Proximal humeral fractures
Treatment of two-part fractures
Treatment of three- and four-part fractures
INTRODUCTION
Recent data indicate that many elderly patients with displaced proximal humeral fractures do not benefit from surgical treatment even for complex fracture patterns. In most elderly there is some degree of physical impairment after fracture regardless of the fracture anatomy and treatment modality. The degree of impairment does not always correlate with the complexity of the injury, and some patients with minimally displaced fractures end up with pain and poor function. Pre-injury infirmity and medical comorbidity may strongly influence outcome after surgery. Poor bone quality and degenerative changes in the rotator cuff may further compromise outcome after surgery. Studies of outcome in the average patient or younger patients with proximal humeral fractures may not apply to older patients, and observer administrated measures of shoulder function (e.g. the Constant score) used to evaluate patients in clinical studies may overemphasize the importance of range of motion and strength. Some elderly patients have lower functional demands and may accept restricted strength and range of motion if pain is limited.
Evidence based recommendations for management according to age are sparse and the optimal treatment for proximal humeral fractures in the elderly has yet to be determined. The methodological quality of clinical studies has generally been low and recommendations are inconsistent. Current best evidence consists largely of uncontrolled case series with a high risk of bias. Systematic reviews have been unable to demonstrate statistically and clinically significant benefits from surgical treatment of displaced fractures.1,2,3,4,5,6,7,8,9,10,11 and 12 However, within the last 5 years new data from randomized trials have appeared in the literature13,14,15,16,17,18,19,20 and 21 and protocols for planned randomized studies have been published.22,23,24,25 and 26 It is likely that the next updated Cochrane review will contain some evidence based treatment recommendations.
This chapter is based on data from current randomized clinical trials, systematic reviews and large epidemiological studies. Whenever possible, data on elderly (65–79 years) and very elderly (80 and above) patients are reported separately.
EPIDEMIOLOGY
Proximal humeral fractures account for 4–6% of all fractures.27,28 and 29 They are associated with advanced age and osteoporosis. Falls from standing height account for about 94% of proximal humeral fractures in patients older than 65.30 The incidence of proximal humerus fractures is third only to fractures of the distal radius and the proximal femur. The lifetime risk of a fracture of the proximal humerus in women aged 50 or more is 13%.31 An increase in incidence from 32 to 105/100,000 per year between 1970 and 2002 has been reported.32 In women older than 80 years the incidence increased from 90 to 294/100,000 per year. Kannus et al. reported an incidence of 298/100,000 per year in women older than 60,33 and Court-Brown et al. recently reported an incidence of 392/100,000 per year in women older than 65, and 520/100,000 per year in women older than 80, compared to 147 and 261/100,000 per year in men.34 At least one previous fracture was found in 47% of patients. Together with low bone mineral density and diminished stature, a previous fracture is an independent risk factor for fracture of the proximal humerus.30 The odds ratio for sustaining concomitant fractures in patients with a proximal humeral fracture is 2.2.35 In a Swedish population the median survival time after a proximal humeral fracture was 9 years compared to 12 years in controls.36 In women aged 60–79 years with a proximal humeral fracture, the lifetime risk for a hip fracture is about 2.4.37 In an unselected population of 629 elderly patients a poor functional outcome (Constant score <55) after a proximal humeral fracture was reported in 27% of the patients after 1 year.38 The functional outcome was unrelated to fracture severity.
Distribution of fracture types
In Neer’s classic article from 1970,39 minimally displaced fractures accounted for 85% of all proximal humeral fractures in a population of patients with a mean age of 56 years (Figure 20.3). More recent studies in elderly populations have reported less than 50% minimally displaced fractures (Table 20.1).28,40,41 Three fracture patterns within the Neer classification (minimally displaced, two-part surgical neck and three-part [surgical neck and greater tuberosity]) account for 86% of all proximal humerus fractures.28 Fracture complexity is age and sex specific. Overall, 70% of three- and four-part displaced fractures occur in patients older than 60 years with a 1.72 times higher rate of three- and four-part fractures in women compared to men.42
Rotator cuff integrity
Fjalestad et al.43 obtained MRI scans of 76 non-operatively treated fractures of the proximal humerus at the time of injury and 1 year after injury and reported 22 full thickness defects presented at the time of injury and 10 more 1 year after fracture. Function measured with the Constant score 1 year after fracture corresponded with the presence of a rotator cuff defect at the time of injury. Given that rotator cuff degeneration is a normal part of human aging, it is not clear if this rate is greater than expected for age.
Bahrs et al.44 sonographically examined 302 patients with proximal humeral fractures 4 years after the injury. In 17% a full thickness rotator cuff defect was found on the fractured side, compared to 4% on the contralateral side. There was a significant correlation between four-part fractures and full thickness rotator cuff defects.
IMAGING
Preoperative assessment of proximal humeral fractures is usually limited to radiographs. A series including an anterior-posterior view, a perpendicular lateral/scapular view and an axillary view is most useful. In some institutions the axillary view is omitted because it can be painful. This may be unwise because the axillary view is the best view for ensuring the glenohumeral joint is not dislocated, it can add important information on tuberosity displacement, and it improved observer agreement on classification in one study.45 Most institutions have access to computed tomography (CT) and three dimensional (3D) CT scans (Figures 20.1 and 20.2). CT may be useful in preoperative planning and might improve reliability of classification but no study has reported a beneficial effect on patient outcome. There is generally limited correspondence between imaging appearance and functional outcome in proximal humeral fractures.
CLASSIFICATION
Agreement on classification
The most frequently used classification systems for proximal humeral fractures are the Neer classification (Figure 20.3) and the AO classification (Figure 20.4). They are based on assessment of two or three perpendicular preoperative radiographs.
Within the last two decades, more than 20 observer studies and systematic reviews have reported that orthopaedic surgeons greatly disagree when classifying according to the Neer and the AO classification. They have consistently reported low kappa values for interobserver agreement ranging from 0.17 to 0.52.46,47 A review on agreement on four commonly used classification systems between experienced shoulder surgeons only, reported kappa values of between 0.15 and 0.44.48 Lack of consistency in classification may explain some of the discrepancies in treatment recommendations and outcome found in the scientific literature.
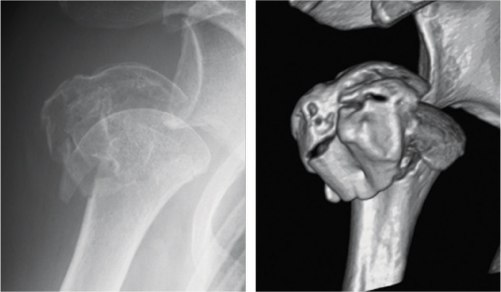
Figure 20.1 Radiograph (anterior-posterior view) and 3D CT reconstruction of a proximal humeral fracture.
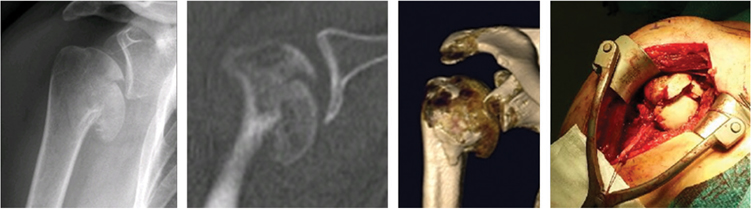
Figure 20.2 Imaging modalities in an articular surface fracture (AO C3.3). Radiograph, CT-scan, 3D CT reconstruction and intraoperative view.
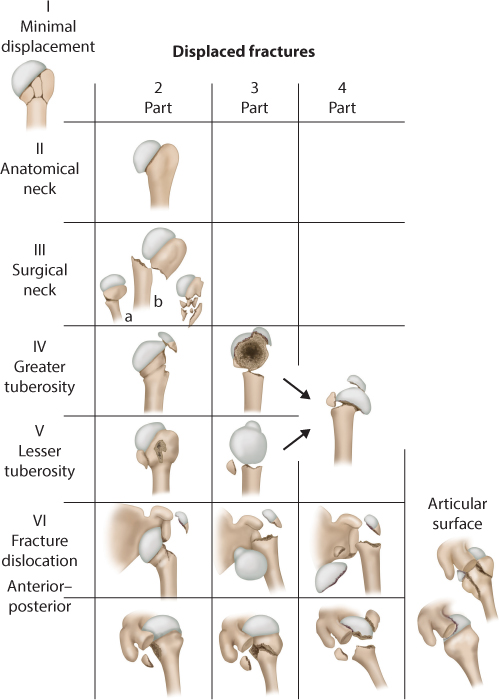
Figure 20.3 The 16 categories of the Neer classification. A fracture is considered displaced if one or more of the four anatomical segments (greater tuberosity, lesser tuberosity, humeral head and humeral shaft) are displaced more than 1 cm or angulated more than 45°. (Modified from Neer CS. J Bone Joint Surg Am 1970;52(6):1077–89. With permission from Rockwater, Inc.)
The low agreement does not improve through selection of experienced observers, by using high quality radiographs only, by reducing the number of classification categories, or by adding advanced pictorial modalities like CT scans or 3D CT reconstructions.46 However, systematical training of observers seems to improve agreement especially among shoulder specialists.49 There seems to be less agreement on complex fracture patterns.50
Agreement on treatment
One study found significantly higher agreement on treatment recommendations than on classification in a consecutive series of 193 radiographs from emergency units or orthopaedic wards.50 Only one third of changes in classification were followed by changes in treatment recommendation. The highest agreement was found on non-surgical treatment. It was concluded that the low observer agreement on the Neer classification may have less clinical importance than previously assumed.
Translation between classification systems
A common ‘fracture language’ is lacking in the scientific literature on proximal humeral fractures and the two most common classification systems are partly incompatible.51 The result is difficulty comparing outcome from clinical studies and ‘translation’ of treatment recommendations into other populations. For example, minimally displaced fractures can correspond to 15 different AO subgroups, ‘classic’ four-part fractures (Neer category 12) can be classified into at least eight different AO subgroups and AO type C fractures can appear as one-, two-, three- or four-part fractures in the Neer classification.51
Important clinical information is lost within both classification systems. Most importantly, a distinction between varus and valgus displacement is not found in the Neer classification, and a concise definition of displacement is lacking in the AO classification. Researchers and surgeons are encouraged to report data from both classification systems and cross-check their coding.51 Classification of proximal humeral fractures remains a challenge in clinical and scientific orthopaedics.
TREATMENT
Non-surgical treatment includes sling immobilization with immediate pendulum exercises or delayed active and passive exercises. Some advocate attempted manipulative reduction (usually impaction of the humeral shaft into the head of the humerus) followed by non-operative treatment. Surgical treatments include manipulative reduction and percutaneous pinning, and open reduction and internal fixation with a plate and screws, tension-band wiring, suture anchors, Kirschner wires, helix wiring, transosseous suture or intramedullary fixation. Arthroplasty options include proximal humerus hemiarthroplasty and reverse total shoulder arthroplasty.
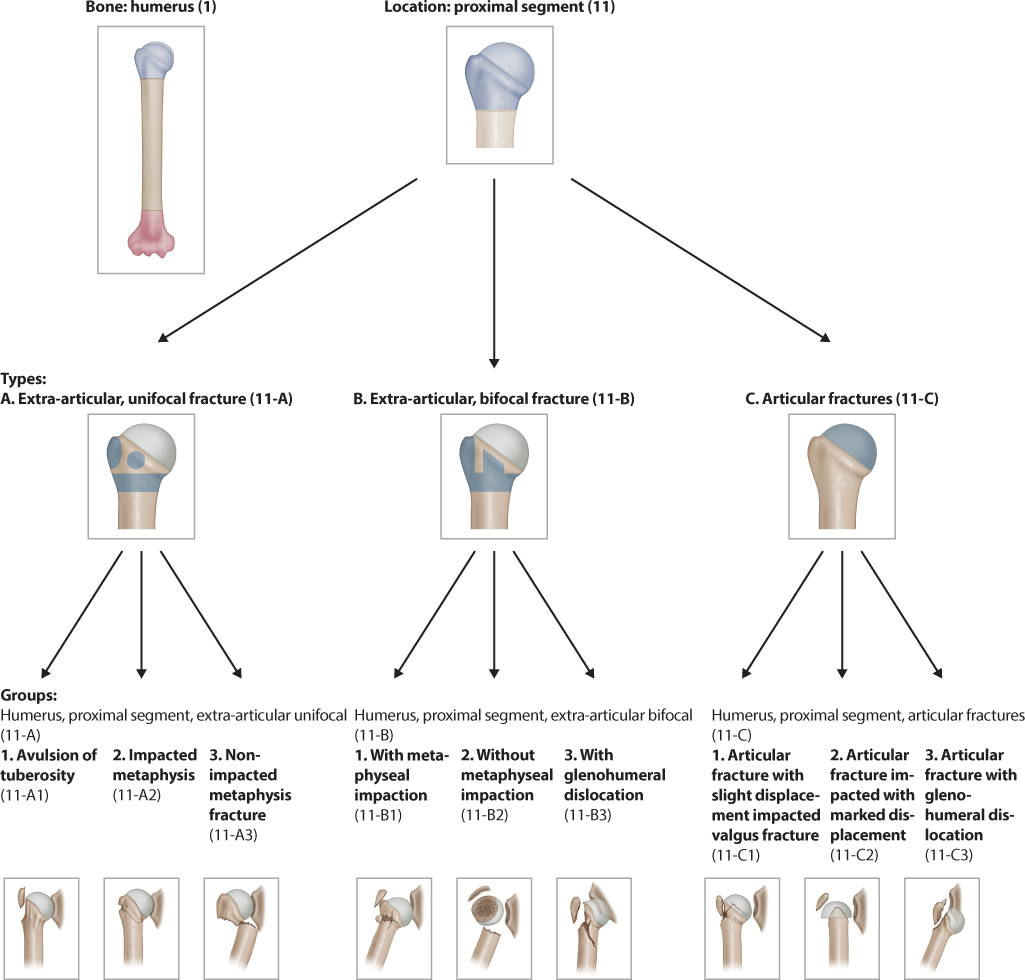
Figure 20.4 The three types and nine groups of the AO classification. The 27 subgroups are not shown. (Reprinted from Marsh JL et al. J Orthop Trauma 2007;21(10 Suppl):S1–133. With permission from RightsLink.)
The proportion of surgically treated patients has increased within the last two decades. Khatib et al.52 reviewed 50,100 patients aged 65 years or older in New York State between 1990 and 2010 with a proximal humeral fracture. The incidence of proximal humeral fractures increased by 28% in the period, but the number of operatively treated fractures increased by more than 40%. The use of locking plates increased from 2001 to 2010 and the use of reverse arthroplasty increased from 2006 to 2010. The use of hemiarthroplasty decreased correspondingly from 2000 to 2010.
Treatment decision
An offer of operative treatment is based on patient age, comorbidity, pre-injury function, fracture anatomy, bone quality, soft tissue injury, the surgeon’s experience and the expectations of the patient.
In a retrospective review of 229 proximal humeral fractures (mean age 77), Okike et al.53 reported factors associated with the decision for operative treatment in patients older than 60. Factors associated with operative treatment included younger age, other orthopaedic injury requiring surgery, AO type C fractures, associated dislocation, translation displacement and management by shoulder or upper extremity specialists compared to trauma specialists.
Medical comorbidity merits careful consideration. Each additional medical comorbidity increases the risk of readmission after surgery by 20%.54 A 90-day readmission rate of 14% was reported among 27,017 surgically treated proximal humeral fractures. Three out of four readmissions were associated with medical diagnoses. Among surgical causes, locking plate osteosynthesis had a significant higher readmission rate (29%) compared to hemiarthroplasty (16%) and reverse prostheses (20%). Mechanical complications after locking plate use accounted for 11% of all readmissions. Infections were also more common in locking plates.55
Surgical or non-surgical treatment in the elderly?
There is limited high level evidence to inform decision making for displaced fractures in elderly patients. A Cochrane review5 included 23 small and heterogeneous randomized trials with a total of 1,238 included patients. Six studies with 270 patients compared surgical and non-surgical treatments. It was concluded that the current evidence is weak, and shows no benefit with surgery. One out of nine surgically treated patients needed additional surgery.
Den Hartog et al.4 included 1096 patients from 33 randomized and non-randomized trials comparing hemiarthroplasty and non-surgical treatment for three- or four-part fractures and found no advantage with surgery.
Kontakis et al.7 included 810 hemiarthroplasties, mainly for four-part fractures, from 16 randomized and non-randomized studies and concluded that there is inadequate evidence to support the effectiveness of primary hemiarthroplasty in the treatment of complex proximal humerus fractures.
Jia et al.6 included 286 three- and four-part fractures from seven randomized trials. They found no clinically important differences between surgical treatment (hemiarthroplasty or internal fixation with tension band or locking plate) and non-surgical treatment.
Nanidis et al.56 included 486 patients from two randomized trials and eight observational studies comparing surgical and non-surgical treatment modalities. They concluded that there was no demonstrable difference in outcomes between fractures managed surgically or non-surgically.
A large randomized clinical trial comparing non-surgical and surgical management of displaced fractures involving the surgical neck has recently been published.57 A total of 250 patients referred for surgical treatment were randomized into non-surgical treatment or surgical treatment. The surgical group was managed according to the surgeon’s preference. Patients were recruited from 33 British orthopaedic departments and all patients followed the same rehabilitation protocol. After 24 months, 215 patients were evaluated with the Oxford Shoulder Score. No difference in outcome between the two groups was found. The rates of complications and secondary surgery were not significantly different, but the cost of surgery was significantly higher.
Timing of surgery
There is no consensus on the optimal time for surgery. Both patient related and potentially modifiable factors influence the time to surgery.
Menendez and Ring58 reported data on 70,000 surgically managed proximal humeral fractures from a national database. Of these, 87% were operated on within 2 days and 13% had surgery after 3 days or more. Increased inpatient morbidity was found after delayed surgery, even when comorbidities and fracture complexity were controlled for. Late surgery was associated with inpatient adverse events (odds ratio 2.1) and prolonged postoperative stay (odds ratio 1.7). In the late surgery group, 57% were discharged to rehabilitation or skilled nursing facility compared to 28% in the early surgery group. Weekend admission was the most common reason for delay in surgery caused by unavailability of the surgeon or operating room facilities.
Outcome assessment with the Constant score in the elderly
The most commonly used outcome assessment instrument in studies of proximal humeral fractures is the Constant–Murley Shoulder score.59,60 and 61 It is an observer administrated shoulder specific outcome instrument consisting of four parts: pain (15 points), activities of daily living (20 points), range of motion (40 points) and strength (25 points). The maximum score is 100 points indicating a shoulder with no disability.
Several problems in the use of the Constant score in the elderly should be mentioned. First, the Constant score can be non-adjusted, age- and sex-adjusted or compared to the opposite shoulder. In several studies it is not clear which version is used. Comparison across studies is therefore problematic. Second, the Constant score decreases with age. Better strength and range of motion is expected in younger patients and the non-adjusted Constant score will therefore underestimate outcome in the elderly. Third, strength cannot be assessed in patients with less than 90 degrees of abduction. This means a subtraction of 25 points from the total Constant score plus the points withdrawn due to the impaired mobility. A satisfied elderly patient with a pain-free shoulder but less than 90 degrees of abduction may therefore have a misleading poor Constant score.
NON-SURGICAL TREATMENT
Only few studies have systematically collected data on outcome after non-surgical treatment of different fracture patterns.
In a systematic review Iyengar et al.62 reported data from 12 studies covering 650 non-surgically treated fractures. There were 49% minimally displaced, 25% two-part, 21% three-part and 5% four-part displaced fractures. Mean age was 65 years and the mean follow-up time was 46 months. Radiographically, healing was obtained in 98% but 13% had complications. Only 2% developed avascular necrosis of the humeral head. The mean Constant score was 74.
Court-Brown et al.63 reported outcome after non-surgical treatment of 125 AO B1.1 fractures followed for 1 year. This fracture pattern represents about 15% of all proximal humeral fractures and appears as minimally displaced fractures, two-part greater tuberosity fractures, two-part surgical neck fractures or three-part fracture fractures (Figure 20.5) within the Neer classification (Figure 20.3). Mean age was 71 years and 81% of the patients reported a good to excellent result after non-surgical treatment with a mean Constant score of 72 overall and 67 in patients aged 80–89. The outcome depended on age and displacement of the fractures, but generally B1.1 fractures can be managed non-surgically.
Hanson et al.64 prospectively followed 160 non-surgically treated fractures. There were 75 minimally displaced, 60 two-part, 23 three-part and 2 four-part fractures according to the Neer classification, and 85 type A, 71 type B and 4 type C according to the AO classification. Four underwent surgical fixation with locking plates or screws, and five had arthroscopic subacromial decompression because of impingement. After 1 year, the difference in mean Constant score between the injured and the contralateral shoulder was 8%. The risk for delayed union and non-union was 7%.
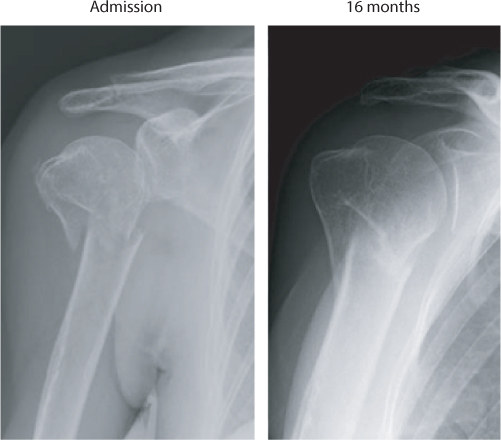
Figure 20.5 A 62-year-old woman with a valgus-impacted fracture (AO B1.1) treated with a sling and early exercises pre-injury function was obtained despite healing with slight angulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








