Proximal tibial fractures
INTRODUCTION
In North America as our population ages, an increasing number of elderly patients (see Chapter 1) sustain injuries including tibial plateau fractures. Unfortunately, there is a relative paucity of evidence based, high quality literature reporting on treatment techniques and outcomes for patients in this age group who sustain tibial plateau fractures. The majority of studies on proximal tibia fractures stratify the analysis based upon fracture or type of treatment without assessment of the elderly as a subgroup. Given this lack of published information, treatment recommendations in this chapter are often extrapolated from studies on tibial plateau fractures without age or bone quality stratification combined with opinions based on our personal experience.
Proximal tibia fractures are complex injuries and the presence of osteoporosis or osteopenia complicates management. Even low energy injuries lead to greater fracture comminution than would occur in patients with normal bone stock.1 Given the relative frailty of the bone there is an increased risk of secondary displacement with both operative and non-operative management. Even with modern implant designs and fixation techniques the effectiveness of operative treatment in maintaining reduction is decreased in the setting of compromised bone stock. Additionally, elderly patients do not tolerate prolonged periods of non-weight bearing or immobilization.
Despite these difficulties in the treatment of elderly patients who sustain proximal tibia fractures, the treatment may be less intensive and in some cases easier than some other osteoporotic peri-articular fractures involving the lower extremity. For instance, non-operative treatment and mobilization is possible for many patterns of injury. In contrast, patients who sustain distal femur fractures or hip fractures require surgical management prior to mobilization. When surgery is chosen less invasive surgical approaches and implants are often possible in the proximal tibia. The knee tolerates joint incongruity to a greater extent than the hip joint.2 Despite articular incongruity and radiographic evidence of posttraumatic osteoarthritis it is not uncommon for patients to remain relatively asymptomatic and function well, as long as the overall alignment of the limb is maintained.3 For these reasons in elderly patients with osteoporosis and a tibial plateau fracture, it is often appropriate to minimize extensive, invasive soft tissue compromising surgical approaches and focus on preserving mechanical alignment of the limb while minimizing the risk for complications.
In this chapter we use elderly age, poor bone quality, osteoporosis and osteopenia relatively interchangeably since there is substantial overlap in these conditions. The epidemiology, evaluation and approach to treatment of these challenging injuries will be covered.
EPIDEMIOLOGY
Proximal tibia fractures occur throughout the entire spectrum of patient age, from young patients who sustain physeal injuries to the most elderly patients where low energy mechanisms can lead to a variety of different fracture patterns. Multiple studies have demonstrated that the highest incidence of tibial plateau fractures is in the fifth decade of life followed by the fourth and six decades.4,5 There are also gender differences, with men typically having a higher incidence in the second, third and fourth decades, often due to higher energy mechanisms. Women have an increasing incidence of tibial plateau fractures with age, often peaking in the seventh decade.5 It is in this population that osteoporotic proximal tibia fractures are most commonly encountered and lower energy mechanisms start to predominate.5,6
While the specific incidence of tibial plateau fractures complicated by osteoporosis remains difficult to elucidate, such fractures are felt to be increasingly common. Previous studies have demonstrated that approximately 30–40% of all tibial plateau fractures may have some degree of underlying osteoporosis or osteopenia.5,6 Given the increasing population of elderly individuals and with improved techniques for assessing osteoporosis, a focused study might demonstrate that this is a conservative estimate.
CLASSIFICATION
Fractures of the tibial plateau represent a diverse and complex group of injuries. There are many different mechanisms of injury with varying degrees of radiographic displacements and associated soft tissue injuries. These varied injuries require different evaluation and treatment techniques, yet all remain classified as fractures of the tibial plateau. Nowhere is this variation more apparent than in elderly patients, where injury patterns span the spectrum from severe high energy bicondylar fracture dislocation patterns resulting from motor vehicle accidents to low energy valgus loading fractures with joint impaction.
The two most commonly used classification schemes for tibial plateau fractures are the Schatzker classification6 and the AO/OTA classification.7 These classifications are utilized for elderly patients and have similar relevance to when they are used in younger patients with tibial plateau fractures.
The relative incidence of tibial plateau fractures varies in patients with osteoporosis or osteopenia compared to that of patients who have normal bone. The lateral split depression fracture (Schatzker II, 41-B) is the most common fracture pattern in patients with osteoporosis or osteopenia.3 In a patient with compromised bone stock, a valgus load leads mainly to overloading of the lateral plateau and a split depression fracture, whereas in an individual with normal bone in some cases a bone contusion or medial ligamentous injury may occur as a result of the better structural integrity of the subchondral bone. Likewise a pure split fracture (Schatzker I) is rare in patients with osteoporosis because structural integrity of the bone is requisite for this pattern. As opposed to younger patients with normal bone stock, bicondylar fracture patterns in the elderly may occur without high-energy mechanisms. When they do occur significant comminution and cancellous bone loss or impaction lead to difficulties in subsequent surgical management.8,9 and 10 Crushing, loss of bone stock and small soft articular fragments with metaphyseal comminution are common features of these patterns in elderly patients (Figure 39.1).
TREATMENT
Evaluation
Associated injuries to the soft tissues, including open wounds, compartment syndrome and vascular injuries, may all be associated with high-energy tibial plateau fractures.11,12 High energy fracture patterns may occur from relatively low energy trauma in patients with osteoporosis or osteopenia so these associated injuries must be considered and the patient carefully evaluated even when the mechanism is a simple fall.
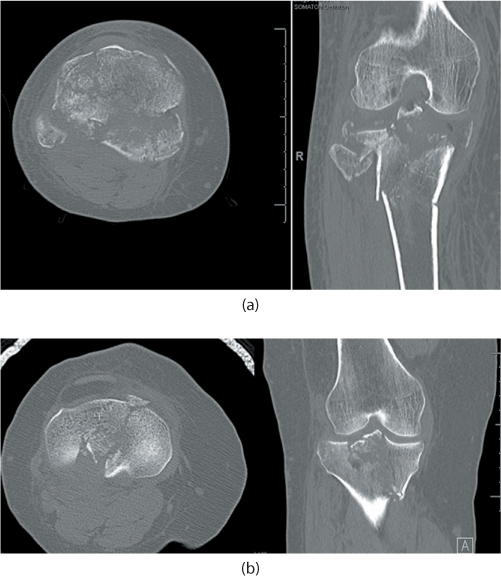
Figure 39.1 (a) Axial and coronal CT images of a 72-year-old woman who sustained a closed bicondylar tibial plateau fracture. (b) Axial and coronal CT images of a 38-year-old woman who sustained a tibial plateau fracture involving both condyles. Note that despite similar injury mechanisms there is significantly more metaphyseal comminution and cancellous bone impaction in the older woman (a).
Although not clearly documented in the literature, vascular injuries may be more common in severe injury patterns because of less compliance of potentially calcified vessels13 (Figure 39.2). In elderly patients the soft tissue envelope may be less resilient and more poorly vascularized. For this reason careful assessment of the soft tissues prior to surgical approaches is equally or more important than in younger patients. The soft tissue envelope in elderly patients with osteoporotic fractures may be less tolerant of extensive surgical approaches.
Ligamentous injuries about the knee are commonly associated with tibial plateau fractures.14,15 For example, in lateral split depression injuries or local lateral compression fractures from a valgus load on the knee, a common injury pattern in the elderly population, a medial collateral ligament (MCL) injury may occur. However the incidence of MCL injury is generally thought to be higher in patients with normal bone stock since osteopenic bone protects ligamentous structures about the knee, as failure occurs through the bone rather than soft tissue.3

Figure 39.2 Lateral radiograph of an 89-year-old man with a bicondylar tibial plateau fracture. Vascular calcifications (black arrow) can be easily seen.
The physical exam is important and should be similar to that for other patients with tibial plateau fractures. This includes inspection of the soft tissues as well as a detailed neurovascular examination, both of which are critical for determining subsequent treatment strategies. Stability testing or ligamentous examination may be appropriate in low energy type fracture patterns when considering non-operative management, as mechanical stability and limb alignment are important for a satisfactory outcome.16 Sometimes just assessing limb alignment in the supine position is helpful in assessing likely deformity without surgical treatment.
Radiographic assessment and work-up of tibial plateau fractures is similar regardless of bone quality. This includes anteroposterior (AP), lateral and caudal or plateau view radiographs. Radiographs of adjacent joints including the hip and ankle may be indicated. When surgical management is considered, a CT scan of the injured extremity will assist with surgical planning. MRI may identify associated soft tissue injuries to menisci and ligaments but we do not routinely use it in all plateau fractures. In elderly patients we would rarely obtain an MRI since the need to assess and treat ligament and meniscal injuries is less. We could find no specific study addressing the treatment of intra-articular or periarticular soft tissue injuries of the knee in elderly or osteoporotic patients.
General considerations
The treatment of proximal tibia fractures in elderly patients with osteoporosis requires several considerations that can lead to different treatment techniques than what would be chosen for younger patients with good bone stock. Patients who are elderly or those with decreased bone stock from osteoporosis are more likely to have lower functional demands than those with normal stock. Additionally, complications occurring in elderly or infirm patients are particularly problematic. For these reasons less aggressive treatment techniques, including non-operative treatment, are often more appropriate than in younger or more active patients with a commensurate injury. The literature supports numerous surgical and non-surgical techniques that can achieve satisfactory outcomes after tibial plateau fractures in both young patients and in those who have underlying osteoporosis or osteopenia.3,10,17 Given this finding, a surgeon can be reassured that a potentially less aggressive surgical strategy may yield an acceptable outcome.
In deciding on treatment the surgeon should strongly consider those factors that lead to favourable outcomes. Central to this is avoiding limb malalignment. Malalignment greater than 10 degrees tends to alter the weight-bearing axis and predispose to an unfavourable prognosis. Like malalignment, ongoing instability in the knee is also poorly tolerated and attempts should be made to minimize it.5 Persistent intra-articular displacement is felt to be an important predictor of prognosis; however tolerances of residual articular displacement remain difficult to fully elucidate.18 This remains an area of ongoing controversy in both healthy and osteoporotic bone.16,19,20 Less aggressive treatment techniques designed only to maintain or restore limb alignment may be preferable to interventions designed to perfectly reduce the injured articular surface. When functional demands are very low, even limb alignment becomes less important. A modest deformity in a non-ambulatory patient will have little functional or cosmetic significance.
When possible, early joint motion for tibial plateau fractures should be instituted and indeed this is felt to be one of the main advantages of surgical management.19,21,22,23 and 24 It should be noted, however, that tibial plateau fractures treated non-operatively tolerate 4–6 weeks of immobilization without negative consequences.25
There is a clear association between poor patient outcomes and operative complications such as infection, wound breakdown and neurologic injury, so whenever possible these should be avoided.11,26 Complications may require prolonged and difficult treatment particularly in injuries that result from higher energy mechanisms.
Nonoperative treatment
Nonoperative treatment of tibial plateau fractures may be an option in elderly patients. Unlike some fractures in other areas of the body including the hip or distal femur, prolonged skeletal traction is not required for nonoperative management. Patients may be mobilized with a simple splint or brace without significant difficulty. Surgery may therefore be reserved for those cases where predictable improvements in ultimate knee function may be achieved. Given the increased risks of complications and difficulties of surgical management in elderly patients with poor bone stock, the indications for nonoperative treatment in this patient population are increased.25 For those individuals who have lateral split depression type fractures without significant valgus instability, treatment would consist of early knee range of motion and protected weight bearing with a lightweight maneuverable soft brace (Figure 39.3). Generally progression to full weight bearing may begin at 6 weeks following injury. Most commonly, clinical symptoms including pain and significant swelling recede and patients are able to return to full baseline function within several months following the initial injury. Often when patients have unstable injury patterns such as valgus instability, more rigid immobilization in a formal cast may be considered. This however has to be weighed against the decreased mobilization and the potential need for increased nursing support. Segal and colleagues have shown that weight bearing in a cast-type brace may be allowed with the expectation of no greater than 2 mm of increased displacement.27 With increased initial displacement of the fracture and in bicondylar fracture patterns, non-operative management often results in malalignment and less satisfactory outcomes.25
In higher energy injury patterns, such as bicondylar tibial plateau fractures or in fractures with predictable instability greater than 10 degrees or in those where satisfactory limb alignment cannot be achieved, skeletal traction may be considered; however, in such patients prolonged immobility or bed rest is often poorly tolerated, and operative management may be more appropriate.28 Traction with a spanning fixator will usually be preferable.29
Indications for operative treatment
As with all patients who undergo operative management of displaced tibial plateau fractures, but particularly in those with compromised bone quality, many factors must be considered prior to surgery. It is clear that elderly patients undergoing surgical management, including reduction and fixation, have worse outcomes than those patients who are otherwise healthy and have normal bone stock.6,30 These less than satisfactory results may in part result from a higher rate of postoperative settling or collapse of the articular surface and decreased stability of implants used to hold fracture fragments. Other considerations include the risks of anaesthesia as well as the continued potential for decreased mobility even with successful operative management. Despite these potential risks, there are patients who will clearly benefit from thoughtful and carefully planned and executed surgical intervention. As in many situations, a surgical plan must be individualized based on the patient, fracture pattern and the quality of bone. Likewise, a patient’s baseline functional demands and ultimate expectations must be also carefully considered. When limb malalignment is predicted with non-operative management in patients with split lateral depression fractures with significant articular depression, baseline valgus deformity or bicondylar fracture patterns with large initial displacements, surgery should be contemplated.25 When surgery is chosen, some newer techniques may have particular advantages in patients with poor bone stock. These include percutaneous insertion techniques that are less damaging to the soft tissues and locking plate and screw constructs that provide improved fixation and in some cases avoid more damaging soft tissue approaches, including extensile and dual approaches. Additionally, calcium phosphate cement may maintain articular elevation to a greater extent than autogenous graft.31 The use of external fixation with limited internal fixation may allow for control of coronal alignment, while at the same time minimizing surgical soft tissue dissections that can potentially lead to catastrophic complications.32 Spanning external fixation may be used in selected difficult fracture problems as a definitive treatment with or without limited internal fixation.
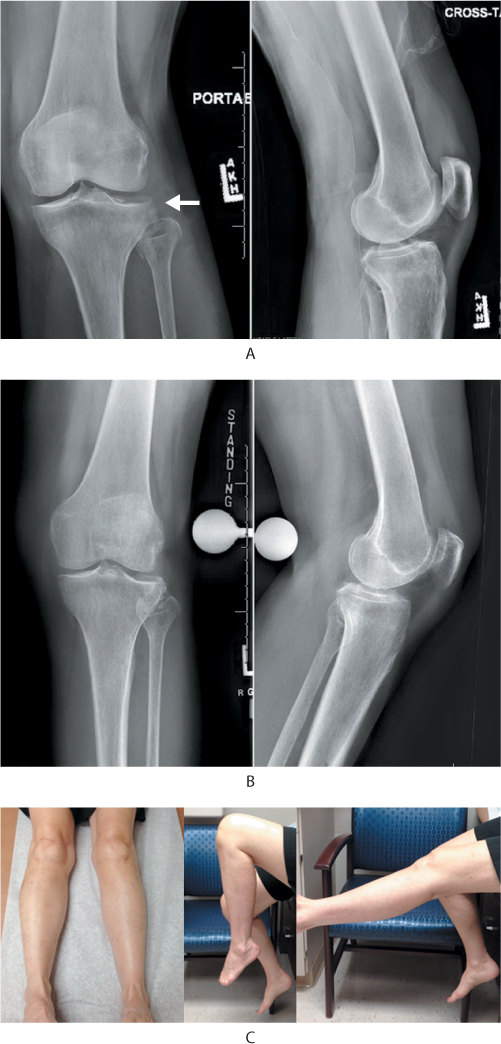
Figure 39.3 (a) Anteroposterior (AP) and lateral radiograph of 66-year-old woman who sustained a twisting injury to her left knee (note fracture line, white arrow). (b) Standing AP and lateral radiograph 8 weeks following injury. (c) Clinical photographs of the patient’s limb alignment, knee flexion and knee extension. The patient had 6 weeks of protected weight bearing with a hinged knee orthotic; range of motion was unrestricted when not ambulating.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








