46 Shoulder Pain
Determining the source of shoulder pain is essential in recommending the proper method of treatment. The examining physician must be able to differentiate the occurrence of shoulder pain caused by intrinsic, or local factors, and extrinsic, or remote factors, or a combination of the two. Intrinsic factors originate from the shoulder girdle and include glenohumeral and periarticular disorders, whereas extrinsic factors occur outside of the shoulder girdle with secondary referral of pain to the shoulder (Table 46-1). Examples of extrinsic factors include left shoulder pain as the initial presentation of coronary artery disease; hepatic, gallbladder, and splenic disease also may initially manifest as shoulder pain.
Table 46-1 Common Causes of Shoulder Pain
| Intrinsic Causes |
| Periarticular Disorders |
| Glenohumeral Disorders |
| Extrinsic Causes |
| Regional Disorders |
Anatomy and Function
Because of its complexity, an understanding of the structural and functional anatomy of the shoulder is required for the clinician who is treating shoulder pain. The shoulder joint is the most mobile joint of the body, although mobility is gained at the sacrifice of stability. Only 25% of the humeral head surface has contact with the glenoid at any time. The labrum increases the contact area of the articular surface and confers stability to the joint.6 Lesions of the labrum may result from instability, and the type of lesion may indicate the type of instability. Labral tears also may be a source of pain from internal derangement of the shoulder.7 Joint stability is provided by a thin capsule and by the glenohumeral ligaments, which are thickenings of the capsule anteriorly, posteriorly, and inferiorly.6 Anterior stability is predominantly conferred by the anterior band of the inferior glenohumeral ligament.
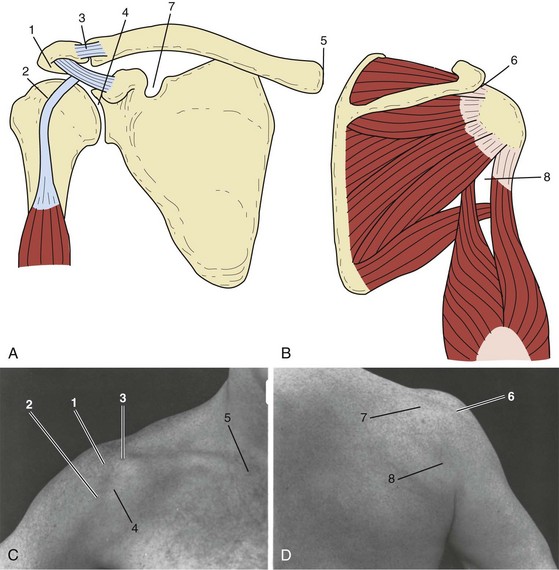
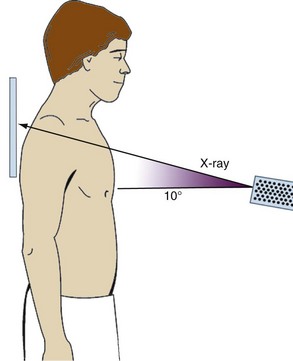
Figure 46-1 shows the musculoskeletal and topographic localization of pain associated with common shoulder disorders. Figure 46-2 shows the relationship of the three posterior rotator cuff muscles coursing anteriorly underneath the acromion to insert on the greater tuberosity. The subscapularis, the only anterior rotator cuff muscle, inserts on the lesser tuberosity. By understanding the relationship between the rotator cuff and the subacromial region, bounded inferiorly by the humeral head and superiorly by the undersurface of the acromion, the clinician can visualize the problems of impingement syndrome and can accurately inject this space. Knowledge of the route of the tendon of the long head of the biceps through the bicipital groove and onto the superior aspect of the glenoid helps in understanding bicipital tendinitis. Before attempting to diagnose and treat shoulder pain, the clinician should review in detail one of the many sources describing the structural and functional relationships of the shoulder girdle.2,3
Diagnosis
Physical Examination
Proper physical examination of the shoulder includes close inspection of the shoulder girdle from the front and back. The evaluation is started by standing behind the patient, who has both shoulders exposed. The normal shoulder is always inspected and compared with the injured shoulder. Examination can be performed with the patient in the sitting or standing position. Contour and symmetry are observed and compared between shoulders, and any atrophy or asymmetry in shoulder position or level is assessed. Spinatus muscle atrophy may result from disuse, chronic cuff tear, or suprascapular or brachial neuropathy.8 If scapular winging is evident, the patient should be asked to do a wall push-up, which accentuates winging.
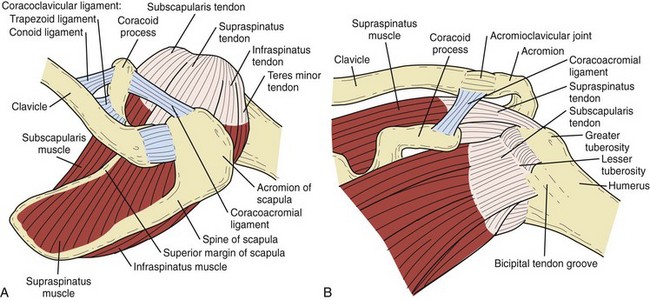
Range of motion should be carefully recorded, along with notation of any absence of rhythmic shoulder motion or excessive scapulothoracic motion that may compensate for the lack of glenohumeral motion. Internal rotation of the shoulder is checked by having the patient reach behind the back with the thumb while the examiner notices the vertebral level. Loss of internal rotation is seen early with shoulder pain and usually indicates some tightness of the posterior shoulder capsule. The biceps tendon; the coracoid, lesser, and greater tuberosities; and the posterior cuff are palpated, and any tenderness is gauged (Figure 46-3A). Tenderness on palpation of the long head of the biceps frequently is associated with rotator cuff tendinopathy and tenderness of the greater tuberosity. Any spasm or tenderness of the trapezius or levator scapulae may be associated with rotator cuff disease or cervical spine disease. Cervical range of motion and palpation of the paracervical muscles are carried out. Paracervical tenderness and limited range of motion of the neck may indicate cervical spondylosis or neurogenic disease. A Spurling test is done by flexing the neck laterally while applying axial compression to the skull. Pain that radiates to the ipsilateral shoulder is considered a positive test result and indicates radiculopathy.
To elicit the impingement sign, the shoulder is elevated passively in forward flexion, while the scapula is depressed with the opposite hand, forcing the greater tuberosity against the anterior acromion and producing pain in cases of impingement (Figure 46-3B).9 This maneuver also may be painful in conditions such as adhesive capsulitis, glenohumeral and acromioclavicular (AC) arthritis, glenohumeral instability, and calcific tendinitis. A dynamic impingement test, the circumduction-adduction shoulder maneuver, also called the Clancy test, is 95% sensitive and 95% specific for diagnosing rotator cuff tendinopathy, including partial tears.10 The test is done with the patient in the standing position and with the head turned to the contralateral shoulder. The affected shoulder is circumducted and adducted across the body to shoulder level, while the elbow is kept in extension, the shoulder in internal rotation, and the thumb pointing toward the floor (Figure 46-3C). In this position, the patient is instructed to resist maximally as a uniform downward force is applied to the extended arm by the examiner. The test result is considered positive if pain or weakness is elicited during the maneuver, with pain localized to the anterolateral aspect of the shoulder. A strong positive correlation of pain and weakness is noted with complete cuff tear.10
The sternoclavicular and AC joints should be observed for prominences and palpated for stability and tenderness. Many patients with impingement have tenderness on direct downward palpation of the AC joint owing to impingement on the cuff from undersurface osteophytes of the distal clavicle.2,8
AC joint tenderness may also result from primary AC joint arthrosis and should be differentiated by physical examination, including the cross-chest adduction test and O’Brien’s test.11 Radiographic evidence of AC joint arthrosis is common in patients older than 40 years, but this condition is not usually painful.12
The cross-chest adduction test or the horizontal adduction test is performed by forward flexing the shoulder 90 degrees with subsequent cross-chest adduction of the arm (Figure 46-3D). Pain localized to the AC joint is considered a positive test result. If pain occurs posteriorly over the shoulder, a tight posterior capsule with impingement is suspected. O’Brien’s test is performed by forward flexing the arm 90 degrees and adducting the arm 10 degrees out of the sagittal plane of the body. The first part of the test is performed with the hand maximally pronated with the thumb pointed down. In this position, the patient is asked to resist as the examiner applies a downward force on the arm. If the test elicits pain, the patient is asked if the pain is on top of the shoulder or deep inside. Pain localized to the top of the shoulder indicates AC joint pain, and pain deep inside the shoulder indicates a superior labrum anterior posterior (SLAP) lesion. In the second part of the test, the patient is asked to supinate the hand maximally, while the examiner applies a downward force to the arm. If the patient notices significantly less pain, the test result is positive for a SLAP lesion. If the pain is unchanged and is located on top of the shoulder, the test result is positive for AC joint pathology.11
If the cause of AC joint tenderness is still in question, a lidocaine injection should be administered. The clinician should carefully avoid injecting the subacromial space by advancing the needle too far inferiorly through the AC joint; this can lead to false interpretation. Painful degenerative changes of the AC joint may exist concomitantly with subacromial impingement and should be evaluated thoroughly when surgical treatment (i.e., distal clavicle excision) is being considered.13
In patients with pain out of proportion to objective findings, other causes of shoulder pain should be sought, including calcific tendinitis, infection, reflex sympathetic dystrophy, and fracture. Patients with significant wasting of the supraspinatus and infraspinatus muscles and posterior shoulder pain, especially younger patients, may have suprascapular neuropathy or brachial neuropathy (Parsonage-Turner syndrome).8,14
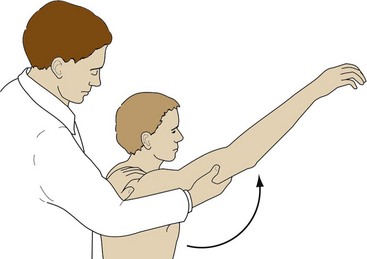
Patients with chronic cuff disease frequently have variable disuse atrophy of the supraspinatus and infraspinatus fossae; in cases of chronic massive cuff tears, atrophy and weakness can be severe. Strength testing of external rotation should be done with the elbow at the side and supported by the examiner; the patient is asked to attempt external rotation of the shoulder from a neutral position (0 degrees of adduction), while the examiner applies resistance (Figure 46-3E).15 Weakness in this position may suggest a tear of the infraspinatus tendon. Abduction strength testing against resistance is done with the shoulder in 30 degrees of forward flexion and 90 degrees of abduction, and with the thumb pointed toward the floor (Figure 46-3F).16,17 Weakness in this position may suggest a tear of the supraspinatus tendon. A lift-off test should be performed with the shoulder in internal rotation; the patient is asked to try to hold the hand away from the back. Inability to do so indicates a subscapularis tear.
If after a thorough physical examination impingement is suspected, an impingement test should be performed with injection of 5 mL of local anesthetic into the subacromial space.18,19 Before the test is performed, the patient is asked to grade the pain during the impingement signs on a visual analog scale of 0 to 10, with 0 equal to no pain and 10 equal to the most severe pain the patient has ever experienced. The injection may be done anteriorly, laterally, or posteriorly, depending on the physician’s preference. Ten minutes after injection of local anesthetic into the subacromial space, the patient should be re-examined and asked to regrade the pain on the same visual analog scale. A 50% or greater reduction in pain is thought to be a positive test result for impingement; otherwise, an alternative cause of shoulder pain should be sought, or inadequate placement of the anesthetic should be suspected. If the AC joint is thought to be contributing to the shoulder pain, 1 to 2 mL of local anesthetic should be injected into the joint, and the shoulder should be re-examined. When subacromial impingement and the AC joint are thought to be contributing to shoulder pain, serial injections during separate office visits may be needed to evaluate the shoulder while minimizing discomfort to the patient.12
Imaging
Radiographic Assessment
For nontraumatic painful shoulder evaluation, standard radiographic profiles are used. An impingement series should be obtained, which includes anteroposterior views with a 30-degree caudal tilt (Rockwood view), an outlet view (scapular Y with 10- to 15-degree caudal tilt), and an axillary view. Internal and external rotational views may be obtained if calcific tendinitis or instability is suspected. The Rockwood view can reveal any osteophytes off the anterior acromion and AC joint.20 In cases of traumatic injury, a trauma series is obtained that includes a true anteroposterior view, a scapular Y view, and an axillary view. The axillary view is useful in assessing posterior or anterior subluxation of the humeral head. Additional views, such as the West Point view, which evaluates the glenoid for evidence of a bony Bankart lesion, or the Styker notch view, which assesses the humeral head for a Hill-Sachs lesion, may be obtained to assist evaluation if the diagnosis of instability is in doubt. Secondary impingement-type rotator cuff tendinitis may be caused by increased anterior translation with subluxation of the humeral head. In such cases, an axillary view or fluoroscopy can help show the subluxation.21,22
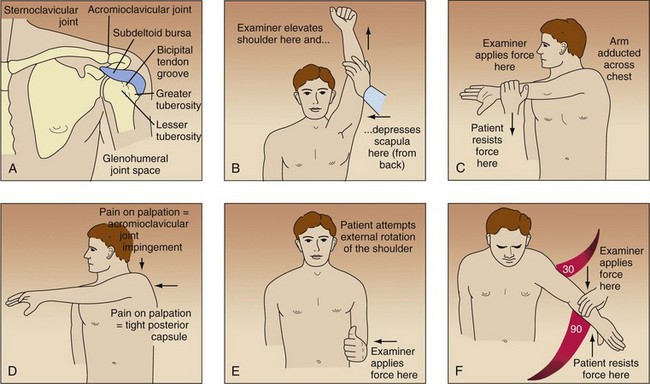
When AC joint pathology is suspected, a 10-degree, cephalic tilt view of the AC joint at 50% penetrance, as described by Zanca,23 should be obtained (Figure 46-4). Stress views of the AC joint may be obtained by strapping 5 to 10 lb of weight to the patient’s forearms and determining AC separation. Comparing the coracoclavicular distance of both shoulders may be helpful. When clinically indicated, cervical spine radiographs should be obtained to exclude cervical spondylosis as a cause of shoulder pain.
Arthrography
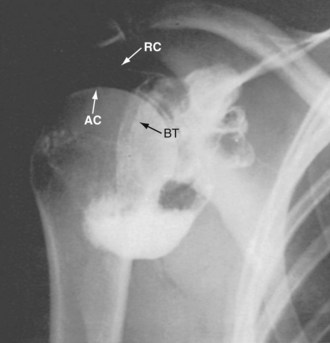
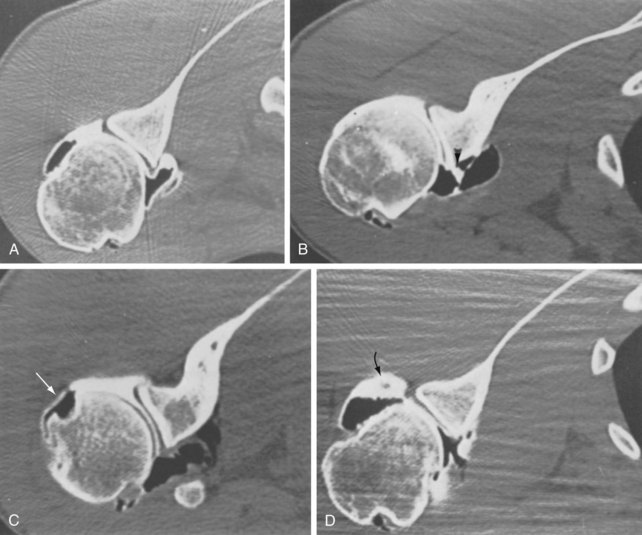
Double-contrast arthrotomography (DCAT) can be used to evaluate problems of the rotator cuff, glenoid labrum, biceps tendon, and shoulder capsule.24–27 Figure 46-5 shows normal DCAT of the shoulder. Rotator cuff tears can be shown by single-contrast or double-contrast studies. Proponents of double-contrast arthrography believe that the extent of the tear, the preferred surgical approach, and the quality of the rotator cuff tissue are best determined by double-contrast studies.24–29 Arthrography without MRI or CT can be misleading and may result in underestimation of the extent of a rotator cuff tear. Multidetector CT can enhance the accuracy of diagnosing labral and rotator cuff tears, especially in patients for whom MRI is not possible (Figure 46-6).
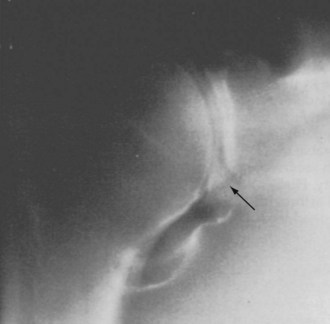
Tears of the glenoid labrum without shoulder dislocation are sources of anterior shoulder pain in athletes.7 Glenoid labrum tears (Figure 46-7), with or without associated glenohumeral subluxation, frequently can be identified by DCAT.27,28 Kneisl and colleagues30 described 55 patients who underwent DCAT followed by diagnostic shoulder arthroscopy. DCAT predicted the arthroscopic findings in 76% of anterior labrum studies and 96% of posterior labrum studies. This test was 100% sensitive and 94% specific in diagnosing complete rotator cuff tears. Partial rotator cuff tears identified at arthroscopy were missed in 83% of patients undergoing DCAT. Investigators believed that DCAT was better in diagnosing intra-articular and cuff pathology in cases of instability than when pain alone was the presenting diagnosis.30
Shoulder arthrography can confirm a diagnosis of adhesive capsulitis by showing a contracted capsule with an obliterated axillary recess (Figure 46-8). The use of subacromial bursography has been beneficial in visualizing the outer surface of the rotator cuff and the subacromial space in cases of impingement.31,32 Fukuda and associates33 reported a small series of younger patients (average age, 41.8 years) who underwent subacromial bursography after a negative glenohumeral arthrographic result. These patients showed pooling of contrast medium on the bursal side of a tear, which was confirmed at the time of surgery. Subacromial bursography is not routinely used diagnostically, and, in our opinion, it is of little value in planning surgical procedures.
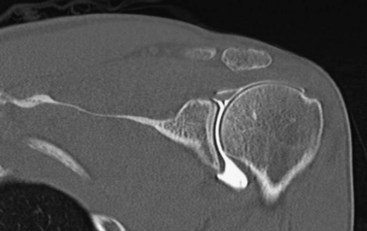
Computed Tomography
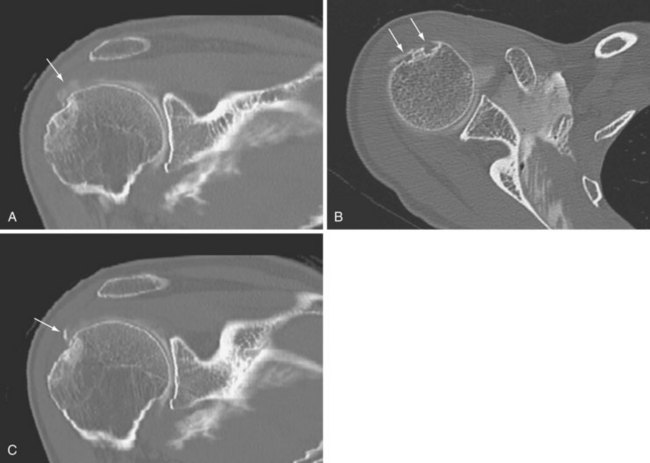
CT is helpful in evaluating the musculoskeletal system, and CT combined with contrast arthrography (CT-arthrography) has become a major diagnostic tool for the evaluation of glenoid labrum tears, loose bodies, and chondral lesions (Figure 46-9). Rafii and co-workers34 reported using CT-arthrography in an evaluation of shoulder derangement. This study found 95% accuracy of CT-arthrography for investigating lesions of the labrum and articular surface.34 More recently, multidetector CT-arthrography scans have been used to evaluate partial cuff tears (Figure 46-10A), cystic lesions (Figure 46-10B), and calcific tendinopathy (Figure 46-10C).
Ultrasonography
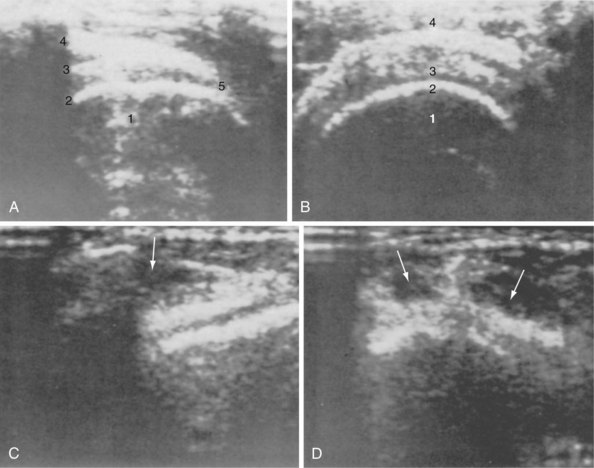
Technologic improvements in ultrasound equipment have led to improved ultrasound study of the rotor cuff. The technique is noninvasive, is rapid, and involves no radiation exposure.30–3235 The cuff is examined in the horizontal and transverse planes with the arm in different positions to allow visualization of various areas of the cuff. These techniques generally provide visualization of the distal cuff, where most rotator cuff tears are located. Figure 46-11 shows normal and abnormal ultrasound images of the rotator cuff in longitudinal and transverse planes.
Several studies report high sensitivity and specificity for the diagnosis of a rotator cuff tear by ultrasound.32–35 The specificity and sensitivity of the procedure are reported to be greater than 90% as determined by arthrographic and surgical correlations.34,35 This technique also has been used for the postoperative evaluation of a rotator cuff repair and for evaluation of abnormalities of the biceps tendon.36–40
Gardelin and Perin41 reported ultrasound to be 96% sensitive in determining rotator cuff and biceps tendon pathology. Mack and associates36 found ultrasound to be valuable in evaluating postoperative patients with recurrent shoulder symptoms. In a prospective study, Hodler and colleagues39 compared ultrasound with MRI and arthrography in evaluating rotator cuff lesions in 24 shoulders. Ultrasound identified 14 of 15 torn cuffs, MRI identified 10 of 15, and arthrography identified 15 of 15.39 Ultrasound identified 7 of 9 intact rotator cuffs, whereas MRI was accurate in 8 of 9 intact cuffs.39 Vestring and colleagues42 found ultrasound to be as accurate as MRI in the diagnosis of humeral head defects and joint effusions, but inferior to MRI in the diagnosis of labrum lesions, rotator cuff lesions, subacromial spurs, and synovial inflammatory disease. In the hands of an experienced sonographer, ultrasound may be the most cost-effective test for the initial evaluation of a rotator cuff injury, but most surgeons require CT-arthrography or MRI confirmation before beginning surgical exploration.36,39,41–43
Arthroscopy
The use of arthroscopy for the diagnosis of shoulder pathology increased in the 1980s, in part because of its accuracy, which was far greater than that of clinical examination and better than the accuracy of other diagnostic modalities of the time. With technologic advances in fiberoptics, video output, and arthroscopic instrumentation, the use of arthroscopy to diagnose and treat shoulder problems exponentially increased to include procedures previously used only for open techniques.44
Compared with DCAT, arthroscopy is more accurate in the diagnosis of intra-articular lesions associated with a painful shoulder.30 An additional benefit is that arthroscopy can be used to diagnose and treat shoulder problems of the glenohumeral joint and the subacromial region. With increased accuracy of MRI-arthrography in detecting partial cuff tears and labral lesions, diagnostic shoulder arthroscopy has become less common in the absence of clear indications and specific treatment plans. In combination with a detailed history and physical examination, and along with examination under anesthesia, shoulder arthroscopy has been helpful in the diagnosis of chronic instability patterns of the glenohumeral joint.44–47
The indications and usefulness of shoulder arthroscopy in the treatment of common pathologic conditions have continued to increase as the technology improves, and as understanding of the pathophysiology of shoulder problems grows. Shoulder arthroscopy has been used routinely to confirm and treat SLAP lesions, labral tears, partial cuff tears, refractory adhesive capsulitis, partial biceps tendon tears, and multidirectional instability. Other conditions that are routinely treated arthroscopically include rotator cuff tears, glenohumeral instability, AC joint pathology, loose bodies, sepsis, osteochondritis dissecans, synovitis, chondral lesions, subacromial impingement, and calcific tendinitis.7,13,44,47
Magnetic Resonance Imaging
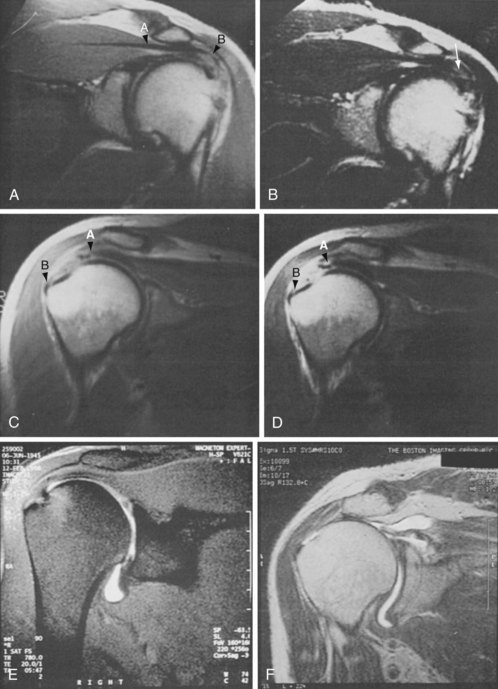
MRI has been used to diagnose partial-thickness and full-thickness rotator cuff tears, biceps tendon tears, impingement of the rotator cuff, synovitis, articular cartilage damage, and labral pathology associated with glenohumeral instability.48–50 In rheumatoid arthritis, MRI is reported to be more sensitive than plain radiographs in determining soft tissue abnormalities and osseous abnormalities of the glenoid and humeral head.51
One of the most valuable diagnostic uses of MRI is in rotator cuff pathology. Morrison and Offstein52 studied 100 patients with chronic subacromial impingement syndrome using arthrography and MRI. MRI was 100% sensitive but only 88% specific in confirming arthrography-proven rotator cuff tears. Nelson and associates53 studied 21 patients with shoulder pain and found MRI to be more accurate than CT-arthrography or ultrasound in identifying partial-thickness cuff tears. These investigators also reported MRI to be as accurate as CT-arthrography in the diagnosis of abnormalities of the glenoid labrum.53
Characteristic MRI findings in rotator cuff tears include a hypointense gap within the supraspinatus muscle tendon complex on T1-weighted films, absence of a demonstrable supraspinatus tendon with narrowing of the subacromial space, and an increased signal within the supraspinatus tendon on T2-weighted images.54 Seeger and colleagues,55 reporting the results of 170 MRI studies, found that T1-weighted images were highly sensitive for identifying abnormalities within the supraspinatus tendon, but T2-weighted images were required to differentiate tendinitis from a small supraspinatus tendon tear. Large full-thickness tears could be identified, however, on T1-weighted and T2-weighted images. Figure 46-12 depicts common shoulder pathology as seen by MRI. MRI is almost as sensitive as and is more specific than scintigraphy in the diagnosis of osteonecrosis and neoplastic lesions around the shoulder.
Electromyography and Nerve Conduction Velocity Studies
EMG and nerve conduction velocity studies can help differentiate shoulder pain from pain of neurogenic origin. They also may be beneficial in determining the localization of neurogenic pain to a particular cervical root, the brachial plexus, or a peripheral nerve.56,57
Injection
Injection of local anesthetics and glucocorticoids is a useful technique for the diagnosis and treatment of shoulder pain.58 The physician must have a thorough understanding of the anatomy of the shoulder girdle and a presumptive diagnosis to direct the injection properly. Injection of referred pain areas may be misleading. In a patient with lateral arm pain secondary to deltoid bursal involvement from calcific tendinitis of the supraspinatus tendon, injection should be performed in the subacromial space, rather than in the area of referred pain in the deltoid muscle. It is often better to use a posterior or lateral subacromial approach when injecting a rotator cuff tendinitis in a patient with anterior impingement symptoms because it is easier to enter the subacromial region posteriorly or laterally, and this approach is less traumatic for contracted anterior structures.
Potential Diagnostic Tests
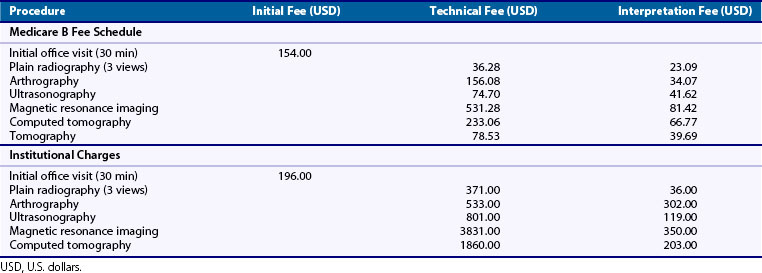
Table 46-2 lists reimbursement and charges for various shoulder diagnostic tests based on 2011 Medicare fee schedules and 2011 charges at a single institution. The choice of a specific test depends on its sensitivity, specificity, and cost-benefit analysis. History and physical examination are the most important factors in establishing diagnosis of the painful shoulder. Plain radiographs (three views) should be the first radiographic tests performed. Although not as sensitive as the more sophisticated tests, plain radiographs can identify arthritic change, calcific tendinitis, established osteonecrosis, and most neoplasms.
Intrinsic Factors Causing Shoulder Pain
Periarticular Disorders
Shoulder Impingement and Rotator Cuff Tendinopathy
One of the most common nontraumatic causes of shoulder pain is impingement with rotator cuff tendinopathy. In 1972, Neer9 described his results of 100 anatomic shoulder dissections and coined the term impingement syndrome. Impingement may be defined as the encroachment of the acromion, coracoacromial ligament, coracoid process, or AC joint on the rotator cuff as it passes beneath them during glenohumeral motion. The function of the posterior rotator cuff is to abduct and externally rotate the humerus. The cuff with the biceps tendon serves as a humeral head depressor to maintain the head centered within the glenoid fossa as the cuff and to use the deltoid to elevate the arm.59–61
Controversy continues, however, as to the exact cause of impingement, that is, whether it is a primary, intrinsic, degenerative event within the tendon with superior migration of the head on arm elevation and secondary impingement on the acromion, or purely mechanical attrition of the tendon with primary impingement against the acromion. The mechanical impingement of the rotator cuff may be influenced by variations in the shape and slope of the acromion.62,63 The supraspinatus outlet may become narrowed from proliferative spur formation of the acromion or degenerative changes in the AC joint. These changes, along with intrinsic degenerative changes of the rotator cuff, may lead to rotator cuff tear, but the exact pathogenesis remains controversial. Many studies have found a strong correlation between degenerative hypertrophic spur formation, with its resulting narrowing of the supraspinatus outlet, and the presence of full-thickness cuff tears,9,19,64–71 but clinical studies have failed to confirm whether hypertrophic changes in the coracoacromial arch are caused by the cuff lesions, or whether these changes themselves cause the lesions.
Neer9 developed a staging system for description of impingement lesions of the shoulder. A stage I lesion involves edema and hemorrhage of the rotator cuff and is typically found in individuals younger than 25 years who are active in overhead athletics. The condition usually responds to conservative treatment that includes rest, anti-inflammatory medication, and physical therapy. Stage II lesions usually occur in the 30s or 40s and represent the biologic response of fibrosis and thickening of the tendon after repeated episodes of mechanical impingement over time. Lesions are treated conservatively, as in stage I, but attacks may recur. If symptoms persist despite adequate conservative management for longer than 6 to 12 months, surgical intervention is warranted. Stage III lesions involve rotator cuff tears, biceps tendon rupture, and bone changes, and they rarely occur before age 40. Patients may present with pain, weakness, or supraspinatus atrophy, depending on the chronicity of the tear. Surgical treatment depends on the patient’s age, loss of function, weakness, and pain.
The impingement sign as described by Neer9 (Figure 46-13) is useful in the diagnosis of rotator cuff tendinopathy. The patient often describes a catch as the arm is brought into the overhead position. The patient may be observed to raise the arm by abduction and external rotation to clear the greater tuberosity of the acromion, bypassing the painful area. A typical painful arc usually occurs between 70 degrees and 110 degrees of abduction. Neer9 also described an impingement test that involves injection of lidocaine into the subacromial bursa. Relief of pain is a positive impingement test result and usually indicates rotator cuff origin of the shoulder pain.
Radiographs in the early stages of cuff tendinopathy may be normal or may reveal a hooked acromion. As the disease progresses, sclerosis, cyst formation, and sclerosis of the anterior third of the acromion and the greater tuberosity may be observed. An anterior acromial traction spur may appear on the undersurface of the acromion lateral to the AC joint and represents contracture of the coracoacromial ligament. Late radiographic findings include narrowing of the acromiohumeral gap, superior subluxation of the humeral head in relation to the glenoid, and erosive changes in the anterior acromion.71 Arthrography, MRI, and ultrasound may be helpful in diagnosing a full-thickness tear of the rotator cuff in association with stage III disease. In some cases of chronic large rotator cuff tears, proximal migration of the humeral head leads to a pattern of degenerative arthritis termed cuff-tear arthropathy.
An integrated program of occupational and physical therapy often precludes the need for surgery in patients with stage II disease. Job modification for individuals with impingement syndrome caused by overuse may alleviate symptoms. Businesses are becoming increasingly aware of the cost savings associated with proper job ergonomics.72,73
The initial rehabilitation in stage II impingement consists of cessation of repetitive overhand activity. Ice, NSAIDs, and local injections also may be beneficial. Initial physical therapy includes passive, active-assisted, and active range of motion combined with stretching and mobilization exercises to prevent contracture. As pain and inflammation subside, isometric or isotonic exercises are used to strengthen the rotator cuff musculature. Isokinetic training at variable speeds and in variable positions is instituted before the patient is returned to full activity. For patients with a job-related injury, it is crucial to review and modify job mechanics to prevent recurrent episodes that can cause further disability and may precipitate the need for surgery.72
Neer19 suggested that a patient with refractory stage II disease may respond to division of the coracoacromial ligament and bursectomy of the subacromial bursa. Open anterior acromioplasty as described by Neer has become accepted as the procedure of choice for stage II and III impingement lesions, with many investigators reporting high success rates in treating impingement syndrome and rotator cuff tears.74–77 Reported results show good and excellent relief of symptoms in 71% to 87% of patients treated by the open surgical procedure.78–81
In 1985, Ellman45 described the technique of arthroscopic subacromial decompression. His initial results46 and the results of others are comparable with those of open surgical techniques.47,82 Arthroscopic subacromial decompression has become a widely accepted treatment for refractory stage II and III impingement lesions. The procedure can be done as outpatient surgery, and because no deltoid is detached, as with the open technique, the procedure facilitates rehabilitation and increases overall recovery rates.
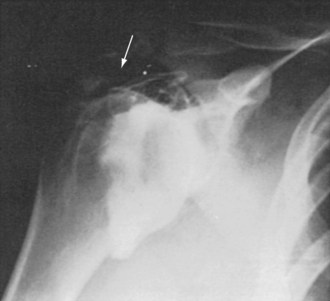
Calcific Tendinitis
Calcific tendinitis is a painful condition around the rotator cuff that is associated with deposition of calcium salts, primarily hydroxyapatite.83–85 The cause of calcific tendinitis is unknown. The commonly accepted cause is degeneration of the tendon, which leads to calcification through a dystrophic process.85 A common clinicopathologic correlation is seen in three distinct phases of the disease process: the precalcific or formative phase, which can be relatively painless; the calcific phase, which tends to be quiescent and may last months to years; and the resorptive or postcalcific phase, which tends to be painful, as calcium crystals are resorbed.83 Although it is more common in the right shoulder, at least a 6% incidence of bilaterality has been reported. Patients with bilateral shoulder involvement often have the syndrome of calcific periarthritis, in which calcium hydroxyapatite crystals are found at multiple sites.86 Patients usually present with impingement-type pain in the affected shoulder during overhead activity. The pain may seem to be out of proportion to any objective physical findings. The patient may describe difficulty sleeping on the shoulder and trouble falling asleep. Symptoms may last a few weeks or a few months.
The incidence of calcific tendinitis varies in the literature among asymptomatic individuals from 2.7% to 20%. Most calcification occurs in the supraspinatus tendon, and 57% to 76.7% of patients are women. The average age of patients is 40 to 50 years.83,87
Codman1 pointed out the localization of calcification within the tendon of the supraspinatus. He provided a detailed description of the symptoms and the natural history of this condition. In describing the phases of pain, spasm, limitation of motion, and atrophy, he noted the lack of correlation between symptoms and the size of the calcific deposit. According to Codman, the natural history includes degeneration of the supraspinatus tendon, calcification, and eventual rupture into the subacromial bursa. During the latter phase, pain and decreased motion can lead to adhesive capsulitis (see Figure 46-8).
Several factors may affect localization of calcium within the supraspinatus. Many patients have an early stage of impingement, which compresses the supraspinatus tendon on the anterior portion of the acromion.9,19 This long-standing impingement may lead to local degeneration of tendon fibers. In patients without impingement, localization of calcium within the supraspinatus may be related to the blood supply of the rotator cuff, which normally is derived from an anastomotic network of vessels from the greater tuberosity or from the bellies of the short rotator muscles.84 The watershed of these sources is just medial to the tendinous attachment of the supraspinatus.88 Rathburn and Macnab89 referred to this watershed as the critical zone and pointed out that during abduction this area was rendered ischemic.
Patients with discrete calcification and perhaps associated adhesive capsulitis (see Figure 46-8) may be at a stable phase, in which calcium produces a mechanical block and is unlikely to be resorbed. For these patients, mechanical removal of calcific deposits and correction of associated pathologic lesions may be necessary.90–92 Percutaneous disruption of calcified areas may be performed using a needle directed by fluoroscopy. This technique allows lavage and injection, but does not treat associated impingement. Subacromial arthroscopy allows mechanical débridement of calcific deposits under direct visualization. This technique can be combined with arthroscopic removal of the inflamed bursa and decompression of associated impingement. Improved results have been noted with complete removal of calcific deposits.93 In many cases of refractory calcific tendinitis associated with impingement, open or arthroscopic acromioplasty, subacromial bursectomy, and decompression are indicated.
Rotator Cuff Tear
Pathophysiology
Spontaneous tear of the rotator cuff in an otherwise normal individual is rare.19 It can occur in patients with rheumatoid arthritis or systemic lupus erythematosus as part of the pathologic process with invasion from underlying pannus. Metabolic conditions such as renal osteodystrophy and agents such as glucocorticoids occasionally are associated with cuff tears. Most patients report a traumatic episode, such as falling on an outstretched arm or lifting a heavy object. The usual presenting symptoms are pain and weakness of abduction and external rotation. Crepitus and even a palpable defect may be associated. Long-standing tears generally are associated with atrophy of the supraspinatus and infraspinatus muscles. It may be difficult to differentiate a painful tendinitis from a partial-thickness or a small full-thickness cuff tear.
Controversy continues about the exact cause of cuff tendinopathy.88,92,94,95 Most likely, the pathophysiology involves a combination of factors, including decreased vascularity and cellularity of the tendon, along with changes in the collagen fibers of the tendon that occur with aging.
Loss of motion with subsequent capsular tightness, particularly in the posterior capsule, may lead to cephalad migration of the humeral head, with subsequent impingement of the cuff under the coracoacromial arch.96 Rehabilitation exercises stress regaining a normal range of motion. To achieve full, painless motion, the normal relationship of glenohumeral to scapulothoracic motion must be achieved.16,17,97
Diagnosis
History
Patients with nontraumatic tears of the rotator cuff report symptoms of chronic impingement. Loss of motion and a feeling of stiffness are often noted with extremes of motion, along with difficulty during activities of daily living, such as combing the hair, hooking a bra strap, putting on a shirt or coat, and reaching into the back pocket. In chronic cases of cuff tendinopathy, loss of motion usually occurs. Limitation of internal rotation occurs initially, is caused by posterior capsular contracture, and is often associated with posterior shoulder pain with adduction of the ipsilateral shoulder. Further shoulder impingement occurs with forward flexion because of superior migration of the humeral head against the anterior inferior acromion. This upward translation is analogous to the action of a yo-yo climbing on a string.96,98 Over time, loss of forward flexion, abduction, and external rotation occurs with passive and active motion of the shoulder.
Imaging
Plain radiographs are used in initial evaluation of impingement-type shoulder pain with cuff tendinopathy. An impingement series should be ordered, including an anteroposterior radiograph with a 30-degree cephalic tilt (Rockwood view), which can reveal osteophytes of the anterior os acromion and AC joint; a scapular Y view with a 10-degree cephalic tilt (supraspinatus outlet view), which can evaluate the type of acromion and reveal anterior and AC osteophytes; and an axillary view, which can evaluate the acromion for possible os acromionale. Calcific deposits within the rotator cuff tendon can be viewed best with rotational anteroposterior radiographs. Cuff arthropathy should be suspected if the acromial-humeral distance is less than 7 mm, or with the presence of cyst formation within the greater tuberosity, humeral head osteopenia, sclerosis around the greater tuberosity, or humeral head collapse. In advanced stages of cuff arthropathy, complete loss of glenohumeral joint space may be seen with superior migration and abutment of the humeral head against the undersurface of the acromion.59
In the past, shoulder arthrography was considered the “gold standard” for diagnosing full-thickness and partial-thickness rotator cuff tears, with greater than 90% sensitivity and specificity.33,99 Currently, arthrography with CT or MRI is routinely used to diagnose rotator cuff pathology, including full-thickness and partial-thickness tears.
Ultrasonography has been accurate in the diagnosis of full-thickness rotator cuff tears.39,100–103 Ultrasonography offers the advantages of being inexpensive and noninvasive, but disadvantages include unproven effectiveness in determining subacromial impingement, capsular and labral abnormalities, and partial cuff tears. The procedure and its results are technician dependent. Ultrasonography may have a useful role in determining the postoperative integrity of the cuff repair.38
MRI has been invaluable in evaluating rotator cuff tears. Sensitivity and specificity of MRI for diagnosing full-thickness cuff tears are 100% and 95%.104 Through the use of gadolinium or saline, partial tears that are otherwise difficult to detect with conventional imaging can be detected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree