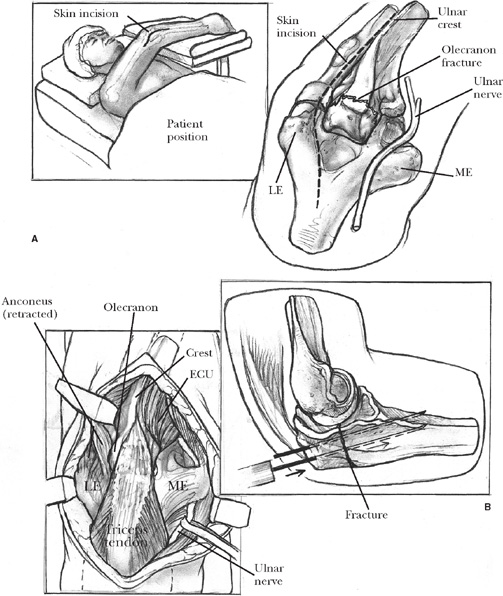
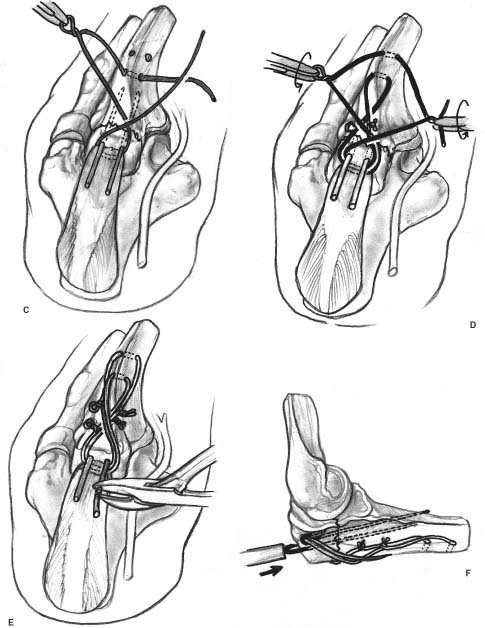
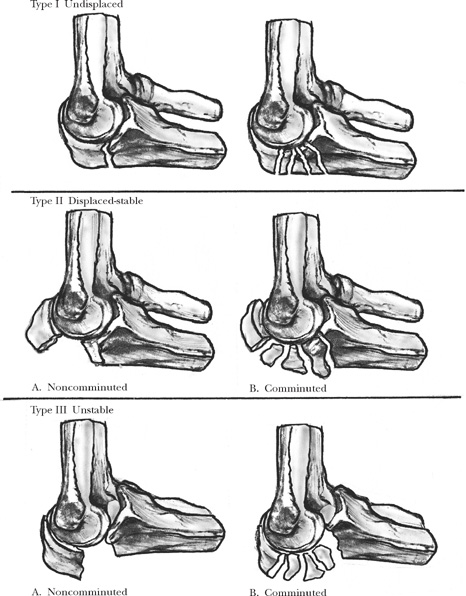
4 The olecranon process of the proximal ulna enhances the stability and strength of the elbow. Its subcutaneous position and attachment to the triceps make it susceptible to both direct and indirect injury. Although fractures of the olecranon are intra-articular, they have relatively low rates of post-traumatic arthritis, probably because most fractures occur at the relatively nonarticular transverse groove of the trochlear notch. The goals of treatment are restoration of the normal contour and dimensions of the trochlear notch to restore stability, healing of the fracture to restore triceps function, and early mobilization of the elbow to limit stiffness. Operative treatment is required for most fractures. The specific operative technique is tailored to the characteristics of the injury. Simple transverse fractures are treated with tension band wiring (with an interfragmentary screw added for oblique fractures), and comminuted fractures and fracture-dislocations are repaired with a plate and screws. The olecranon and coronoid processes of the proximal ulna form the trochlear notch that articulates with the trochlea of the humerus. The trochlear notch has olecranon and coronoid articular facets separated by the relatively nonarticular transverse groove of the trochlear notch.1 This is an area of relative narrowing of the olecranon process that, combined with diminished sub-chondral bone, may make it more susceptible to fracture. The trochlear notch prevents anteroposterior translation of the ulna on the humerus and also provides varus, valgus, and rotational stability to the elbow. It has been shown that the stability provided by the ulnohumeral articulation gradually decreases as the proximal ulna is incrementally resected.2,3 The triceps muscle tendon inserts on the dorsal surface of the olecranon, blending with the periosteum and the forearm fascia. The coronoid process is often fractured in association with a fracture-dislocation of the olecranon. Large coronoid fractures include the insertion of the anterior band of the medial collateral ligament. The brachialis inserts more distally on the ulna and usually remains functional even with a large coronoid fracture. Olecranon fractures may result from a fall from a standing height or a higher energy mechanism, such as a fall from a greater height or a motor vehicle collision. A direct blow to the olecranon with the elbow in 60 to 110 degrees of flexion produced olecranon fractures in the deepest part of the olecranon in a cadaver model.4 Indirect injuries such as avulsion fractures or posterior Monteggia-type fracture-dislocations also occur. A careful examination of the soft tissues and especially the ulnar nerve is carried out. Fracture-dislocations of the olecranon are often associated with small open wounds. Large wounds may occur with very high energy injuries. Immediate internal fixation is appropriate except in the unusual fracture with extreme contamination, extensive devitalized tissue, or a large soft tissue defect. FIGURE 4-1. The Mayo classification of olecranon fractures accounts for the important management issues, including displacement, comminution, and dislocation. Standard anteroposterior and lateral radiographs are usually sufficient to characterize the fracture. When the coronoid or radial head is fractured, computed tomography (CT), sometimes with three-dimensional reconstructions, will help depict the character of these associated injuries. Several classification systems have been described. Each has helped to emphasize certain injury characteristics and management issues. Colton et al5 proposed a classification system based on the displacement and character of the fracture. According to their system, type I fractures are nondisplaced and stable. Type II fractures are displaced and may be divided into subgroups based on the fracture pattern: Type IIA are avulsion fractures, Type IIB are transverse or oblique fractures, Type IIC are isolated comminuted fractures, and Type IID are fracture-dislocations.1 According to this system, a fracture is considered nondis-placed and stable if there are no more than 2 mm of displacement and no change in position of the fracture with gentle flexion and extension.5 Schatzker6 suggested classification of olecranon fractures into five types: type A, simple transverse fracture; type B, complex transverse fracture with articular impaction centrally; type C, simple oblique fracture; type D, comminuted fracture; and type E, oblique fracture distal to the midpoint of the trochlear notch.6 Impaction is less important at the olecranon than in other articular fractures and probably does not need to be distinguished from other forms of comminution. The Comprehensive Classification of Fractures7 groups olecranon fractures with those of the proximal radius and ulna. The fractures are divided into types, groups, and subgroups. Type A fractures are extra-articular, type B fractures have intra-articular involvement of one bone, and type C are intra-articular fractures of both bones. The fractures are further divided into groups and subgroups based primarily on the complexity of the fractures. Although inclusion of proximal ulna fractures along with proximal radius fractures is appealing for research purposes, in practice the characteristics important to treatment tend to get lost in the details. The Mayo classification system1 for olecranon fractures evaluates displacement, stability, and comminution (Figure 4-1). Type I is a stable, minimally displaced fracture (less than 2 mm of a gap between the fracture fragments), type II is a displaced fracture, and type III fractures are associated with instability of the ulnohumeral articulation. The fractures are further divided into subgroups A and B, according to the absence or presence of comminution, respectively. This classification accounts for most of the important issues and helps to guide treatment. Nondisplaced and minimally displaced fractures are treated nonoperatively. Standard treatment consists of 4 weeks of immobilization in a cast or splint, with the elbow at 90 degrees and the forearm in neutral rotation.1,5,8–10 Immobilization in extension is not necessary for these stable fractures. Four weeks after the fracture, immobilization is discontinued, and gentle active-assisted range of motion is initiated. Resistive exercises are delayed until healing is established on radiographs, usually about 8 weeks after the injury. Some authors suggest initiating active flexion with passive extension 2 weeks after the fracture.5 Displaced fractures are treated operatively.1,5,7,8,11,12 Displaced simple transverse fractures, the most common type of olecranon fracture,1,13,14 are treated with tension band wiring (Figure 4-2). Screw fixation alone does not provide rotational control, can distract the fracture, and does not always gain adequate hold of the distal fragment. Screw fixation combined with tension wire fixation has been described. Problems associated with migration or prominence of the implants can be limited by the use of specific operative techniques.15 The tension band principle converts the distractive force of the triceps into a compressive force across the fracture by applying fixation to resist distraction on the dorsal surface of the ulna.5 The tension band is provided by one or two stainless steel wires applied in a figure-of-eight fashion on the dorsal surface of the ulna. Two Kirschner wires drilled across the fracture provide additional translational and rotational stability. In oblique fractures, a lag screw can be placed across the fracture to provide stability through interfragmentary compression with tension band wiring used to protect or neutralize this screw.12 FIGURE 4-2. Noncomminuted, displaced fractures of the olecranon are treated with tension band wiring. (A). A lateral radiograph is obscured by the splint, but it shows a simple, transverse fracture of the olecranon. (B). The 0.045-inch Kirschner wires are drilled anteriorly so that they engage the anterior ulnar cortex distal to the coronoid to help limit the potential for wire migration. (C). Two 22-gauge Kirschner wires are passed through drill holes distal to the fracture, underneath the triceps insertion proximally, and over the dorsal ulna in a figure eight. (D). The wires are tensioned on both the radial and ulnar sides so that they are flush with the ulna and the slack is taken up. (E). The Kirschner wires are retracted a few millimeters, bent 180 degrees, and trimmed. (F). The bent ends are then impacted into the olecranon underneath the triceps insertion. Either general or regional anesthesia may be used. The patient can be positioned supine with the arm draped over the chest, in lateral decubitus with the arm supported by a bolster, or prone. Bone graft may be obtained from the iliac crest in all three positions, but it is rarely necessary. A sterile tourniquet may improve exposure and facilitate manipulation of the arm. Although some authors recommend curving the skin incision to avoid the tip of the olecranon, we prefer a straight dorsal incision and have encountered few problems with it. The ulnar nerve is mobilized only if needed for exposure, if the nerve is injured, or if associated soft tissue injury risks compression or kinking of the nerve. For simple, noncomminuted fractures, hematoma is removed from the fracture surfaces, and the periosteum is peeled back from the fracture edges to facilitate anatomic reduction. The reduced fracture can be stabilized with a large pointed reduction forceps. This may be facilitated by making a small drill hole in the distal fragment, allowing purchase of one tip of the pointed forceps. The other tip of the forceps grasps the tip of the olecranon and compresses the fracture. Two parallel 0.045-inch Kirschner wires are then drilled across the fracture site. The wires are directed slightly anterior to engage the anterior cortex of the distal fragment. A recent study suggested biome-chanical advantages of this wire orientation as compared with intramedullary placement of the wires.16 After drilling the wires through the anterior ulnar cortex, they are retracted a few millimeters in anticipation of later impaction of the proximal end into the olecranon. Two 2.5 mm transverse drill holes are placed through the apex of the diaphyseal ulna distal to the fracture site. A 22-gauge stainless steel wire is passed through each hole, placed in a figure-of-eight configuration over the dorsum of the fracture site, and passed anteriorly to the Kirschner wires—under the triceps insertion—using a 14-gauge needle. The wires are tensioned both medially and laterally until all slack is taken up in the wires and the twisted wire rests on the bone. The wires are trimmed, and the ends are bent into the soft tissues. The use of two 22-gauge wires rather than a single 18-gauge wire helps limit hardware prominence without compromising fixation strength. The proximal ends of the Kirschner wires are bent 180 degrees and impacted into the olecranon underneath the triceps insertion. This decreases the prominence of the wires and helps to limit the potential for wire migration. Displaced, comminuted fractures are treated with plate and screw fixation. Fragment excision and triceps advancement are mostly of historical interest, although they may still be useful for infirm older patients with very limited functional demands.1,7 Fragment excision is not appropriate for fracture-dislocations.5,15 Plate fixation allows maintenance of ulnar length in those fractures that would be shortened by tension band wiring. When fragment excision and triceps advancement are elected, Morrey7 recommends limiting the resection to no more than half of the olecranon to maintain stability; however, in older infirm patients, it may be reasonable to resect even more. It is important to attach the triceps as close as possible to the articular surface to provide a smooth transition between joint and tendon as it glides over the trochlea. Stout nonabsorbable sutures are placed in the triceps insertion from which the bone fragments have been excised. A tendon-grasping stitch such as a Krackow stitch is used. These sutures are passed through drill holes initiated directly adjacent to the articular surface and exiting onto the dorsal surface of the ulna, where they are tensioned and tied.7 For comminuted fractures, there is no need to elevate periosteum or muscle attachments. Instead, the normal contour and dimensions of the trochlear notch are restored, and the area of fragmentation is bridged with a plate and screws. For very unstable fractures it can be useful to temporarily stabilize the olecranon to the trochlea using a stout smooth Kirschner wire (usually 5/64 inch). A 3.5 mm limited contact dynamic compression plate (Synthes, Paoli, PA) contoured to wrap around the olecranon or a precontoured plate with 2.7 mm screws proximally (Accumed, Beaverton, OR) is well suited to the olecranon (Figure 4-3). Proximally the plate lies on the flat dorsal surface of the olecranon. Distally it lies directly over the apex of the olecranon. This is unsettling to some surgeons, but stable fixation can be achieved and very little muscle or periosteum need be elevated from the bone. The dorsal surface is the tension side of the olecranon and is the best surface for plating. Plates applied to the medial or lateral surface of the ulna are more likely to fail. The plate should extend well distal, particularly when comminution is extensive. There are few disadvantages to a long plate in this area. If the proximal olecranon is small or extensively fragmented, the fixation can be reinforced using a tension band wire passed through the triceps insertion.
Olecranon Fractures
Anatomy
Incidence and Mechanism of Injury
Assessment and Diagnosis on Presentation
Classification
Treatment
Nonoperative Treatment
Operative Treatment
Displaced Noncomminuted Fractures of the Olecranon
Operative Technique for Tension Band Wiring
Displaced, Comminuted Fractures of the Olecranon
Operative Technique for Excision of Fragments and Advancement of the Triceps
Operative Technique for Plate and Screw Fixation

Olecranon Fractures
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree