Type
Finding
Percent (%) [6]
I
Labral and biceps fraying, anchor intact
21
II
Labral fraying with detached biceps tendon anchor
55
III
Bucket-handle tear, intact biceps tendon anchor (biceps separates from bucket-handle tear)
9
IV
Bucket-handle tear with detached biceps tendon anchor (remains attached to bucket-handle tear)
10
V
SLAP lesion and anterior labral tear (Bankart lesion)
VI
Superior flap tear
VII
SLAP lesion with capsular injury
13.3 Clinical Presentation and Essential Physical Examination
A complete history and physical examination are critical to evaluating patients with suspected concomitant rotator cuff and SLAP pathology. These patients can typically be divided into two groups based on age: (1) younger patients with acute, traumatic etiologies and (2) older patients with chronic and/or acute-on-chronic presentations. At the initial evaluation, the mechanism of injury must be determined. Traumatic etiologies of RCT and/or SLAP lesions behave differently than insidious/atraumatic etiologies, and such differences may ultimately affect treatment strategies. Previous treatment, including both nonsurgical and/or surgical interventions, must be documented. Specifically, the patient must be asked if he/she experienced a traumatic dislocation versus a subluxation event. It is important to ascertain the position of the arm at the time of injury as well as the current and desired activity level of the patient. Treatment decisions are often made, regardless of the extent of the pathology, based on the desired activity level of the patient. It is imperative to differentiate between treatment options for high-level athletes/throwers versus weekend warriors and older, more sedentary patients, looking to improve their functionality with recreational sports and activities of daily living, respectively.
While certain features of the patient history may be suggestive of rotator cuff and/or SLAP lesions, patients may present with multiple coexisting pathologies. It is crucial to determine which is symptomatic and which is simply incidental or age appropriate. Perhaps some of the most difficult patients to evaluate are those with primary multidirectional instability (MDI). These patients will often complain of generalized, or deep, posterior shoulder pain, often accompanied with decreased athletic performance (often tennis, swimming, football linemen, etc), and loss of strength [24–26]. Similar complaints may be found in patients with chronic RCT/SLAP pathology, making evaluation of these patients challenging. The clinician must make every attempt to distinguish between such pathologies, as the treatments are vastly different. Patients with generalized ligamentous laxity and/or a history of multiple other joint subluxation events may lead more toward a diagnosis of MDI.
Patients with combined RCT/SLAP pathology may describe sharp shoulder pain resulting from an initial traumatic event, but more often these patients will complain of pain diffusely throughout the shoulder, and especially with overhead activities. Patients whose symptoms are predominately RCT related may complain more of night pain and difficulty with overhead activities of daily living, while patients with predominantly SLAP-related complaints may complain more of symptoms during attempted overhead throwing or with repetitive activities requiring shoulder overhead motions.
On physical examination, the appearance, neurologic status, and stability of both shoulders should be carefully evaluated. Care should be taken to document atrophy, asymmetry, abnormal motion, muscle spasm, swelling, scapular winging, and abnormal glenohumeral tracking. The asymptomatic shoulder may be examined first to gain patient confidence and relaxation [27–29]. Scapulothoracic dyskinesis should be carefully evaluated and documented if present [30–32]. Any loss of motion, even subtle, should be documented, and every attempt should be made to improve motion with therapy preoperatively in order to avoid progressive loss of motion. Special tests for suspected SLAP pathology should then be performed, including O’Briens active compression test and dynamic labral shear (O’Driscoll’s) test. The active compression test is performed with the shoulder in 90° of flexion and 30° of horizontal adduction. Downward pressure is placed onto the arm, and the patient is asked to resist the pressure both with the arm in maximum external (thumbs up) and internal (thumbs down) rotation. Labrum pathology should be suspected if the patient has pain during the internal rotation portion of the test that is decreased when the shoulder is placed into external rotation (Fig. 13.1a, b). The dynamic labral shear test is performed with the arm at the side and the elbow flexed to 90°. The shoulder is then externally rotated and abducted to 90°, followed by further abduction of the arm to 120° (with the elbow flexed). The test is considered positive for labrum pathology if pain is reproduced during the abduction from 90° to 120° (Fig. 13.2a, b). The test is considered equivocal if the patient has pain both within and outside this range.
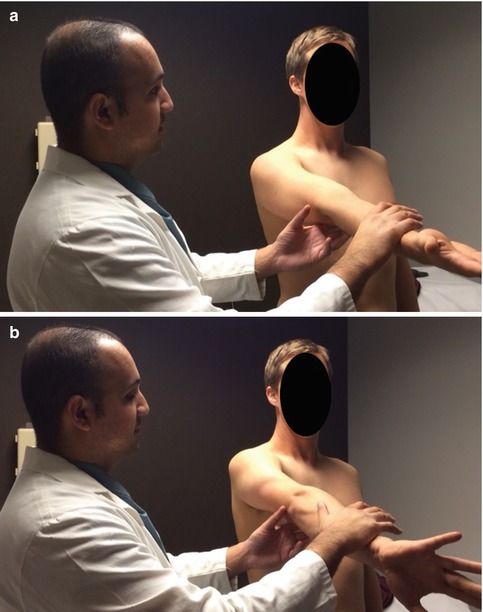
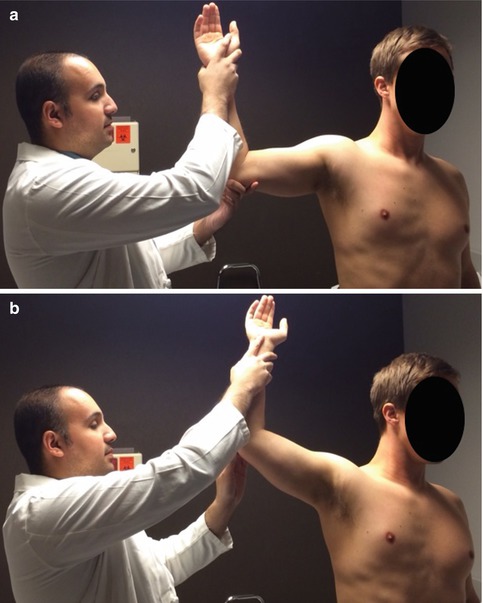
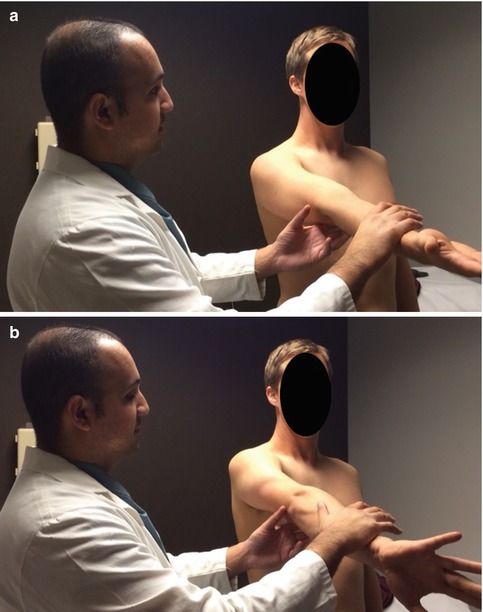
Fig. 13.1
(a, b) O’Brien’s test for SLAP pathology is positive when the patient has increased pain with resisted forward elevation when the shoulder is in the adducted and internally rotated position
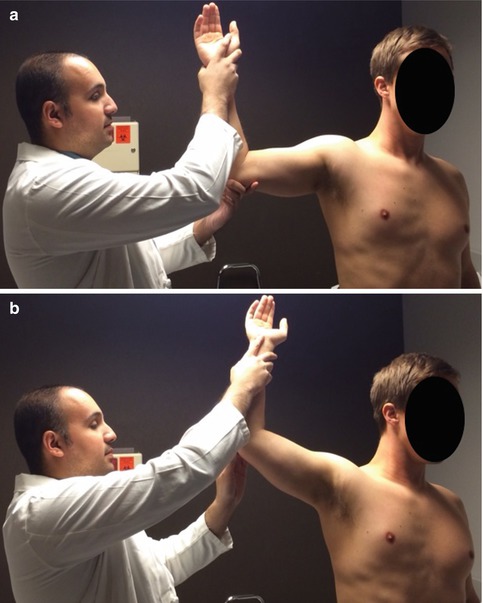
Fig. 13.2
(a, b) O’Driscoll’s dynamic labral shear test is positive for SLAP pathology when the patient’s pain is recreated with abduction of the arm from 90° to 120°
Intraoperatively, examination with the patient under anesthesia includes evaluation of anterior and posterior glenohumeral translation, as well as the degree of inferior capsular laxity. Anteroposterior glenohumeral translation is graded as follows: grade I, humeral head translation up to but not over the glenoid rim; grade II, humeral head translation over the rim of the glenoid that spontaneously reduces; and grade III, dislocation of the glenohumeral joint. As described by Altchek and colleagues, the sulcus sign was graded as follows: grade 0, no inferior translation; grade I, inferior humeral head translation of up to 1 cm; grade II, inferior translation of 1–2 cm; and grade III, inferior translation of >2 cm [24]. The Gagey hyperabduction test is also performed to assess laxity of the inferior glenohumeral ligament. While stabilizing the scapulothoracic joint and passively abducting the arm (via the glenohumeral joint alone,), a 15° increase versus the contralateral side is suggestive of inferior capsular laxity (i.e. 105° vs. 90°) (Fig. 13.3a, b) [33].
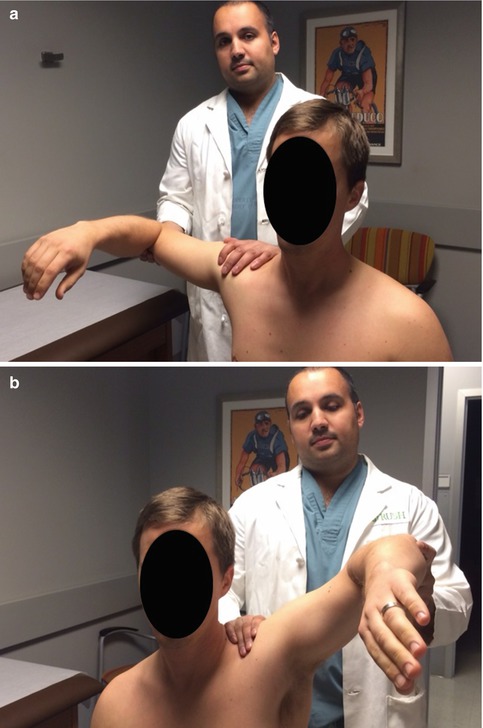
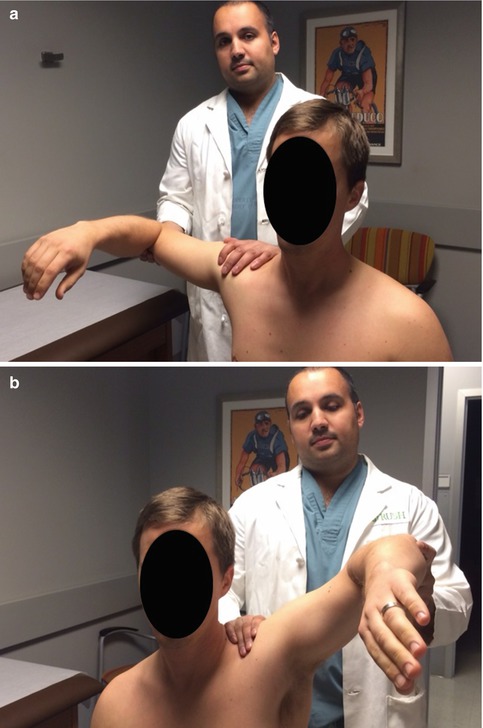
Fig. 13.3
(a, b) The Gagey hyperabduction test is suggestive of instability (more specifically IGHL laxity) if the involved shoulder demonstrates an increase of 15° of passive abduction relative to the contralateral
13.4 Essential Radiology
For initial evaluation of the shoulder, standard radiographs are obtained. In addition to the standard anterior-posterior (AP), scapular-Y, and axillary views, a shoulder instability series may also include a Grashey view, West Point axillary view, Stryker notch view, Garth view, or Bernageau view. The Grashey view aligns the glenoid such that it is perpendicular to the plane of the x-ray allowing for evaluation of the glenohumeral joint space. The West Point axillary view is a tangential view of the anteroinferior rim of the glenoid. The Stryker notch view is particularly useful in evaluating for the presence of a Hill-Sachs lesion. The Garth view, also known as the apical oblique view, is also used in patients with shoulder instability. Of note, the axillary view is often the best true lateral view of the shoulder. It allows for evaluation of anterior and posterior instability, glenoid fractures, and humeral head compression fractures. Note the Bernageau view (Fig. 13.4) is an accurate and reproducible technique for measuring the presence of glenoid erosion, with similar results when compared to the 3D CT scan [34].


Fig. 13.4
The Bernageau glenoid profile view (normal in this example) is the most sensitive plain radiographic view for detecting the presence of a glenoid rim lesion
Magnetic resonance imaging (MRI) is useful in evaluating the rotator cuff, labrum, glenohumeral ligaments, cartilage, and capsule. This modality provides superior detail of soft-tissue pathology, while also detailing the bone marrow and articular cartilage integrity. MRI with the administration of intra-articular gadolinium (MRI-arthrogram, or MRA) results in improved sensitivity for detecting subtle pathology. Of note, indirect MRI-arthrogram is less invasive and better tolerated than the direct arthrogram. In this situation, intravenous gadopentetate dimeglumine is administered, resulting in homogeneous enhancement and improved delineation of soft-tissue structures. This modality is valuable in identifying inflammatory conditions and is indicated in diagnosing chronic Bankart lesions and their variants and SLAP lesions and in postoperative evaluation of the painful shoulder. Nevertheless, direct MRI-arthrogram is the diagnostic tool of choice for evaluation of the rotator cuff and labrum in young athletes. Direct MRI-arthrogram is indicated in rotator interval lesions, SLAP tears, anterior labrum periosteal sleeve avulsion (ALPSA) lesions, Bankart lesions, and its variants [9]. The utility of MRI without arthrography has been questioned by a recent study where a high level of sensitivity and low level of specificity was found with respect to diagnosis of SLAP lesions [35]. The investigation of choice is MRI-arthrogram with accuracies reported between ~75–90 %. Distinguishing between subtypes, however, can be difficult [36]. The characteristic finding is high signal (fluid on T2WI or contrast on T1WI) extending into the superior labrum and tracking into the labrum and sometimes into the biceps tendon (Fig. 13.5).
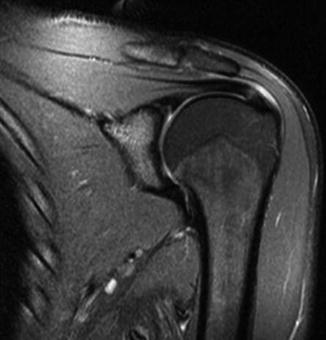
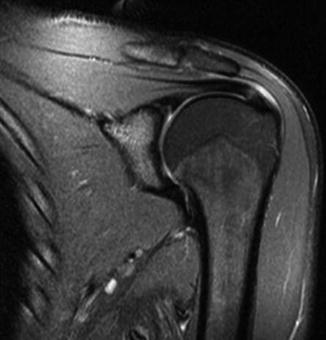
Fig. 13.5
Coronal T2-weighted MRI slice demonstrating a superior labral tear (evidenced by fluid tracking between the glenoid and superior labrum)
CT is also indicated in evaluating more chronic pathology in addition to grading the degree of muscle atrophy or fatty infiltration in the setting of concomitant rotator cuff pathology [9]. Patients with a history of previous instability surgery and patients with a midrange-of-motion instability should undergo CT scan to evaluate for anterior or posterior glenoid insufficiency, engaging Hill-Sachs or reverse Hill-Sachs lesions (Fig. 13.6). Intra-articular contrast may be of benefit in future defining bony anatomy in chronic cases.
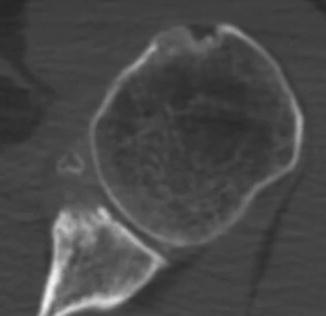
Fig. 13.6
Axial CT image demonstrating anterior glenoid bone loss in the setting of recurrent instability
Finally, ultrasound has become an important diagnostic tool in the evaluation of shoulder complaints, especially for tendon pathology of the shoulder. In experienced hands, this modality is cost-effective and portable and has a high rate of acceptance from patients. In patients for whom MRI is not an option, ultrasound is the diagnostic tool of choice when evaluating the rotator cuff [9]. It also has been shown to have satisfactory sensitivities and specificities in the assessment of postoperative rotator cuffs. Ultrasound is also useful in imaging-guided shoulder interventions, such as the aspiration and injection of paralabral cysts [10–14].
13.5 Arthroscopic Pathology
While MRI is helpful in identifying lesions in the superior labrum, differentiating SLAP tears from normal anatomy is challenging because of the variable insertional anatomy of the anterosuperior labrum and the biceps anchor-labral complex. Therefore, arthroscopy remains the gold standard for diagnosing and classifying the lesion. During diagnostic arthroscopy, care should be taken to differentiate pathology from anatomical variants, i.e., sublabral foramen (Fig. 13.7) or a Buford complex. The shoulder should also be placed in abduction and external rotation to assess for the presence of a “peel-back” sign, which verifies the presence of instability (Fig. 13.8). The biceps-labral complex lesion is closely inspected and probed as its classification will direct the surgical strategy. Finally, the biceps tendon should be pulled into the joint with downward traction, with a blunt probe, to examine for fraying or tenosynovial inflammation of the tissue within the bicipital groove.
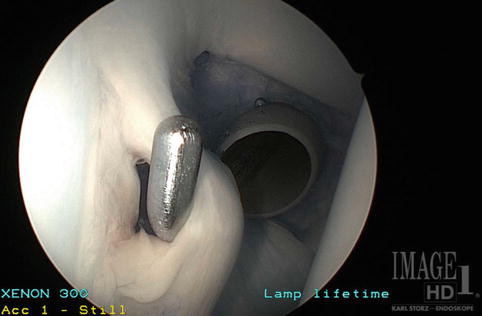
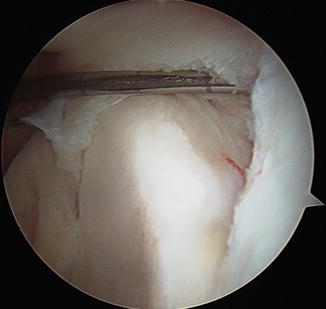
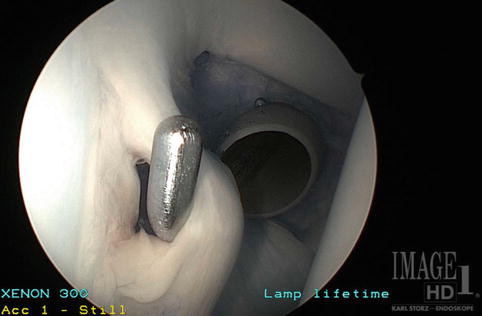
Fig. 13.7
Arthroscopic image of a sublabral foramen
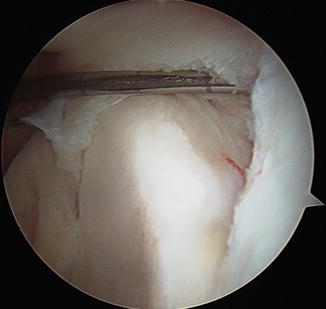
Fig. 13.8
Arthroscopic image demonstrating the peel-back sign
13.6 Treatment Options
The optimal management of patients with concurrent SLAP and rotator cuff lesions remains controversial. At a minimum, nearly all patients should undergo 3 months of conservative management before surgical intervention is even considered. Nonsurgical treatment begins with rest, activity modification, and oral anti-inflammatories. Patients should also be enrolled in physical therapy to focus on biceps stretching, strengthening of the rotator cuff, and ameliorating any scapulothoracic dyskinesis. In patients with persistence of pain or functional limitation after a trial of conservative treatment, shoulder arthroscopy is often warranted. In patients with combined lesions, surgical management of the rotator cuff is identical to that employed in patients with isolated rotator cuff pathology. Generally, partial-thickness tears <50 % width are debrided and partial-thickness tears greater than 50 % width and full-thickness tears are repaired [37]. Symptomatic bursal-sided tears greater than 3 mm in thickness are generally repaired. Similarly, type I, III, and IV SLAP lesions are also managed as they would be if they were stand-alone lesions. The principal dilemma when treating concomitant rotator cuff and SLAP lesions involves management of patients with type II SLAP lesions. While surgeons broadly agree that surgical repair renders superior outcomes for isolated type II SLAP lesions, there is reluctance among many surgeons to perform concurrent rotator cuff and SLAP repair due to concern over prolonged postoperative immobilization, stiffness, and poor clinical outcomes. Therefore, some surgeons advocate biceps-labral complex debridement, others advocate biceps anchor tenotomy or tenodesis, and others still advocate surgical repair of the biceps-labral complex.
Abbot and colleagues randomized 48 patients older than 45 years of age with rotator cuff tear and concomitant type II SLAP lesion to receive either SLAP repair or labral debridement in addition to rotator cuff repair [38]. They demonstrated that at 2-year follow-up, the debridement cohort had significantly better UCLA scores (34 vs. 31), function (5.5 vs. 3.8), and pain relief than the SLAP repair cohort. The authors therefore concluded that rotator cuff repair with SLAP debridement may optimize patient satisfaction and functional outcome in patients over 45 years of age with a minimally retracted rotator cuff tear and associated SLAP lesion.
Franceschi and colleagues randomized 63 patients older than 50 years of age with concurrent lesions undergoing rotator cuff repair to receive either SLAP repair or biceps tenotomy [39]. At minimum 2.9-year follow-up, the tenotomy cohort experienced significantly better UCLA scores, range of motion, and patient satisfaction. Similarly, Kim and colleagues evaluated 42 patients who underwent arthroscopic rotator cuff repair and either SLAP repair or biceps tenotomy for large to massive rotator cuff tears and concomitant type II SLAP lesions, respectively [40]. At minimum 2-year follow-up, patients who underwent biceps tenotomy demonstrated significantly better pain relief, range of motion, simple shoulder test, ASES, and UCLA scores.
In spite of the results of the aforementioned comparative trials, a number of authors support management of the patient type II SLAP lesions and concurrent rotator cuff tear with combined SLAP and rotator cuff repair. As discussed earlier, Morgan and colleagues have theorized that patients with concurrent lesions initially develop a SLAP lesion, which promotes posterosuperior instability that ultimately may contribute to rotator cuff damage. For this reason, they recommend surgical repair of type II SLAP lesions to remove the pathological entity that precipitated (or aggravated) the rotator cuff tear in the first place [16]. Levy and colleagues evaluated patients younger than 50 years (mean 33) and compared results of those who underwent isolated repair of a type II SLAP lesion with those who underwent repair of a type II SLAP lesion and either rotator cuff repair or debridement [41]. They found that both groups had equivalent outcomes with regard to UCLA shoulder score and, therefore, concluded that management of a rotator cuff lesion did not have a negative effect on results of patients undergoing repair of a type II SLAP lesion. Forsythe and colleagues retrospectively compared 34 patients who underwent concomitant rotator cuff and SLAP repair with a control group of 28 patients who underwent isolated rotator cuff repair [20]. Although patients with concurrent lesions had significantly worse preoperative ASES scores (22.6 vs. 34.3), postoperatively there was no significant difference between groups with regard to range of motion or ASES score. Therefore, the authors conclude that simultaneous SLAP repair and rotator cuff repair provides results comparable to isolated rotator cuff repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








