noting a mean decrease in the overall contracture from 48 to 19 degrees. The best results were obtained in those without significant underlying degenerative changes. Similarly good results were reported by Breen et al27 in their experience with a limited number of patients, as well as by Gates et al28 in another series of 33 patients. In this study, the authors also employed the use of continuous passive motion (CPM) in 18 patients after anterior capsular release, but they did not note any significant differences with or without the use of CPM. They noted an average decrease in the overall flexion contractures of 29 degrees in the non-CPM group and 32 degrees in the CPM group, with no significant heterotopic ossification noted in either group. In summary, the volar approach provides good access to the anterior compartment for anterior capsulotomies, partial release of the anterior portions of the collateral ligaments, release of the brachialis muscle, and potential lengthening of the biceps tendon in severe contractures.5,26–28 However, this approach has limited clinical applications in that posterior pathology—almost always a component of post-traumatic elbow contractures requiring surgical treatment—cannot be addressed. As a result, the volar approach is generally reserved for patients with isolated flexion contractures secondary to anterior capsular scarring without any other significant pathology. The utility of the medial approach has been described for contracture release, as it provides access to both the anterior and posterior compartments of the elbow.14,29–31 Following either a posterior or midline medial skin incision, the medial antebrachial cutaneous nerve is identified, followed by dissection and isolation of the ulnar nerve. Next, the supracondylar ridge and medial intermuscular septum are identified, and the anterior aspect of the elbow can subsequently be exposed by developing the interval in the flexor-pronator mass between the pronator teres and the flexor carpi ulnaris (FCU). The proximal half of the flexor mass may be taken off the epicondyle and the anterior humerus along the intermuscular septum only if necessary for greater exposure. Subperiosteal elevation and retraction of the biceps and brachialis muscles anteriorly off the distal humerus is performed to expose the anterior capsule while protecting the median nerve and brachial vein and artery anteriorly. Alternatively, the posterior compartment can be entered through the floor of the cubital tunnel by elevating the triceps off the distal humerus, with controlled elevation off the olecranon tip if needed. The posterior capsule can then be dissected and released, and other pathology including osteophytes within the posterior compartment may also be addressed. In addition, any heterotopic ossification along the medial elbow can easily be removed through this approach. Lastly, the ulnar nerve may be transposed anteriorly to prevent subluxation and potential neuritis.14,29,30 Hotchkiss and colleagues29 reported an improvement in the mean flexion contracture from 45 to 13 degrees, coupled with an average gain in terminal flexion from 70 to 130 degrees, in seven patients with severe contractures and associated heterotopic ossification treated via a medial approach. These patients were also protected with a hinged distraction fixator postoperatively. Oka30 reported significantly decreased pain and increased ROM that was maintained at an average of 59.5 months in 50 osteoarthritic elbows treated with debridement arthroplasty via predominantly a medial approach. Wada et al31 also reported good results in 14 elbow contractures released through a medial approach. The authors observed an improvement in the mean flexion contracture from 43 to 17 degrees, with an average increase in the total arc of motion from 46 to 110 degrees that was maintained at an average follow-up of 57 months. In addition, significant scarring of the posterior oblique bundle of the medial collateral ligament was observed in all elbows that they believed to be a significant pathologic process that necessitated resection. Bae and Waters,32 utilizing predominantly an extensile medial approach in 13 adolescent post-traumatic contractures, reported improvement in the average total arc of motion from 53 to 107 degrees, with decreases in the average flexion contracture from 57 to 15 degrees that were maintained at an average follow-up of 29 months. Numerous variations of the lateral Kocher approach have been described in the literature for the management of elbow contractures,14,33–37 and the lateral collateral ligament sparing “column” approach popularized by Mansat and Morrey33 is currently the treatment method of choice for uncomplicated extrinsic contractures. Initially described as an extensile ligament-sacrificing procedure, the lateral approach has been modified to preserve the lateral ligaments while providing excellent access to the anterior and posterior compartments. In addition, the lateral approach is the only approach that provides adequate exposure and visualization of the radiocapitellar articulation, specifically the radial head and neck. The relatively avascular lateral supracondylar ridge of the distal humerus is the basis of the lateral “column.”14,33,35 After skin incision, dissection is carried down along the lateral supracondylar ridge distally toward the lateral epicondyle. The anterior compartment is accessed by releasing and elevating the extensor carpi radialis longus (ECRL) and the distal fibers of the brachioradialis off the supracondylar ridge, followed by developing the interval between the ECRL and the extensor carpi radialis brevis (ECRB) (Figure 8-1A). The ECRL and brachioradialis are then retracted anteriorly to reveal the anterior capsule, which is carefully separated from the brachialis muscle anteriorly (Figure 8-1B). Subperiosteal elevation of the brachialis off the humerus with retraction of the entire muscle anteriorly serves to protect the anterior neurovascular structures. An anterior capsulectomy can then be performed, as well as debridement of the anterior compartment and excision of osteophytes on the coronoid tip proximal to the brachialis insertion (Figure 8-1C).14,33–35 The posterior aspect of the elbow can be exposed through a Kocher approach between the anconeus and the extensor carpi ulnaris (ECU). Proximally, the triceps is elevated from the distal humerus, and the posterior capsule can then be identified and released. Care is taken to preserve the lateral collateral ligamentous complex from its origin on the lateral epicondyle distally toward its insertion on the proximal ulna.14,33–35 The olecranon fossa can also be debrided and deepened if necessary. Ulnohumeral arthroplasty, if indicated, may also be performed and will be discussed later in this chapter. The tip of the olecranon is excised when osteophytes are present to prevent impingement in terminal extension. Distally, the radiocapitellar articulation can be addressed through the Kocher interval, and a radial head resection with or without arthroplasty may be performed if necessary when forearm rotation is compromised or if the radiocapitellar and/or proximal radioulnar articulation exhibits significant degenerative changes. Husband and Hastings36 reported good results at an average 38-month follow-up on seven patients with post-traumatic elbow contractures treated with open capsular release through an extensive lateral approach. They reported a decrease in the mean flexion contracture from 45 to 12 degrees and an increase in average maximal flexion from 116 to 129 degrees. They observed an increase in the average arc of motion of 46 degrees with no significant heterotopic ossification formation in any patient. In 1998, Cohen and Hastings37 reported results of 22 post-traumatic elbow contractures treated with open release through a less extensive ligament-sparing lateral approach, and noted significantly improved function and decreased pain at an average follow-up of 26 months. They reported an increase in the total flexion arc from 74 to 129 degrees and an increase from 135 to 159 degrees of forearm rotation. Mansat and Morrey33 reported equally successful increases in motion utilizing the lateral column approach for extrinsic elbow contractures. In their series of 38 patients, the authors noted a decrease in the mean flexion contracture from 52 to 24 degrees and improvement in maximal flexion from 101 to 121 degrees. There was an average total gain of 45 degrees in the arc of motion, which was preserved at an average follow-up of 43 months. There were, however, two patients (6%) with transient ulnar neuropathy, as well as four patients (11%) who actually had decreased range of motion at the time of final follow-up.
The Post-traumatic Stiff Elbow: Overview and Management
Incidence and Classification
Evaluation
Treatment
Nonoperative Treatment
Operative Treatment
Arthroscopic Capsular Release and Debridement
Extrinsic Contractures: Open Capsular Release and Debridement
Anterior Approach
Medial Approach
Lateral Approach
< div class='tao-gold-member'>
The Post-traumatic Stiff Elbow: Overview and Management
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree