7
Respiratory System
At the completion of this chapter the reader should be able to do the following:
1. Describe the basic anatomy and physiology of the respiratory system
2. Define common normal and abnormal respiratory patterns
3. Perform a basic evaluation of the respiratory system, including auscultation and percussion
4. Identify characteristics of normal and abnormal breath sounds
5. Recognize common pathological conditions including signs and symptoms, differential assessment, referral, standard medical treatment, and implications for participation in athletics
Overview of Anatomy and Physiology
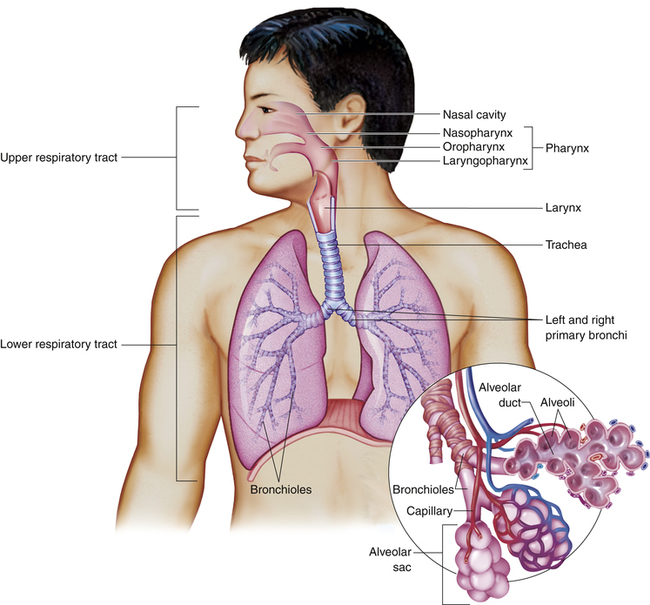
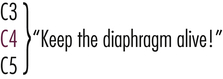
The upper respiratory section of the tract is responsible primarily for warming, humidifying, and filtering the air as it reaches the lower respiratory tract.1 As air is pulled from the external environment into the nasal passages, secretions from the paranasal sinuses add moisture. Cilia, tiny hairlike projections that line the upper airway, filter out fine particles of debris as the air moves into the lower respiratory tract.
The lower respiratory tract is composed of:
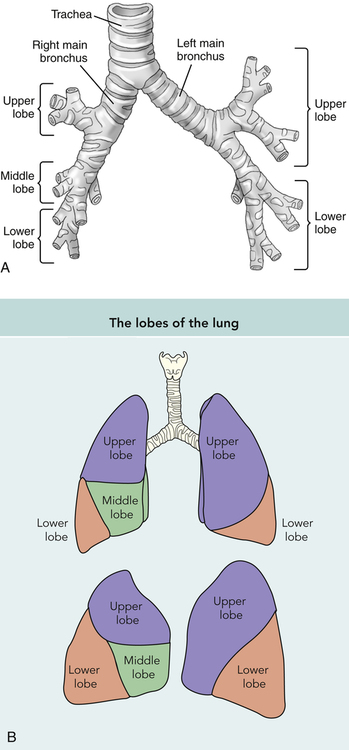
In the lungs each mainstem bronchus is further divided into bronchioles, and terminal alveoli (Figure 7-1). The tracheobronchial tree is a tubular system supported by cartilaginous rings that divide from the trachea into the right and left bronchi at approximately T4 or T5. These main bronchi then divide further into three branches on the right and two on the left. This tubular system serves as a passageway for air as it reaches the bronchioles and, finally, the terminal alveoli where the exchange of oxygen and carbon dioxide from the surrounding capillary beds takes place. The right lung is divided into three separate lobes: upper, middle, and lower, whereas the left has only an upper lobe and a lower lobe (Figure 7-2).
Evaluation of the Respiratory System
History and Inspection
An athlete may present with an acute or chronic respiratory condition while complaining of shortness of breath, abnormal breathing pattern, or cough. The first step in evaluation is to take a thorough history, which includes questions about how long the problem has existed, what exacerbates the condition, and the severity of the symptoms. In an athlete experiencing an acute respiratory attack, the history is abbreviated to only those questions necessary to determine the immediate course of action. A more thorough history is taken once the immediate emergency is controlled. If the patient complains of a cough the examiner asks the patient to describe the characteristics of the cough. Is it “dry” or “barking” or is it productive of sputum? Attention should also be paid to any discoloration of the sputum with the cough. Timing of the cough is also important: is the cough worse at night, as is often the case with asthma or gastroesophageal reflux disease (GERD) (see Chapter 9), or does it occur shortly after exertion as in exercise-induced bronchospasm? If shortness of breath or “dyspnea” is the complaint, the examiner attempts to discover its severity (e.g., how long the athlete has felt short of breath, what activity precipitated it, and does it occur at rest or only with activity). Associated chest pain is another important symptom to ascertain, to consider cardiac causes for dyspnea. Also, the examiner asks the athlete about any past history of respiratory infections, smoking, and environmental exposure to potential allergens.
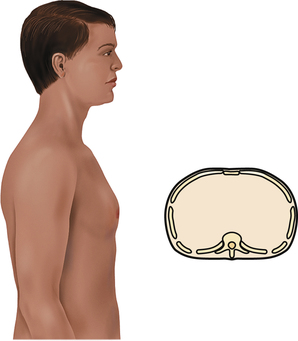
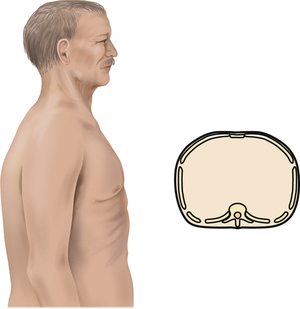
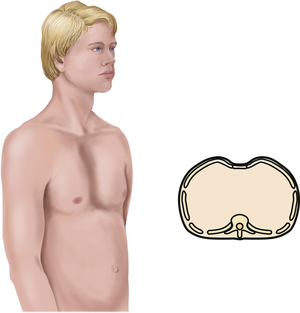
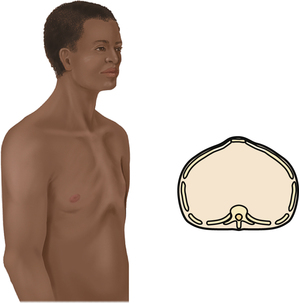
The chest is inspected after the history is taken. In the athletic training clinic, a chest examination is usually performed on a male athlete who has removed his shirt and on a female athlete dressed in a sports bra and shorts. The examiner inspects the chest for shape and configuration, including any skeletal deformities. Congenital deformities, such as scoliosis or kyphosis, as well as other chest deformities may be present and affect not only the shape of the chest but also the efficiency of respiration (Box 7-1).
Respiratory Patterns
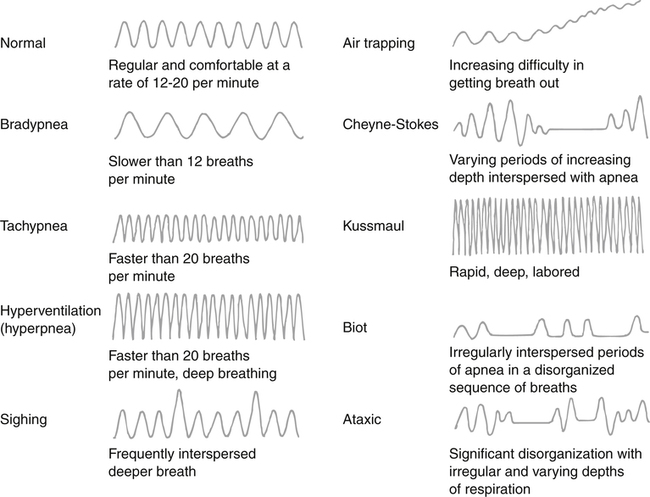
Normal respiration is unlabored, with 12 to 20 breaths per minute. When breathing becomes disordered, several patterns can emerge (Table 7-1). The term dyspnea refers to the subjective sensation of difficulty in breathing or shortness of breath. When patients have dyspnea, it is important to determine its severity. For example, does the difficulty occur at rest or only with exertion? Certain situations may produce dyspnea, such as eating, being exposed to cold ambient temperatures, or lying down at night. A condition known as paroxysmal nocturnal dyspnea is found in patients with underlying congestive heart failure and causes the individual to be short of breath when lying down at night. Dyspnea may accompany other symptoms in various disease processes, such as fever in infections such as pneumonia, wheezing in asthma, or chest pain in acute myocardial infarction.
TABLE 7-1
Classification of Breathing Terms
| Classification | Description |
| Tachypnea | Rapid breathing: >24 breaths/min |
| Hyperpnea | Tachypnea with very large breaths |
| Bradypnea | Slow breathing: <12 breaths/min |
| Hypopnea | Shallow, slow breaths |
| Orthopnea | Shortness of breath when lying down |
When breathing slows to fewer than 12 breaths per minute, it is called bradypnea. Electrolyte and acid–base disturbances can produce this pattern, but well-conditioned athletes with higher levels of cardiorespiratory fitness can develop this slowed breathing pattern as well. When breathing becomes slow and shallow it is called hypopnea and is seen as an adaptive response to pleuritic painful situations, such as rib fractures. The absence of spontaneous respiration is known as apnea. A condition called obstructive sleep apnea occurs primarily in obese patients during rapid-eye-movement sleep. Periods of apnea can also be found in a respiratory pattern called Cheyne-Stokes respiration, or periodic breathing. This breathing pattern can be normal in children and infants during sleep, but it also occurs pathologically in brain-damaged individuals. Figure 7-3 is a visual representation of the respiratory patterns.
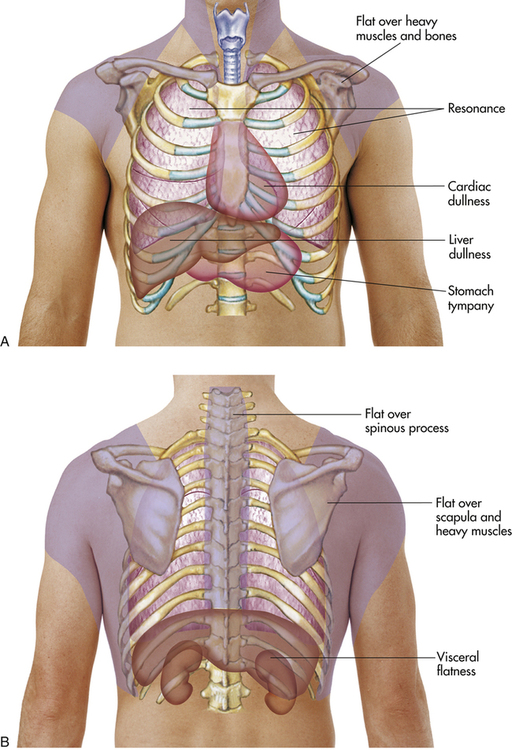
Palpation and Percussion of the Chest
The next step of the evaluation is to palpate the chest for symmetrical expansion. The examiner places the hands on the posterior chest wall with the thumbs placed on either side of the spine at the level of thoracic vertebra 9 (T9) or T10 (Figure 7-4, A).2 The examiner asks the athlete to inhale deeply and then watches the hands move apart symmetrically with the chest wall. Next, one feels for tactile fremitus. This is a palpable vibration that is generated from the larynx and transmitted through the patient’s bronchi and lungs to the chest wall. Use the palmar or ulnar surface of the hand to feel the vibrations over the posterior chest wall while the patient speaks the words “ninety-nine” (Figure 7-4, B). The intensity of the fremitus is not as important as the symmetry between lungs. Fremitus will decrease over the scapulae and will also decrease as the hand is moved distally to the lower posterior chest. Fremitus is increased when there is consolidation of the lung tissue such as in pneumonia. Decreased fremitus occurs when anything obstructs the transmission of the vibrations to the chest wall. Examples of obstructions include pleural effusion, pneumothorax, or emphysema, all of which are discussed in detail later in this chapter.
Percussion
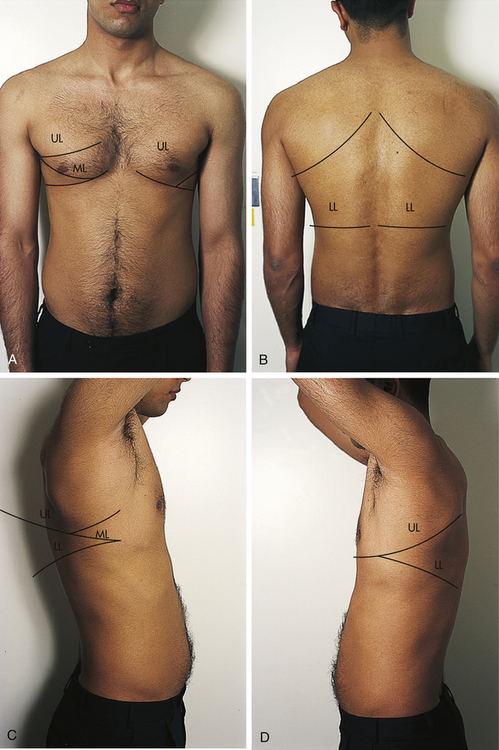
Direct percussion involves lightly striking the chest with the ulnar aspect of the fist. Indirect percussion involves the finger of one hand acting as the hammer, striking the finger of the other hand that is resting on the area of the chest being percussed (Figure 7-5). The striking action creates a vibration or resonance that, with training and practice, can be identified and quantified.
Percussion-generated sounds may be recognized by different characteristics, including intensity, pitch, and location. The general percussion tone over air is loud, over fluid it is less loud, and over solid areas it is soft.3 Common sounds produced by percussion are listed in Table 7-2. It is often difficult to quantify percussion tones, especially for the novice examiner. The examiner should practice identifying tones from various parts of the body to learn how to quantify them, specifically noting the change from one tone to another when moving from percussing a known air-filled body part, such as the lungs, to the abdomen or a muscle or over a bone.
TABLE 7-2
| Sound | Intensity | Pitch | Duration | Quality | Common Location |
| Tympany | Loud | High | Moderate | Drumlike | Enclosed, air-containing space |
| Resonance | Moderate to loud | Low | Long | Hollow | Normal lung |
| Hyperresonance | Very loud | Very low | Longer than resonance | Booming | Emphysematous lung |
| Dullness | Soft to moderate | High | Moderate | Thudlike | Liver |
| Flatness | Soft | High | Short | Flat | Muscle |
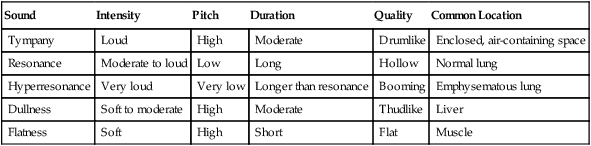
From Potter PA, Weilitz PB: Pocket guide to health assessment, St. Louis, 2003, Mosby, p 43.
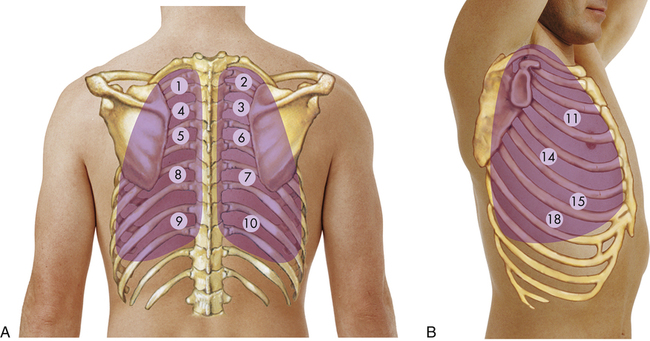
The examiner uses a systematic sequence of percussion, alternating from one side of the chest to the other to compare sounds (Figure 7-6) and starting at the apices of the lungs at the top of the shoulders. The predominant sound found at the top of the shoulders will be resonant. Progressing inferiorly, the examiner percusses the chest at approximately 5 cm intervals in the intercostal interspaces. In a healthy adult lung, resonance will be the predominant sound. Hyperresonance is found when too much air is present, such as in pneumothorax or emphysema. A dull note will occur over bone (e.g., over the scapula) or where there is abnormal density in the lungs, which is seen in pneumonia or pleural effusion.2 Dullness will also be found when percussing the inferior posterior chest wall over the liver and abdominal viscera (Figure 7-7).
Auscultation
Certain basic principles apply to auscultation regardless of the system being examined:
• Perform auscultation after history, observation, and palpation in order to gather as much information as possible from other sources first.
• Perform auscultation in a quiet environment.
• Listen for the presence or absence of sounds as well as their frequency, loudness, quality, and duration.
• Make sure the earpieces of the stethoscope fit comfortably, following the angles of the ear canal.
The examiner uses the part of the stethoscope that best relays the pitch of the sound sought. The diaphragm is used for high-pitched sounds, such as bowel, lung, and normal heart sounds, whereas the bell is used for low-pitched sounds.4 Abnormal heart and vascular sounds have a lower pitch and may be heard better with the bell.5 Table 7-3 describes common characteristics of sounds heard during auscultation.
TABLE 7-3
| Characteristic | Description |
| Frequency | Number of sound wave cycles generated per second by a vibrating object. The higher the frequency, the higher the pitch of a sound and vice versa |
| Loudness | Amplitude of a sound wave. Auscultated sounds are described as loud or soft |
| Quality | Sounds of similar frequency and loudness from different sources. Terms such as blowing or gurgling describe quality of sound |
| Duration | Length of time sound vibrations last. Duration of sound is short, medium, or long |
Characteristics of Normal and Abnormal Breath Sounds
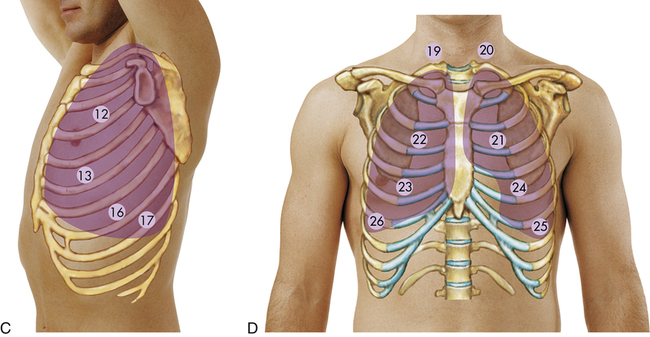
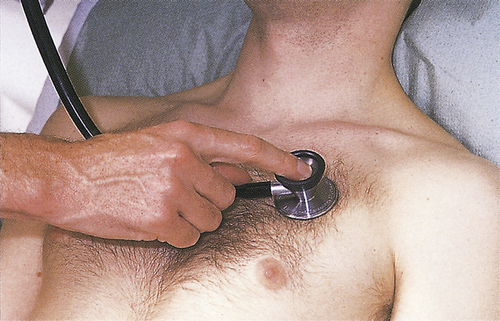
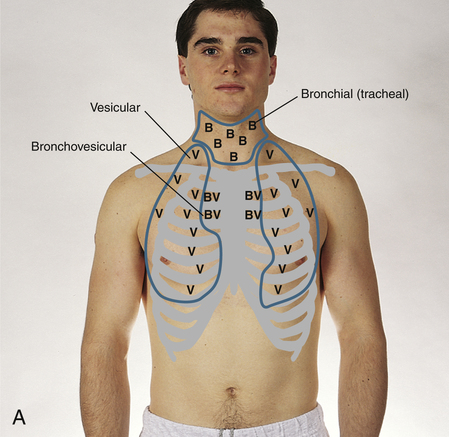
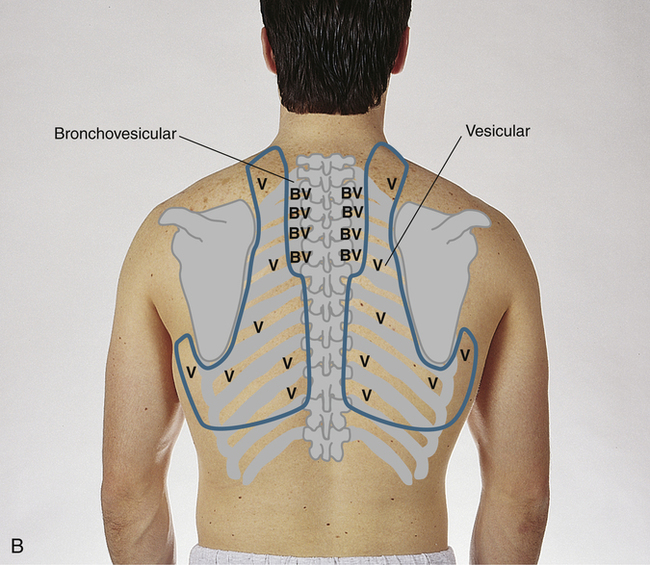
The diaphragm of the stethoscope is used on bare skin to auscultate the lungs. The examiner must listen systematically at each position throughout inspiration and expiration1,2 and evaluate lungs in the anterior, posterior, and lateral aspects to ensure that each lobe of the lungs is properly examined. Figure 7-8 shows the surface markings of the lobes of the lung. The examiner is always mindful of which lobe is being examined: the front of the chest provides access to primarily the upper lobes (Figure 7-9) whereas auscultation of the back exposes mainly the lower lobes of the lungs. One useful technique involves listening in the same sequence that is used in percussion from left side to right at symmetrical locations to make comparisons as the examiner moves downward from the apex to the base of the lungs. When the athletic trainer listens to the lungs, three different sounds can be appreciated in normal individuals depending on the position of the stethoscope (Figure 7-10):
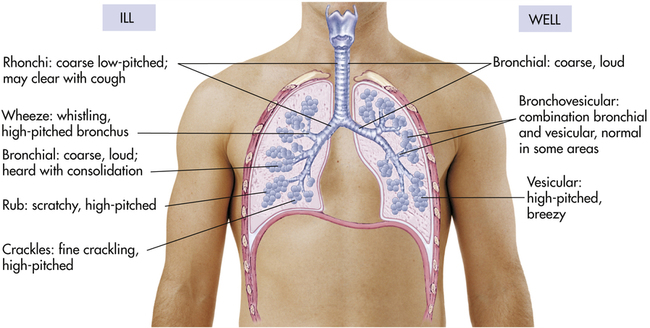
Bronchial breath sounds are loud, high-pitched, and predominantly expiratory. These sounds represent air moving through large airways and sound more tubular. They are normally heard only over the trachea in the anterior chest midline.
Bronchovesicular breath sounds are heard when air moves through medium-sized airways, such as the mainstem bronchi, and can be heard both anteriorly and posteriorly, toward the center of the thorax. These sounds are of medium pitch and moderate intensity. Inspiratory and expiratory phases are approximately equal.
Vesicular breath sounds predominate in most of the peripheral lung tissue and represent the air as it moves into the smaller airways, such as the bronchioles and lung parenchyma. These sounds are soft, low-pitched noises that involve mostly inspiration.
When disease affects the lungs, normal breath sounds are altered depending on the condition (Table 7-4). Fluid in the pleural space may make breath sounds distant or even absent; however, fluid within the lung parenchyma, such as in pulmonary edema or pneumonia, may accentuate breath sounds because sound is transmitted quicker through liquids than through air. Similarly, consolidated masses within the lungs, such as pneumonia, will transmit louder sounds. Most of the abnormal breath sounds heard will be superimposed on normal breath sounds and are called adventitious breath sounds (Figure 7-11).
TABLE 7-4
Physical Findings Associated With Common Respiratory Conditions
| Condition | Inspection | Palpation | Percussion | Auscultation |
| Asthma | Tachycardia | Occasional hyperresonance | ||
| Bronchitis | Tactile fremitus | Resonance | ||
| Pneumonia | Tachypnea | Increased fremitus in presence of consolidation | Dullness if consolidation is great | |
| Pneumothorax | Hyperresonance |
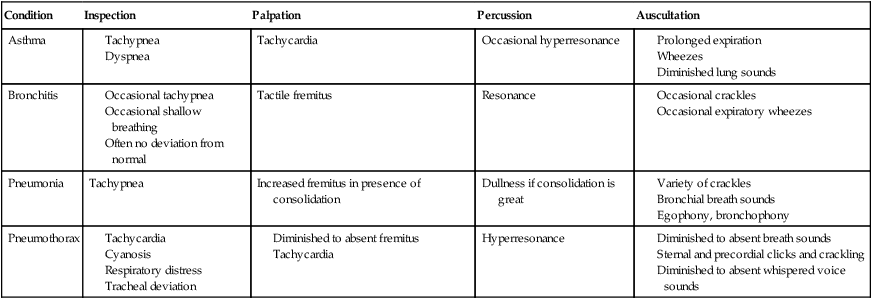
Modified from Seidel HM, Ball JW, Dains JE, et al: Mosby’s guide to physical examination, ed 5, St. Louis, 2003, Mosby, pp 397–398.
Wheezes are also adventitious sounds that represent airway obstruction from mucus, spasm, or even a foreign body. These sounds are usually more pronounced during expiration and can be either high-pitched, musical noises in the smaller airways (e.g., asthma) or low-pitched in the larger airways (e.g., bronchitis). Such low-pitched, sonorous wheezes are also referred to as rhonchi. The stridor sound is also caused by airway obstruction and can often be confused with wheezes. The obstruction in stridor generally occurs in the central airways, such as the trachea or larynx, and is more pronounced during inspiration as opposed to the expiratory-predominant wheeze.1,2 Croup is a condition that classically can produce stridor. Pleural rubs are sounds that occur outside the respiratory tree and result from friction between visceral and parietal pleura in conditions that cause inflammation of the pleura, such as pleurisy, or pleuritis. Usually low-pitched, they can be heard in both inspiration and expiration and can resemble the sound made when two balloons are rubbed together.
The athletic trainer must become familiar with normal breath sounds through auscultation, thus better realizing when adventitious sounds are present in the lungs. Box 7-2 summarizes the steps in the evaluation of an athlete’s respiratory system. In addition, the athletic trainer needs to be vigilant in recognizing the signs and symptoms of respiratory disorders.