Proximal forearm fractures and elbow dislocations
INTRODUCTION
Fractures to the proximal forearm account for over 10% of all upper limb fractures, with fractures of the radial head and olecranon the most common fractures occurring around the elbow.1,2 Recent literature has highlighted an increasing incidence of these fractures occurring in the elderly and an association with osteoporosis has been reported.3,4 and 5 The diagnosis of injuries around the elbow and proximal forearm is routinely made using plain radiographs, with computed tomography (CT) reserved for the more complex fractures and fracture-dislocations.
When assessing and managing fractures and fracture-dislocations around the proximal forearm, a key consideration for all patients is to determine whether it is an isolated osseous injury (stable) or one that is associated with significant soft tissue disruption that could predispose to elbow or forearm instability (unstable). An appreciation of the common injury patterns is useful when determining the appropriate management, in order to restore function and stability to the elbow and forearm.6
Non-operative management is the mainstay for isolated non-displaced or minimally displaced fractures of the proximal radius, with a variety of operative interventions available for the more displaced6,7,8,9 and 10 and/or unstable fracture patterns.11,12 and 13 However, there is increasing evidence to support the use of conservative methods in isolated displaced proximal radius and olecranon fractures, particularly in the lower-demand elderly patient.14,15,16 and 17
EPIDEMIOLOGY
Proximal radial fractures are the most common fractures of the elbow, accounting for over 30% of all elbow fractures and over 50% of all proximal forearm fractures.1 The literature on the epidemiology of proximal ulna fractures is sparse, despite accounting for 10–20% of all elbow fractures.6,18 Over 90% of proximal forearm fractures are simple isolated stable injuries that are not associated with an elbow dislocation, forearm instability or another fracture around the elbow.19,20,21,22 and 23 With the subcutaneous location of the proximal ulna, open olecranon fractures are more common than for fractures of the proximal radius.24
The literature quotes a fairly consistent incidence for radial head fractures of 25–35 per 100,000 adult individuals per year,23,25 with the incidence of olecranon fractures quoted as 11–12 per 100,000 adult individuals per year.5,8 An equal gender ratio is reported for both injuries, with the mean age at the time of fracture ranging from 39 to 48 years for proximal radial fractures and almost 60 years for proximal ulna fractures, with figures noted to have increased for both fracture types over the past decade.3,5,18,23,26
A recent study from Edinburgh analyzing 285 radial head and neck fractures over a 1-year period found a significantly lower mean age at the time of injury for males, with the incidence of radial head fractures fitting a type D fracture distribution curve (unimodal young male, bimodal female).3 Radial neck fractures fit a type A distribution (unimodal young male, unimodal older female) with the peak incidence in women more than 80 years of age and the peak incidence in men less than 20 years of age. Kaas et al. performed a retrospective case–control study that compared the peripheral bone mineral density of 35 women ≥50 years of age with a radial head fracture to 57 matched controls and found that the patients who sustained a radial head fracture had an increased risk of osteoporosis (odds ratio 3.4). These two studies have suggested that a proportion of radial head fractures are low energy fragility fractures associated with osteoporosis.23,27
Earlier literature analyzing the management of olecranon fractures originally reported a mean age of approximately 45 years.6,10,28 In a recent prospective epidemiological study of 78 proximal ulna fractures, the reported mean age was 57 years, with the mean age in females (62 vs 51 years) significantly higher and injuries commonly occurring following a low energy fall.5 This study found a type F fracture distribution (unimodal older male, unimodal older female), with an increasing incidence after the seventh decade (Figure 24.1).
This recent literature has led some to advocate that further investigation with DEXA scanning is potentially indicated in post-menopausal women who present with these injuries, as certain proximal forearm fractures may be an ‘index fracture’ for poor bone quality.23,27 Early intervention with appropriate preventative therapy may reduce the risk of future fragility fractures in this patient group. Secondly, given the increasing incidence with age, it has been suggested that further work is needed to investigate the role of non-operative management for simple displaced fractures of the proximal forearm, particular in lower demand elderly patients.
Mechanism of injury
Proximal forearm fractures most commonly occur through either direct or indirect trauma to the elbow following a fall from standing height.1,8,29 A fall from standing height is found in almost 60% of proximal radial fractures and over two-thirds of proximal ulna fractures.3,5 Higher energy mechanisms include a fall from height and sports injuries, which are more frequent in men.23
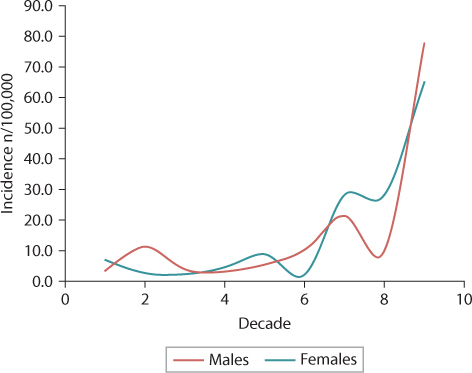
Figure 24.1 The incidence of olecranon fractures, categorized by age and gender.
Anatomical studies have found that fractures of the olecranon are thought to occur when the elbow is flexed at about 90 degrees, with fractures of the radial head and coronoid occurring at less than 80 degrees of flexion.30 Fractures of the radial head occur when an axial load, often with a valgus type force, impacts the radial head into the capitellum.30,31 A study using quantitative 3D CT analysis of Mason type 2 fractures determined that the most common location for injury was the anterolateral quadrant with the forearm in neutral rotation.32
A direct blow to the elbow will commonly lead to an injury of the proximal ulna given the subcutaneous location. This leads to impaction of the proximal ulna into the distal humerus resulting in a more comminuted fracture pattern, particularly in the elderly.7,33,34 Conversely, an indirect traction injury can occur with forceful contraction of the triceps, e.g. following a fall on to the outstretched hand, leading to a short oblique or transverse fracture of the olecranon.7,33,34 With either mechanism, the complexity and displacement is determined by the force of the injury, the pre-existing bone quality of the patient, disruption of the triceps aponeurosis and the force of the triceps contraction.30,35
CLASSIFICATION
AO/OTA classification
The AO/OTA classification combines proximal forearm fractures under one classification system,36,37 with type A fractures extra-articular of either the radius or ulna, type B fractures intra-articular of the radius or ulna and type C fractures intra-articular of both bones. The implementation of this classification in the clinical setting is questioned due to complexity and reproducibility, with recent studies concluding the interobserver reliability to be poor to fair and the intraobserver reliability to be poor.38,39 It is felt better suited for the research setting.
There have been studies that have demonstrated an association between the AO/OTA classification and the outcome of proximal radial fractures.40,41 and 42 Ring et al. reported that more than three fragments of comminution (21-B2.3 type injury) had a significantly increased risk of early fixation failure, non-union and loss of forearm rotation following open reduction internal fixation (ORIF).40
Radial head fractures
MASON CLASSIFICATION
The original Mason classification classified marginal and non-displaced fractures of the radial head as type 1 and displaced partial fractures as type 2, although the qualitative involvement of the head or displacement were not quantified (Table 24.1 and Figure 24.2).43 The modified Broberg and Morrey classification suggested that a type 2 fracture involved more than 30% of the articular surface and was more than 2 mm displaced, which was not based on data and has been reported to have moderate reliability.38,39,44,45 and 46 Some have suggested the inclusion of neck fractures and the Mason type 4 fracture (associated elbow dislocation) is not helpful,35 although there is epidemiological data to suggest neck fractures are predominantly Mason type 1 injuries.3 The Hotchkiss modification is based on clinical parameters such as mechanical block to forearm rotation and the ability to perform ORIF of the fracture.47 The main issue with this is the subjective nature of determining a true block to forearm rotation and which fractures are suitable for ORIF.
The clinical value of the Mason classification is questioned by some as it does not reliably predict the management or prognosis of the fracture. Furthermore, systematic review and meta-analysis are felt to be limited due to the wide variety of modifications used and the limited inter- and intraobserver reliability.48 In a randomized study of 85 orthopaedic surgeons asked to classify 12 radial head fractures using either radiographs and 2D CT, or radiographs and 3D CT, the authors reported that even 3D CT did not significantly improve the interobserver agreement of the Broberg and Morrey modification of the Mason classification.49
Table 24.1 Description and reliability of the original Mason classification and the three modifications,38,39,45,46 with reliability data from studies using plain radiograph interpretation
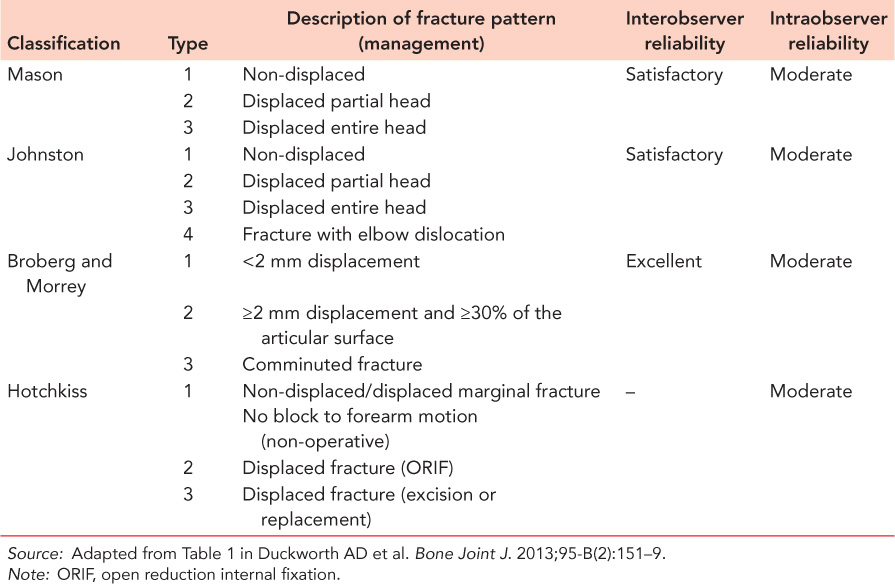
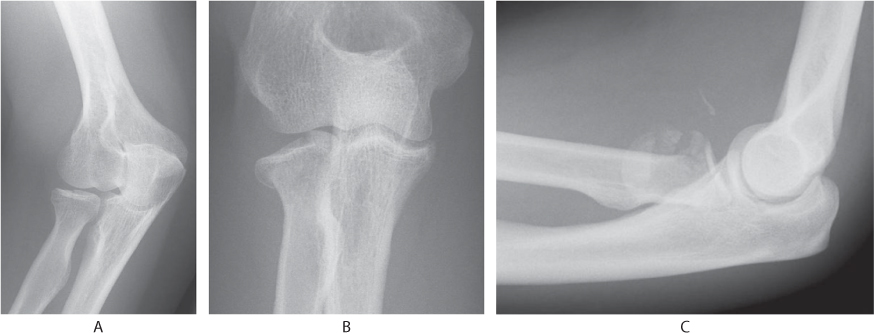
Figure 24.2 Radiographs of the elbow demonstrating Mason type 1 (anteroposterior [AP] view) (a), type 2 (AP view) (b) and type 3 (lateral view) (c) fractures.
STABLE VERSUS UNSTABLE INJURIES
For injuries involving a fracture of the radial head, some have suggested that the injury patterns should be considered as stable or unstable50,51:
Stable isolated radial head fractures are non-displaced or minimally displaced fractures where restoration of elbow and forearm motion is the primary goal of management. Clinically relevant associated injuries are not found, the radiocapitellar contact is preserved and elbow or forearm instability is absent.
Unstable fractures are often part of a more complex injury pattern involving associated osseous and/or ligamentous disruption. In this situation the contact between the radial head and capitellum is often essential to the alignment and stability of the elbow and/or forearm.51,52 and 53 Rineer and colleagues22 defined unstable fractures as loss of cortical contact of at least one fracture fragment with a gap on radiographs, which they reported in 100% of whole head fractures (Mason type 3).
Proximal ulna fractures
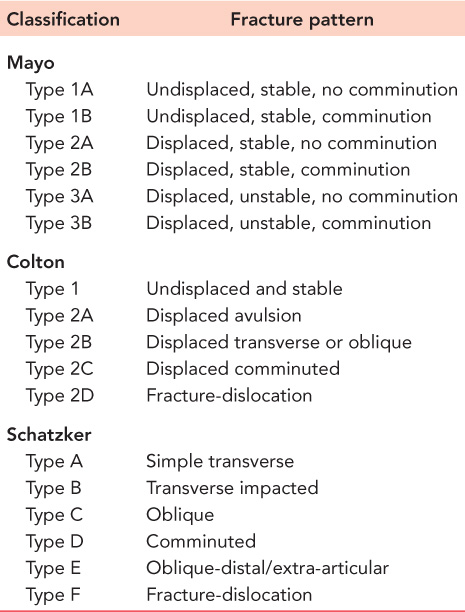
Despite an array of classification systems, the most commonly employed for olecranon fractures is the Mayo classification that incorporates displacement, instability and comminution (Table 24.2 and Figure 24.3).54 Karlsson et al. found in a study of 315 olecranon fractures that 13% were non-displaced (routinely defined as <2 mm articular displacement) and 22% were comminuted.8 Recent data would suggest that up to 85% of all olecranon fractures are displaced stable injuries (Mayo type 2).5,34,55 Alternate classification systems are summarized in Table 24.2. The Schatzker and Mayo classifications have been found to be prognostic of outcome, with instability and fracture configuration (oblique and comminuted) associated with a poorer result.6
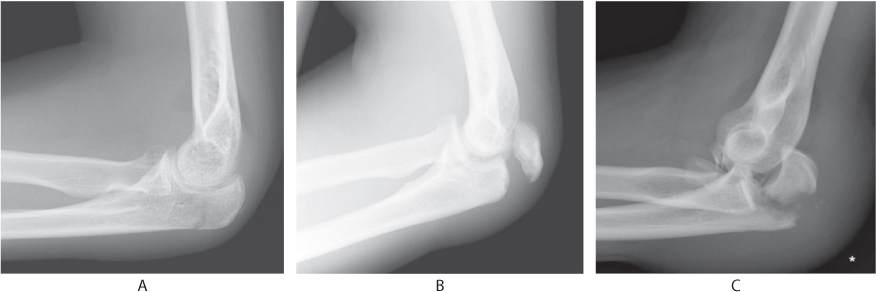
Figure 24.3 Lateral radiographs of the elbow demonstrating Mayo type 1 (a), type 2 (b) and type 3 (c) fractures.
The Regan–Morrey classification is used for fractures of the coronoid.56 Type 1 fractures are defined as an avulsion or tip fracture. Type 2 fractures involve less than or equal to 50% of the coronoid height, with type 3 fractures being greater than 50% of the coronoid height. A recent epidemiological study from Edinburgh reported that only 27% of all coronoid fractures were isolated type 1 fractures, with 73% occurring in association with another significant fracture and/or soft tissue injury.5
Table 24.2 The Colton and Schatzker classification systems for olecranon fractures
Anatomical considerations
The elbow joint is an intrinsically stable complex hinge joint. There are two osseous stabilizing columns, the radiocapitellar and ulnohumeral articulations, which are reinforced by the soft tissue capsuloligamentous attachments.35,57,58 Along with the ulnohumeral articulation (sagittal translation), the medial (valgus stress) and lateral (varus stress) collateral ligament complexes act as the primary stabilizers of the elbow.57,58,59 and 60 Secondary stabilizers include the flexor and extensor muscles that cross the joint, the anterior joint capsule and the radial head.57,58 and 59 These provide stability by limiting posterior translation, as well as rotational and angular stresses, with the radial head a key contributor.54,61,62,63 and 64
These is now a strong appreciation for the role of the radial head, in particular radiocapitellar contact, and the coronoid for stable elbow and forearm motion.54,57,65,66 and 67 This concept is essential to consider in all patients, including the elderly, when determining the appropriate management options for all injury patterns involving a fracture of the radial head.51
OPERATIVE ANATOMY
For fractures of the radial head, the Kocher exposure utilizes the posterolateral interval between the extensor carpi ulnaris (ECU) and anconeus, and is the most utilized operative approach for fractures of the radial head (Figure 24.4).35 The vast majority of injuries can be dealt with using this method as it provides good access, particularly given the auto dissection of some of the capsuloligamentous structures that is associated with proximal radius fractures requiring operative management.40,68,69 For this approach it is best to use the posterior margin of the ECU when dissecting through the joint capsule and the annular ligament, while also protecting the lateral ligamentous complex (if not damaged) and avoiding posterior elevation of the anconeus.35,58 The posterior interosseous nerve (PIN), as it passes around the radial neck, is protected by pronating the forearm.70
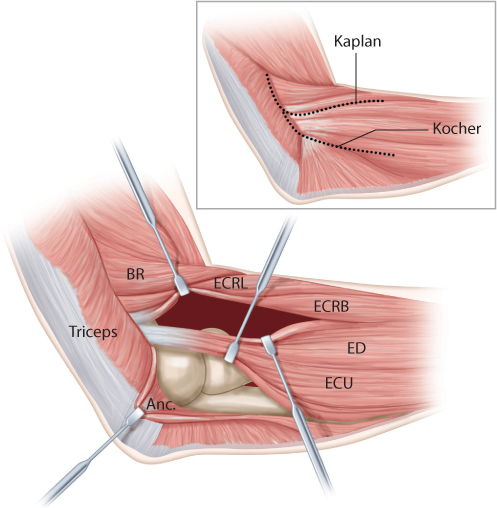
Figure 24.4 The Kocher and Kaplan approaches to the elbow. BR, brachioradialis; ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus; ECU, extensor carpi ulnaris; ED, extensor digitorum. (Adapted from Bell S. Current Orthopaedics. 2008;2(2):90–103)
A more anterior approach is preferred by some surgeons, which involves either splitting the extensor digitorum communis (EDC) or passing between the EDC and the extensor carpi radialis brevis (ECRB) interval (Figure 24.4).35,47 It is important in this approach to stay anterior to the anteroposterior midpoint of the capitellum. The perceived advantages to this method are an improved exposure to the coronoid when needed, as well as increased protection for the lateral collateral ligament (LCL). However, the LCL is often only intact when undertaking ORIF of isolated partial radial head fractures, which in all patients, including the elderly, is of debatable benefit over non-operative management.
The approach to the olecranon and proximal ulna often utilizes a posterior longitudinal midline skin incision to allow adequate exposure of the fracture site, with length variable and dependant on the type of fracture and the type of hardware being used.35 The incision commonly starts proximal to the olecranon and extends over the prominence, continuing distally along the subcutaneous ulna border for usually 3–4 cm past the midpoint of the olecranon.34,71 A direct midline incision may result in reduced subcutaneous nerve damage,72 but some surgeons prefer to pass over the medial border of the olecranon to aid with dissecting out the ulnar nerve when required.35 However, there is no clear indication to dissect out or transpose the ulna nerve in the majority of cases and it can be simply identified with palpation alone.34,71 Full-thickness subperiosteal dissection is performed as necessary to identify the fracture site and the proximal ulna, with anconeus elevated as required from the lateral aspect of the ulna. The collateral ligaments should be preserved throughout.
The operative approach for unstable complex fractures and fracture-dislocation is often aided by the significant soft tissue disruption associated with these injuries. Avulsion of the origins of the LCL and EDC from the lateral epicondyle is often found, with a small rent in the fascia indicating the interval to be used. These structures are mobilized distally, providing good exposure to the radial head and ulnohumeral joint. Fractures associated with a fracture of the proximal ulna can often be addressed through the posterior rent in the muscle by recreating the deformity. An alternative is the Wrightington approach, which involves elevating the anconeus from the proximal ulna and an osteotomy to remove the insertion of the LCL complex at the crista supinatoris.73
CLINICAL ASSESSMENT
Patients present after direct or indirect trauma to the elbow, often following a fall from standing height.1,8,29 Elbow pain (distension of the joint capsule secondary to haemoarthrosis), associated swelling and point tenderness over the proximal forearm are found, often with a reduced range of movement in all directions. The patient will likely be unable to actively extend the elbow and a discontinuity in the extensor mechanism needs to be assessed for. Careful assessment of the skin is necessary to exclude a possible open fracture, particularly in the elderly patient who has sustained direct trauma to the elbow. Distal neurovascular status should always be assessed and documented.
For a fracture of the radial head in particular, an initial and repeated assessment of the arc of motion, forearm rotation, as well as elbow and forearm stability, is often required. Crepitus can sometimes be felt on forearm rotation and/or a frank block to forearm rotation may occur, although the clinical assessment for a bony block to forearm rotation is neither accurate nor reliable as it is very difficult to distinguish a true block to motion secondary to a displaced fragment, from a reluctance to move the forearm secondary to pain. Some authors suggest aspiration of the haemarthrosis to relieve pain and determine if there is a mechanical block to motion that may merit operative treatment.74,75,76,77 and 78
When a proximal forearm fracture is associated with a dislocation of the elbow, deformity and complete loss of elbow motion is seen with associated swelling and ecchymosis. Emergent reduction and assessment of the skin and neurovascular status are paramount.35,79,80 and 81 It is important to be vigilant with a high energy injury mechanism (e.g. a fall from a height) and these patients merit careful evaluation as even minimally displaced fractures and apparently isolated fractures on occasion prove to be unstable and part of a more complex injury pattern.23,35,82 Widespread tenderness, swelling and ecchymosis may indicate possible forearm or elbow instability, particularly over the medial collateral ligament complex, interosseous ligament of the forearm, and/or the distal radial ulnar joint (DRUJ). Potential clinical tests that can be helpful, but which are difficult to perform in the trauma setting, are:
Valgus and varus stability with elbow in full extension and at 30 degrees of flexion53,83
Pivot shift test for posterolateral instability60,83,84 and 85
Axial compression test for forearm instability19
Imaging
A standard anteroposterior (AP) and lateral radiograph of the elbow are the primary investigation, preferably before any potential cast is applied, and should identify fractures of the radial head or neck, the distal humerus, the proximal ulna and any associated elbow dislocation. Initial images may be limited due to pain and repeat imaging once immobilized may be required. Further imaging modalities are not routinely required for simple isolated fractures of the proximal forearm. CT imaging can aid with both the diagnosis and preoperative planning for the more complex fractures and fracture-dislocations. This may be of use in the elderly patient where complex comminuted fractures are seen, but this should not delay surgery unduly.
Excluding a radioulnar dissociation or distal injury to the forearm can be difficult and if there is any clinical concern then bilateral posterior-anterior (in neutral rotation) and true lateral radiographs of both wrists should be performed.86,87 and 88 A high index of suspicion is advised with increasing fracture complexity and higher energy injuries.82,89 There is a great deal of debate regarding the amount of radial shortening that is diagnostic of an Essex-Lopresti type lesion.88,90 MRI can be employed when the diagnosis is in doubt, with cadaveric studies reporting a sensitivity ranging from 88% to 93% and specificity of 100%.91,92 Intraoperative testing using the push-pull test following radial head excision can be helpful. This uses axial traction and compression of the hand and wrist, with a >3 mm change in the distance between the radial neck and the capitellum felt to be diagnostic of an interosseous ligament injury.93
ASSOCIATED INJURIES
Up to 90% of radial head fractures are stable isolated non-displaced or minimally displaced fractures of the neck or the anterolateral portion of the radial head (Mason type 1 and 2), with no clinically relevant associated osseous or ligamentous injury.3,25,32 A study analyzing the MRIs of 46 radial head fractures (40 Mason type 1 and 2) found evidence of ligamentous injury in over two-thirds of stable fractures, but this did not influence the short-term outcome in terms of elbow motion or the surgeon reported outcome score.21,94 However, multiple authors have found a clear association between increasing fracture complexity and the rate of associated injuries,23 with the rate in Mason type 3 fractures 100% in some studies.21,23,25,26 It has been suggested that these injuries often fit one of the following unstable injury patterns23,51,95:
Radial head fracture with posterior dislocation of the elbow (modified Mason type 4)44,96
Radial head fracture with complete medial collateral ligament (MCL) rupture or capitellum fracture
Proximal ulna fracture with radial head fracture (Monteggia variants)97,98 and 99
Terrible triad injury: radial head fracture, posterior dislocation of the elbow, coronoid fracture67,96
Radioulnar dissociation (Essex-Lopresti variants): radial head fracture plus rupture of the interosseous ligament and rupture of the triangular fibrocartilage complex (TFCC).100,101
Associated injuries of the proximal ulna are often variable and need to be assessed and managed on an individual basis. Fractures of the radial head, coronoid, distal humerus and the Monteggia fracture-dislocation (and variants) are seen. Unlike anterior olecranon fracture-dislocations, posterior fracture-dislocations are often associated with radial head and coronoid fractures, as well as an LCL complex injury.99,102
Although the average age of patients with more complex injuries is often reported in the literature as being higher than those with simple isolated fractures, no significant association has been found.3,23 For elderly patients, it is possible to find what would appear to be an unstable displaced and/or comminuted fracture of the radial head, but with no elbow dislocation or proximal ulna fracture. It is essential in these cases to consider these as complex unstable injuries until confirmed otherwise.35
TREATMENT
In the elderly patient the aims of treatment for all proximal forearm fractures are to attain a functional and stable elbow and forearm, with minimal associated complications. The management decision should consider the clinical assessment, the fracture complexity and associated injuries, and most importantly the baseline functional status and pre-existing medical comorbidities of the patient. It is also important to consider bone quality, as well as the surgical risks of any proposed surgery. Treatment options include non-operative, ORIF, fracture excision and replacement.
Non-operative
RADIAL HEAD FRACTURES
The vast majority of radial head fractures are isolated stable injuries where non-operative management produces a good or excellent patient reported outcome, with the reported rates of residual pain, stiffness, symptomatic arthritis and re-intervention very low.14,48,103,104 For elderly patients with an isolated Mason type 1 or type 2 radial head injury, the only clear indication for surgery would be a proven mechanical block to forearm rotation, which is rare.47,48,105,106
In a long-term prospective study of 100 (mean age of 46 years; range 17–79 years) stable isolated radial head fractures (57 Mason type 1, 43 Mason type 2) managed with primary non-operative intervention, 92% of patients were satisfied and the median satisfaction score was 10/10 at a mean of 10 years post injury. The mean Disabilities of Arm, Shoulder and Hand (DASH) score was 5.8, 14% of patients reported stiffness and 24% some degree of pain. Only 2% of patients required subsequent surgery for persistent symptoms associated with the original fracture. Although this study reported a worse DASH score in older patients and those with multiple comorbidities, this is not unexpected given the inevitable decline in function with age that is detected in most patient reported outcome scores and has been reported for other injuries.107
These findings are supported by data from Sweden. Herbertsson et al. analyzed 32 Mason type 1 fractures at a mean of 21 years after injury and reported full motion and only three patients with occasional pain.104 In another study from this group, Akesson et al. analyzed 49 patients with an isolated Broberg and Morrey Mason type 2 fracture at a mean of 19 years post injury and reported 82% had no pain, although 12% underwent delayed radial head excision at 4–6 months after injury for unclear reasons.48
All studies in this area seem to highlight that the predominant adverse outcome following the non-operative management of these injuries is persistent elbow stiffness and all patients should be counselled regarding this.
PROXIMAL ULNA FRACTURES
The general consensus is that Mayo type 1 stable undisplaced fractures of the olecranon can be managed effectively with non-operative intervention (Table 24.3), with the generally agreed criteria for displacement being <2 mm of articular displacement.7,29
With conflicting literature regarding the outcome following surgery for displaced olecranon fractures in elderly patients108,109 and the rising number of older patients sustaining these injuries, the role of non-operative management has been investigated (Table 24.4). There is now a growing body of evidence supporting the role of non-operative treatment for displaced olecranon fractures in lower demand elderly patients where comorbidities, pre-injury functional status, bone quality and potential complications following surgery need to be considered.5
A recent study from Edinburgh reported the outcome of 43 patients with a mean age of 76 years who sustained a displaced fracture of the olecranon that was managed with primary non-operative intervention.17 At a mean of 4 months following injury the mean Broberg and Morrey score was good, with 72% achieving an excellent or good short-term outcome and no patients requiring further surgery for a symptomatic non-union (Figure 24.5). The long-term outcome was assessed at a mean of 6 years in the 23 patients who were still alive and it was found that overall patient satisfaction was 91% and the mean DASH score was 2.9. Eighty-three per cent of patients reported no subjective weakness of extensor strength and 78% developed a functional non-union.
Table 24.3 Treatment options for olecranon fractures categorized by the Mayo classification
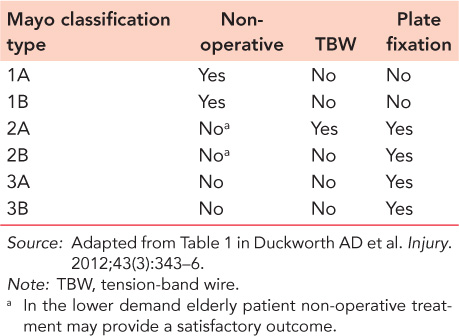
Table 24.4 Current literature on the non-operative management of isolated displaced olecranon fractures
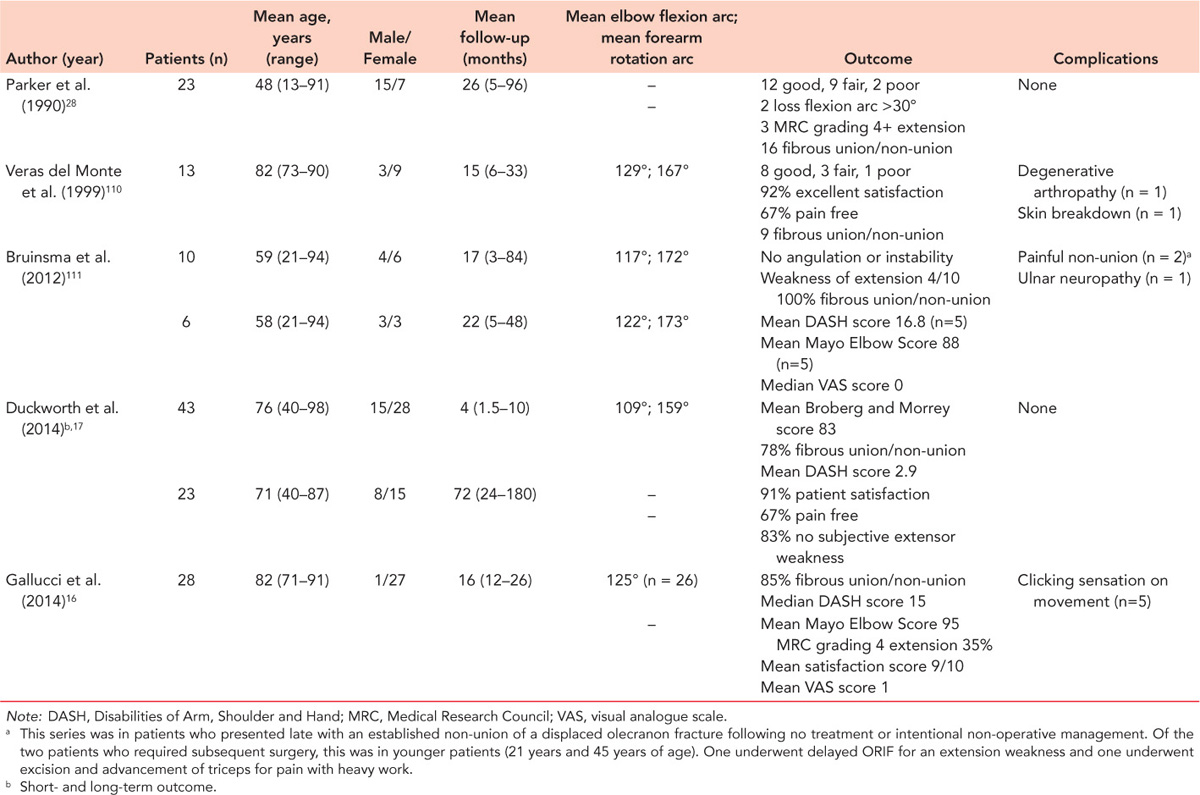
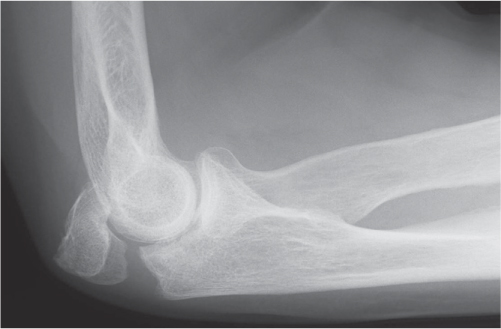
Figure 24.5 An established functional painless non-union at 6 months post injury in a 77-year-old female patient.
Gallucci et al. reported on a retrospective short-term case series of 28 elderly patients (mean age 82 years, all >70 years) treated non-operatively with an above elbow cast for an average of 5 days for a displaced olecranon fracture, which was defined as any articular displacement, or displacement of the posterior cortex of >5 mm.16 Ten (36%) fractures were comminuted (Mayo type 2B) with articular displacement ranging from 0 to 23 mm (mean 12 mm), but with no fractures open or associated with a dislocation. In 28 patients at a mean of 16 months post injury the mean satisfaction score was 9, the median DASH score was 15 and the mean MEPI score was 95, with 22 outcomes rated excellent and 6 good. Nine (35%) patients had loss of extension strength (Medical Research Council [MRC] grade 4) and 22 (85%) developed a radiographic non-union.
Similar positive short-term results (Table 24.4) have been reported in: (1) an older series of 23 patients with ages ranging from 13 to 91 years,28 (2) in a case series of 13 elderly patients with a mean age of over 80 years110 and (3) in a series of 10 patients with a mean age of 59 years who presented with a non-union of a displaced olecranon fracture at a mean of 17 months post injury.111
The literature in this area would suggest the predominant adverse outcome following the non-operative management of displaced olecranon fractures is a weakness to elbow extension strength, but which does not appear to markedly affect the patient reported outcome. The only caveat is the rare subtle unstable injury, which may not be apparent on initial radiographs.
COMPLEX ELBOW FRACTURES AND FRACTURE DISLOCATIONS
For some elderly patients non-operative management for complex fractures of the proximal forearm can be used if it is felt elbow and forearm stability can be maintained without surgery and the patient is willing to accept the possible complications that can occur44,112,113,114 and 115 which include recurrent instability, pain and loss of function. The type of injury suitable would include radial head fractures associated with a dislocation of the elbow alone, and/or a fracture of the coronoid. Criteria that are commonly used include: (1) a concentric elbow joint on post-reduction AP and lateral elbow radiographs, (2) a partial radial head fracture that does not block forearm rotation, (3) a Regan-Morrey type 1 or 2 fracture of the coronoid and (4) a stable active flexion arc from a minimum of 30 degrees of extension within the first 7–10 days of injury.114,116,117
Broberg and Morrey reported the long-term results of cast immobilization with or without acute radial head resection in patients who sustained a Broberg and Morrey type 2 (n = 7) or type 3 (n = 17) fracture of the radial head fracture associated with a dislocation of the elbow.44 There were associated injuries in 42% (n = 10) of patients, including six coronoid fractures. The authors reported that in patients managed with primary conservative treatment alone, delayed radial head resection was required to improve forearm rotation in those with a Mason type 3 fracture (6/7 patients).
Chan et al. reported a retrospective analysis at a mean of 3 years post injury in 11 patients (mean age 51 years, range 26–76) with a terrible triad injury of the elbow that fit the criteria described above and were managed non-operatively.116 Three patients had a Mason type 1 fracture and eight were a Mason type 2 (displacement range 2–8 mm), with all coronoid fractures a Regan–Morrey type 2. At final follow-up the mean DASH score was 8 and the mean Mayo Elbow Score was 94. Two patients underwent further surgery – one for surgical stabilization for early recurrent instability and a second for arthroscopic debridement for heterotopic ossification (HO).
Preferred technique
For radial head fractures we would recommend a collar and cuff for comfort, and early active mobilization. We do not routinely undertake aspiration of the joint. The methods of non-operative management have been investigated in patients of all ages. Early mobilization appears to be safe and effective for stable isolated radial head fractures. In a prospective randomized trial of 60 patients comparing immediate active mobilization or 5 days of immobilization followed by active mobilization, the authors reported no differences after the first week of injury and excellent outcomes in both groups.118 A recent three-arm prospective randomized trial of 180 isolated stable radial head fractures compared immediate mobilization, a sling for 2 days and then active mobilization, and a cast for 1 week prior to mobilization.119 The authors reported that immediate mobilization was safe and effective, but with a delay of 2 days prior to mobilization potentially advantageous.
For non-displaced olecranon fractures we would recommend splinting the elbow in 45–90 degrees of flexion for approximately 3 weeks, followed by supervised mobilization.7,35 Check radiographs within the first couple of weeks of injury to ensure there is no displacement of the fracture. From the studies discussed above on the non-operative management of displaced olecranon fractures, the methods of immobilization range from a collar and cuff with early mobilization to an above elbow cast for 4–6 weeks. In our centre, we would generally use an above elbow cast for 2–3 weeks and then allow the patient to mobilize as they are able. If the patient is not in too much pain, a collar and cuff can be used. It is important to perform an AP and lateral radiograph of the elbow within the first 2 weeks to exclude a subtle unstable injury.
For type 4 radial head fractures or terrible triad injuries, a variety of non-operative protocols are suggested in the literature. In the paper by Chan et al.116 all patients with a terrible triad injury underwent immediate closed reduction and assessment of elbow stability, immobilization and were then reviewed within 1 week of injury for a physical examination and a CT scan of the elbow. Referral to physiotherapy was made within 10 days for protective motion including forearm rotation at 90 degrees of elbow flexion. This protocol is consistent with our approach, although not all patients undergo a CT of the elbow (particularly if there is no associated coronoid fracture) and we do undertake an examination under anaesthesia (EUA) if there is a concern regarding elbow stability or forearm rotation.
ORIF
RADIAL HEAD FRACTURES
Although there are still advocates for ORIF of isolated displaced radial head fractures, in our opinion the role of fixation is diminishing. This is certainly the case in the elderly patient where fixation in osteoporotic bone is challenging. There are some retrospective case series that report good results following ORIF of isolated partially displaced fractures of the radial head, but as has already been discussed, there is a growing body of evidence that a good result would be expected with non-operative management.106,120,121,122,123 and 124
Lindenhovius et al. reported the long-term outcome (mean 22 years) of 16 patients who underwent ORIF for an isolated Mason type 2 fracture and found a complication rate of 31%, a mean DASH score of 12 points and a good or excellent Mayo Elbow Score in 81%.106 Recently, Yoon et al. reported a retrospective comparative mid-term review of 60 patients with an isolated displaced (2–4.9 mm) fracture of the radial head.15 Thirty patients were managed with ORIF (mean follow-up 4.5 years) and 30 patients were treated non-operatively (mean follow-up 3 years). Using a combination of surgeon and patient reported outcome measures, superior outcomes were found in favour of non-operative management according to the Mayo Elbow Score (MES), the SF-12 physical component and overall rate of complications. This study found that patients younger than 60 years in both groups had a poorer outcome according to the MES and the Patient Rated Elbow Evaluation questionnaire.
Preferred technique
In our unit, ORIF is now not routinely used for fractures of the radial head, particularly in the elderly patient. If considering fixation, it is important to consider the 90 degree arc (‘safe zone’) of the radial head that is used to place implants safely so as to avoid impingement at the proximal radioulnar joint. A variety of methods are used for identifying the non-articular part of the proximal radioulnar joint on the radial head:
PROXIMAL ULNA FRACTURES
The management of a displaced fracture of the olecranon or proximal ulna aims to restore the articular surface with minimal associated complications (Table 24.3).7,128 The literature would suggest that the risk factors associated with an inferior outcome following surgery are fracture morphology and associated elbow instability and/or fractures.6,129 A recent Cochrane review of 244 olecranon fractures from six randomized controlled trials concluded that further work is needed in this area to determine the optimal surgical management of simple isolated displaced fractures of the olecranon.130
For the stable comminuted displaced fracture (Mayo type 2B) and those fractures associated with other injuries or elbow instability (Mayo type 3), plate fixation is considered to give superior results to tension-band wire (TBW) use.7,55,128,131,132,133,134,135 and 136 For the stable displaced olecranon fracture with minimal or no comminution (Mayo type 2A), although TBW fixation is seen as the gold standard by many and is frequently used, plate fixation is a noted alternative.6,7,8,9 and 10,55,71,132,137 For the Mayo type 2 fracture, it is important to consider whether any form of surgical intervention provides a superior outcome to non-operative management in the elderly lower demand patient.
TBW and plate fixation
There is an increasing body of biomechanical evidence to suggest that plate and intramedullary screw fixation confers greater stability at the fracture site than a TBW construct. Wilson et al. performed a biomechanical comparison of TBW and plate fixation in 20 ulna models with identical transverse fractures of the olecranon.138 They found that the modern pre-contoured location specific plates were significantly better at providing fracture compression, particularly at the articular surface, than the TBW construct. In a more recent study of 12 pairs of simulated olecranon fractures in cadaveric limbs, cyclic loading and assessment of fracture stability following fixation with either a plate or TBW construct demonstrated a median displacement of 0.25 mm for the plate and 1.12 mm for TBW.139 Whether these findings confer an inferior patient reported outcome is unknown.
There are short- and long-term data reporting good functional outcomes following TBW fixation,6,71,140,141 and 142 although none have specifically analyzed the outcome in the elderly. Flinterman et al. reported the long-term patient reported outcome in 41 patients who sustained a simple transverse displaced fracture of the olecranon. The mean age of the patient group was 35 years (18–73). At a mean of 20 years following surgery, the mean DASH score was 10, the mean MES was 98 and the mean elbow flexion arc was 142 degrees. The only predictor of the DASH score was increasing age at the time of surgery.143
The complications documented following TBW fixation are wound breakdown, infection, prominent metalwork, malunion and non-union6,7,71,133,140,144,145 (Figure 24.6). The most common complication is symptomatic metalwork requiring removal, which is best avoided were possible in the elderly patient. Macko et al. reported the highest re-operation rate at 85% in their 5-year retrospective analysis of 20 patients with a range of displaced olecranon fractures,140 with symptomatic K-wire prominence most frequent (80%). Proximal wire migration was found in only 15% (n = 3), skin breakdown in 20% (n = 4) and infection in 5% (n = 1).
There is almost no literature exclusively examining the use of plates for the treatment of type 2A fractures specifically in elderly patients (Figure 24.7). There have been recent retrospective comparative studies of TBW versus plate fixation for both simple and comminuted displaced fractures of the olecranon.146,147 and 148 These have consistently reported comparable functional outcomes, a higher rate of metalwork removal following TBW fixation and increased costs with plate fixation. Although it is perceived that plate fixation is associated with symptomatic prominent metalwork given the location of the plate, the literature would suggest the rates of removal are lower than those for TBW, ranging from 5% to 20%.7,133,134 A recent study by Tarallo et al. compared the outcome of TBW and plate fixation in 78 patients with a Mayo type 2A or 2B fracture.147 At a mean of 33 months no significant differences were found between groups in terms of functional or clinical outcomes but a higher rate of complications and hardware removal were found following TBW: 38% vs 17% for type 2A fractures and 20% vs 6% for type 2B fractures.
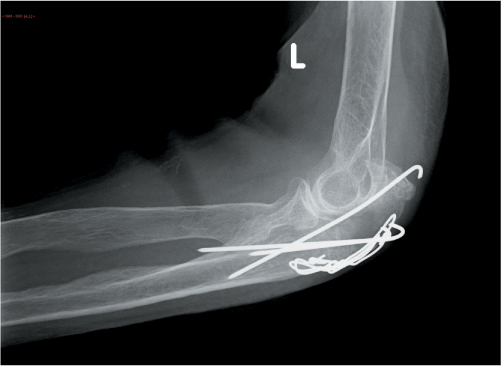
Figure 24.6 A failed TBW fixation at 6 weeks postoperative in a 91-year-old female patient with a stable displaced fracture of the olecranon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








