Polytrauma in the elderly
Risk factors and mechanisms of injury in older polytrauma
Comorbidities in older polytrauma
Patterns of injury and specific associated injuries
Triage of the elderly polytrauma patient
Evaluation and care of elderly polytrauma patients
INTRODUCTION
Trauma, in general, and polytrauma, in particular, are widely recognized as conditions afflicting the young. Consequently, the study of polytraumatized or multiply injured patients has focused historically on young, male adults, commonly considered the population most affected by trauma. More recently, however, there has been recognition that high-energy trauma affects all populations. In fact, approximately 35% of all trauma occurs in individuals over 65 years of age.1,2
The elderly make up the population demographic whose numbers are increasing at the greatest rate. Prior to 2007, at no time in human history did the number of individuals over the age of 65 exceed the number of individuals under the age of 5. Since 2007, however, the number of the elderly in the world’s population has begun to exceed the number of young children. In fact, the global population of elderly individuals (generally considered to be 60+ years of age) is expected to increase from 287 million in 2013 to 417 million by 2050.1
Additionally, older individuals are participating in activities that put them at high risk for sustaining severe injuries that may involve multiple organ systems. The number of older individuals who drive or are passengers in motor vehicles, who ride motorcycles or who engage in other high speed or high-energy activities is increasing. It stands to reason that, given the demographic and behavioural trends, the prevalence of polytrauma in the elderly will increase (Figure 14.1).
When older individuals sustain polytrauma, their outcomes, when compared to a younger population, are generally poorer and result in higher complication and mortality rates. This poses unique challenges to medical, trauma and orthopaedic providers.
EPIDEMIOLOGY
The elderly constitute an increasing proportion of polytraumatized patients. Although recent census reports estimate that people aged 65 and older make up 13–14% of the US population, the 2014 report of the US National Trauma Data Bank indicates that patients aged 65 and older comprise 28% of all reported trauma patients.3 An analysis of the same data reveals that 30% of all polytrauma incidents were in this older age group.4
In 1986, a Swiss study focused attention on polytraumatized elderly patients. In a cohort of 300 patients who sustained polytrauma, defined as either a visceral injury associated with significant fractures or a minimum of two major fractures, 27 (9%) were aged 70 and older.5 Similarly, in 1988, Broos et al. described 416 multiply injured Belgian patients, of whom 49 (12%) were aged 65 and over.6 Before these reports, only a small number of authors in the English literature had written on the topic of polytrauma in the elderly and even fewer had reported on the orthopaedic implications of polytrauma in the elderly.
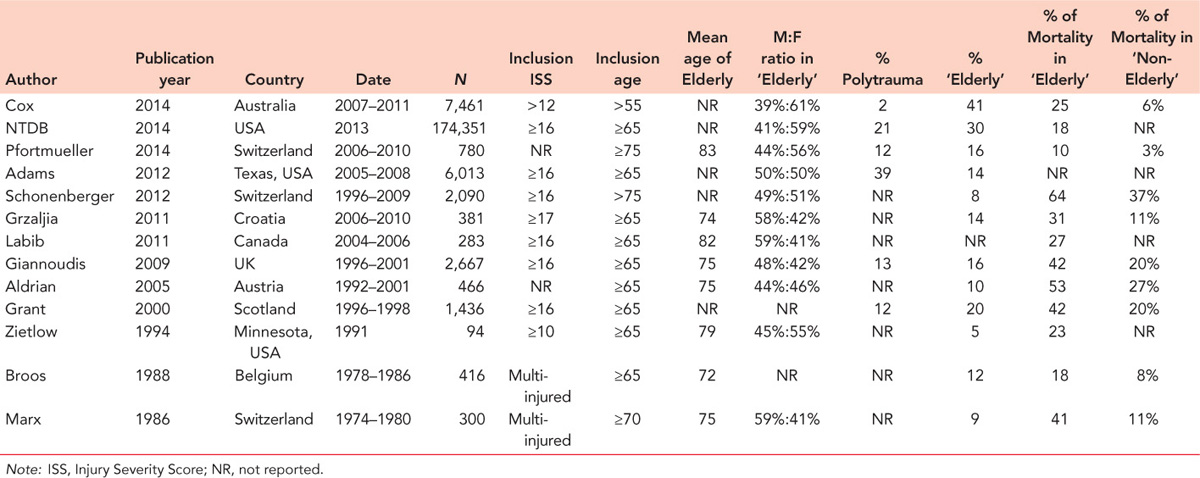
In the nearly three decades since these initial reports, only a limited number of studies have expanded our epidemiological knowledge about these patients. As illustrated in the summary of the literature in Table 14.1, few authors have specifically described older trauma victims as a unique patient cohort that might require specific protocols of care and that could benefit from specific study.4,5,6,7,8,9,10,11,12,13,14,15 and 16 As this summary elucidates, most authors have defined ‘elderly’ or ‘geriatric’ as patients aged 65 and older. Only a few reports have used an older5,8,10 or younger7 definition for the elderly patient.
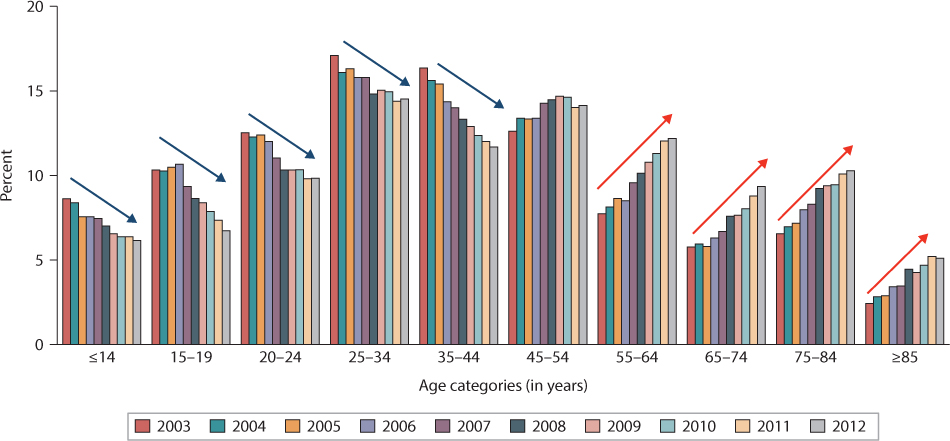
Figure 14.1 A 10-year history of weighted estimates of the incidents of trauma admissions from the US National Trauma Databank illustrate a clear declining trend in trauma admissions in patients aged 44 years and younger, but an increasing trend for all age categories in patients aged 55 and older. (Reprinted from the Committee on Trauma, American College of Surgeons. NTDB Annual Report 2014. Chicago, IL. With permission. The content reproduced from the NTDB remains the full and exclusive copyrighted property of the American College of Surgeons. The American College of Surgeons is not responsible for any claims arising from works based on the original data, text, tables or figures.)
Most reports on trauma in the elderly have employed an inclusion criterion of a minimum Injury Severity Score (ISS) of 10–17 to indicate ‘polytrauma’ or ‘severely’ injured (Table 14.1). One study found that 5% of all trauma patients admitted to a level 1 trauma centre were elderly patients (≥65 years old) with multisystem trauma.16 From these reports, we can see that ‘elderly’ patients comprise 8–30% of reported polytrauma cohorts, with one study from Australia reporting an incidence of 41% of trauma patients with an ISS >12 at 55 years of age or over.7
In a review of the changing characteristics of all trauma patients across the decades, a study of 501 polytraumatized patients found an age increase of 0.75 years for each subsequent year.17 In other words, older age is becoming an increasingly important characteristic of polytrauma patients. A report from the national hospital registries in Spain found similar trends in the decade from 2000 to 2010, when the incidence of all trauma patients under the age of 75 remained stable, but the incidence of trauma patients over the age of 75 increased significantly.18 This trend has also been noted across Europe; in an analysis of a large prospective single centre database from Switzerland from 1996 to 2009, the percentage of patients over 75 years of age increased from 6.5% in years one and two to 11.8% in the final 3 years of the study data.10 Similarly, a US based study from Texas noted a nearly 3% increase in annual elderly admissions to a level 1 trauma centre between 2005 and 2008 (P<0.001),9 further indicating the global phenomena of the increasing elderly polytrauma patient population.
The sexual dimorphism of polytrauma in the elderly occurs at a rate that is neither consistent with the rate of low-energy injury in the elderly nor the rate of high-energy injury in the young. The proportion of male to female elderly polytrauma patients is nearly 50/50, while the proportion of male to female low-energy trauma patients is approximately 25/75. Most reports in younger trauma populations show an approximately 75/25 male to female proportion.9
RISK FACTORS AND MECHANISMS OF INJURY IN OLDER POLYTRAUMA
As in all orthopaedic trauma related events, the greatest predictor of injury is participation in risky activities. Increased independence, increased life expectancy and an expectation of a more active lifestyle are the primary characteristics of elder individuals that predispose them to polytrauma.
Although there has been an increase in the number of elderly polytrauma patients, focused reports indicate that, across the past quarter of a century, mechanisms of injury in this patient population have not changed significantly. Blunt trauma, as opposed to penetrating trauma, is reported as the cause of injury in nearly 99% of all polytrauma in the older adult population.12 However, the elderly are participating in higher energy activities such as motor vehicle usage, motorcycling, climbing or working at heights.
Data from the National Hospital Ambulatory Medical Care Survey show that between 2003 and 2007 there were an average of approximately 240,000 annual visits by elderly individuals (>65 years of age) to US emergency departments for motor vehicle related injuries.19 In fact, motor vehicle collisions are the second most common cause of non-fatal injury in elderly individuals, the most common being falls. Broos et al., when first drawing attention to elderly polytrauma patients in 1993, found that motor vehicle accidents (MVA) and falls were the leading cause of injury, with 57% and 30% of the 126 cases reporting these mechanisms, respectively.20 Interestingly, these authors also determined that, in 44% of these cases, the patient was a pedestrian hit by a motor vehicle. Similarly, in a 1994 study by Zietlow et al., 59% of the multiply injured elderly patients included in the study were injured due to a fall and 36% were due to MVA16 (Figure 14.2).
Table 14.1 Global reporting of the incidence of elderly polytrauma
These same commonalities in mechanism of injury (MOI) hold true globally as well. In a large study from the United Kingdom’s Trauma Audit and Research Network (TARN) database of 438 polytrauma patients aged 65 and older, road traffic accidents were determined to be the MOI in 42%. Falls from a low height were the cause of injury in 31% of older patients but in only 8% of the younger adult trauma population.13 In registry reports from both Scotland (Scottish Trauma Audit Group)15 and Australia,7 MVA were determined to be the predominant cause of injury in older adults, although falls from a low height were found to have a significantly older mean age than other mechanisms.15
Falls are the leading cause of death due to injury in the elderly. Multiple studies have shown that as a result of falls, the elderly sustain injuries of a similar severity to those in younger patients resulting from higher energy mechanisms.21,22 Not surprisingly, in studies that stratify polytrauma patients by age, increasing age correlates with falls as an increasingly more prevalent injury mechanism. One such study found that falls from a low height were the MOI in only 9.7% of adult trauma patients aged 25–49, 19.7% in patients aged 50–75 and 37.3% in patients over the age of 75.10
COMORBIDITIES IN OLDER POLYTRAUMA
Older patients have blunted physiological responses to trauma. Secondary to changes associated with aging and diminished physiological reserve, older patients cannot mount the same type of haemodynamic and metabolic response to trauma as younger patients. Additionally, other factors such as the use of medications that complicate resuscitation of elderly polytrauma patients also challenge their care.
Specific physiological changes that may lead to challenges in the treatment of polytraumatized individuals are listed in Table 14.2. These include decreased renal, hepatic and pulmonary function, impaired cardiovascular reserve, an inability to launch an appropriate physiological response to stress and shock, frailty and dementia. In a study of abstracted data from over 33,000 medical records of trauma patients over the age of 65, hepatic disease, renal disease and cancer, in particular, were shown to contribute to poorer outcome in polytraumatized older patients.23
The elderly may also have deceptively normal vital signs, even when they are hypovolemic and close to shock. A normal adult haemodynamic response to hypovolemic shock, as a result of trauma, is increased heart rate and blood pressure. When elderly trauma patients present with normal heart rate and/or a normal or low blood pressure, they can be misdiagnosed as being either less injured or better resuscitated than they actually are; hypertension is common in the elderly, therefore normal vital signs might indicate hypovolemia. Low volume and hypoperfusion, as a result of trauma in the elderly, are often further complicated by a decreased ability to generate responses to stress, the effect of medications commonly prescribed in the elderly (i.e. beta blockers, ACE inhibitors, steroids) and/or the fact that, when compared to body weight, the elderly have a lower gross blood volume and cardiac output.
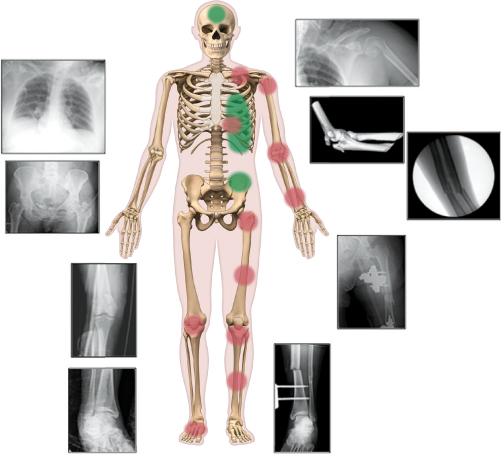
Figure 14.2 A 64-year-old female patient was involved in a head-on motor vehicle collision. The patient sustained subarachnoid haemorrhage, splenic laceration, L rib fractures with pneumothorax, R subtalar fracture dislocation, R patella fracture, L tibia and fibula fracture, L tibial plateau fracture, L femur fracture, L inter-trochanteric hip fracture, L both-bone forearm fracture, open L transolecranon fracture dislocation and L clavicle fracture with L four-part proximal humerus fracture.
Table 14.2 Physiological considerations and comorbidities in older polytrauma patients
Considerations |
|---|
Heart disease and hypertension |
Diabetes |
Chronic obstructive pulmonary disease (steroid treatment: reduced wound healing, clinical adrenal insufficiency) |
Dementia (antipsychotics: effect neurological exam) |
Cancer |
Chronic renal failure |
Hepatic disease |
Medications (beta blockers: masking normal vital signs, under-recognition of tachycardia) (anticoagulation/antiplatelet agents, warfarin, blood thinners, cardiac medications) (polypharmacy) |
Pacemaker |
Also complicating evaluation and management in the setting of trauma in the elderly is the decreased reporting of pain by the elderly, as well as mental status change that can occur as a result of age. These patients may have a history of Alzheimer’s disease, cognitive decline, Parkinson’s disease or a history of cerebrovascular insults that can contribute to difficulty in communication that, in turn, lead to difficulties in diagnosis and treatment. Even mild dementia can be precipitously worsened by trauma, and the delirium that often accompanies stress and trauma in the elderly can make challenging the interpretation of information available in the setting of polytrauma in the elderly.
PATTERNS OF INJURY AND SPECIFIC ASSOCIATED INJURIES
Given the lack of robust investigative focus on elderly polytrauma patients, it is difficult to well characterize common patterns of injury in this patient population. There are, however, important injury types and injury constellations that may guide future study in this area.
In the 1984 report by Oreskovich et al.,24 a review of 100 patients over the age of 70 who were admitted to a metropolitan trauma centre, 80% of the patients were classified as ‘multi-trauma’, having at least two body regions injured. In this cohort, the authors reported that the extremities and pelvis were the most common body regions to be injured and that one-third of the patients had an injury to the thorax or abdomen that required surgery. In 1994, in a similar single centre cohort of 94 subjects, Zietlow et al. found that 57% experienced thorax injury, 56% experienced an extremity fracture and 13% experienced combined abdominal and pelvic injuries. The mean ISS in this cohort was 18. Closed head injury and fractures were cited as the most frequent injuries.16
Two studies that focused specifically on elderly pedestrian trauma reported the increasing occurrence of specific fracture patterns in the elderly when compared to younger victims.1,25,26 Both reports found that the elderly had significantly higher rates of fractures of the pelvis, upper extremities and lower extremities. The elderly patients also had a higher rate of intracranial injuries, but sustained lower rates of hepatic injuries when compared to younger age groups (Figure 14.3). These reports contrast with a 2009 database analysis that compared young and old, severe and multiply injured trauma patients, and found similar anatomic injury distribution regardless of age. These authors reported 63% had serious head injury, 18% serious thoracic or lower limb injury and 9% serious abdominal injury.13 A 2011 report of 283 elderly trauma patients with ISS ≥16 and a mean age of 81.5 years found that rates of injury in this population included: 88.4% traumatic brain injury, 22.8% thoracic injuries (with rib fractures and flail chest the most common), 17% spine injuries and 8%, 7.6% and 6.5% long bone, pelvic and hip fractures, respectively.12 Most recently, a single centre report that included 154 older polytrauma patients with orthopaedic injuries found that spine fractures followed by pelvic/acetabulum injuries were most common. These authors excluded all low-energy mechanisms and the most severely injured patients with an Abbreviated Injury Scale (AIS) ≥4, which could have skewed the results.27
Pelvic and acetabular fractures that occur as a result of trauma in elderly patients demonstrate characteristics that differ from those in younger patients. Lateral compression pelvic factures are the most common pelvic ring injury in the elderly and, when they occur, result in greater blood loss and need for transfusion, longer length of stay and higher mortality than those in younger patients.28 Anterior column, both-column, and anterior column with posterior hemitransverse acetabular fractures are also more common in the elderly.1
Clavicle and/or rib fractures that occur in the elderly as a result of blunt trauma also demonstrate increased morbidity and mortality when compared with the same injuries in younger patients. In an analysis of 277 patients >65 years of age, the morbidity and mortality of blunt chest trauma was such that, for each additional rib fracture, mortality increased by 19% and the risk of pneumonia increased by 27%.29 A study by Keller et al. of high-energy skeletal trauma in the elderly, found, in addition to a high association between pelvic, spine injuries with increased mortality, an increase in mortality associated with clavicle fracture.30
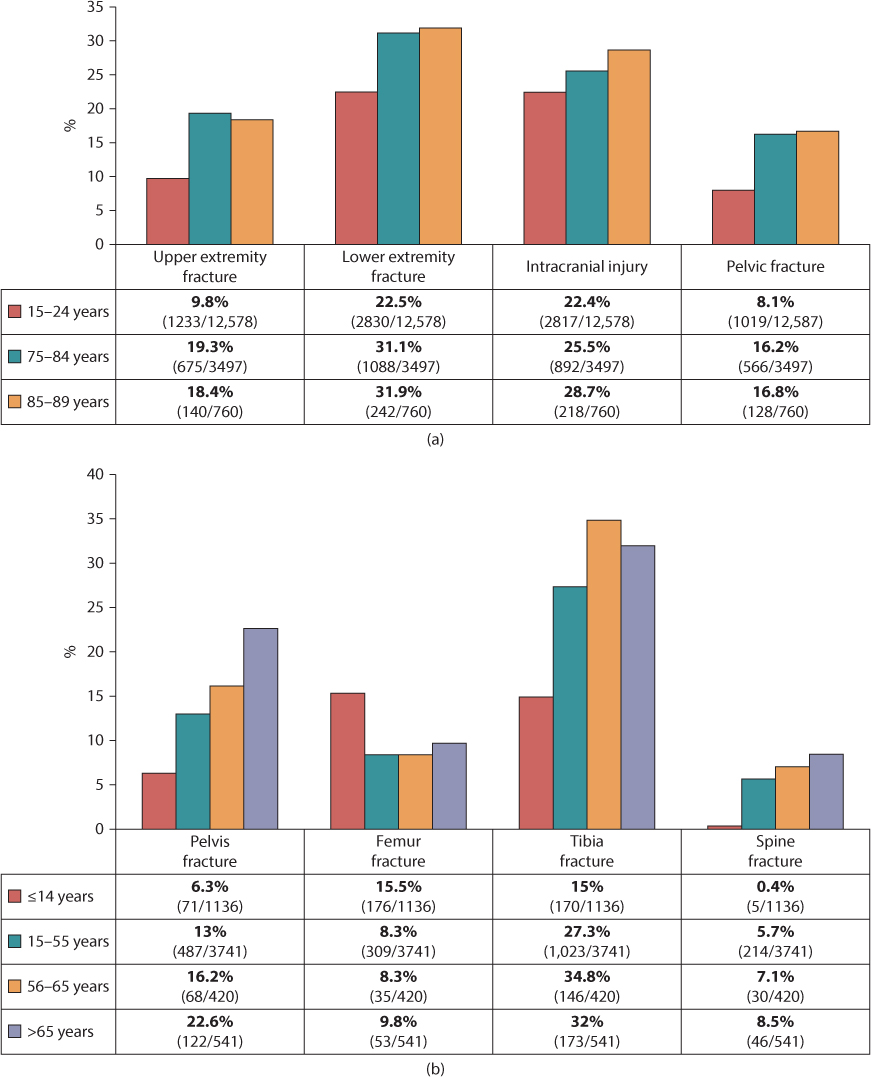
Figure 14.3 (a) Chart showing data from the study by Siram et al.25 which illustrates the rate of pedestrian trauma by age group and location of injury. (b) Chart showing data from the study by Demetriades et al.26 which illustrates the rate of pedestrian trauma by age group and location of injury. (Reprinted from Switzer JA, Gammon SR. J Bone Joint Surg Am. 2012;94(23):2195–2204. With permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








