Outcome after fracture
Stakeholders, goals and prioritized outcomes
Inter-relationship of outcomes
Health-related quality of life
INTRODUCTION
A fracture can be a sentinel event for an older adult, resulting in death or serious physical or psychological injury to the patient. Such injury can either trigger a decline or can be seen during the course of an ongoing decline and may require a significant amount of time for recovery. This chapter reviews different outcomes, their incidence and predictors, presenting both individual and situational risk factors, and approaches that may help to improve outcomes. This chapter addresses predominantly post-hospital outcomes; immediate outcomes and complications of fracture repair are discussed in Chapter 7. Because there are many types of fractures and a discussion of all outcomes for all fractures would be unwieldy, we focus on the fractures that are most common in older adults – proximal femur fractures, distal radial/ulnar fractures, proximal humerus fractures and vertebral fractures, which are all usually considered to be fragility fractures (see Chapter 1 for more on the incidence of these fractures). Discussion focuses on mortality, function and health-related quality of life for each of these fractures, and other outcomes of clinical concern are presented.
STAKEHOLDERS, GOALS AND PRIORITIZED OUTCOMES
There are multiple stakeholders whose goal is to optimize the outcome of a fracture. These include the patient, informal and formal caregivers, healthcare professionals, healthcare systems and payors. To this end, the goals in an optimal care setting have been noted to be those outlined in Table 9.1.1 A recent consensus conference in the United Kingdom supported five domains as core outcomes to measure for any trial related to hip fracture: mortality, pain, activities of daily living (ADL), mobility and health-related quality of life.2
PATIENT PREFERENCES
Understanding a patient’s values and goals of care is important for providing optimal care for all patients, but particularly for older adults, where there may be trade-offs involved due to frailty and comorbidities. Although mortality is often viewed as the ‘worst possible’ outcome when assessing trade-offs, other outcomes, such as functional status, mobility, pain control and fear of being a burden, may take priority in an older or more frail individual’s values.
It is therefore important to discuss goals of care with patients in order to weigh the risks and benefits of a procedure, and for care planning. This may be particularly challenging for patients with dementia or other conditions that limit their ability to weigh options or to state preferences, and in this situation, discussions with family members or others who are close to the individual can be invaluable in understanding meaningful outcomes.
INTER-RELATIONSHIP OF OUTCOMES
As thoroughly discussed in Chapter 7, frail patients, or those with limited physiological reserve, are at high risk for multiple adverse outcomes. These outcomes may be inter-related. As an example, hip fracture patients who develop neuropsychiatric symptoms, such as night-time behaviour disturbance, agitation or depression, are at higher risk for motor function decline.3 Patients with functional or cognitive decline are at risk of needing an increased level of care. This has implications for prognosis as well as care. First, identifying individuals at high risk for adverse outcomes helps to frame discussions for care planning. Additionally, targeted care in the acute and rehabilitation setting may in turn lead to improvement in multiple outcomes and prevent a vicious spiral that may occur when one adverse outcome leads to another.
Table 9.1 Goals for optimized care
|
MORTALITY
Risk of mortality following a fracture depends primarily on the site of the fracture (Figure 9.1),4 which is discussed under the subheadings below, but also on the characteristics of the patient. For many, fractures serve as a marker of frailty and comorbidity.
Osteoporotic fractures overall are associated with an increase in mortality risk.5 For hip, vertebral and other major fractures, this is true for all older adults. In individuals aged 75 and over, even minor fractures are associated with increased mortality risk. Standardized mortality rates are higher for men than for women, and this is especially true for men over the age of 75. Age and quadriceps strength are predictive of mortality in both women and men with fractures, and sustaining a subsequent fracture is also a marker for increased mortality risk.
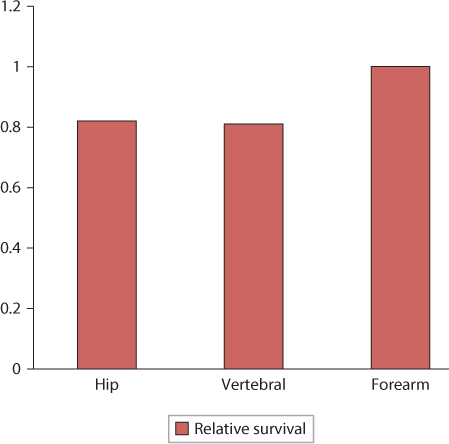
Figure 9.1 Relative survival at 5 years.
Hip fractures
Mortality following a hip fracture is increased. Mortality rates in the year following hip fracture vary substantially depending on the patient population, ranging from 12.7% in a community dwelling, cognitively intact patient population at baseline,6 to 58.3% in male nursing home residents.7 Although the demographics of hip fracture patients have changed in the past several decades, with increasing age at presentation, the overall mortality in the year following a hip fracture has not changed significantly.8
The excess mortality is highest immediately following a hip fracture. In the first 3 months, women are five times more likely to die, and men are eight times more likely to die than their counterparts who have not sustained a fracture. Excess mortality drops throughout the first year, but persists for at least 10 years for both women and men.5,9 Viewed another way, hip fractures reduce life expectancy by 1.8 years or by about 25% relative to age- and sex-matched counterparts.10
It is estimated that fewer than a third of deaths following hip fracture are causally related, but that the predominance of mortality among hip fracture patients is due to their underlying frailty and comorbidity.11,12 This has implications for clinical care. For those whose mortality is related to outcomes of caring for the fracture and its consequences, optimizing systems and the specifics of care to reduce adverse outcomes is the approach that will improve mortality. For those whose mortality is related to their underlying frailty, reducing comorbidity and improving function, treating osteoporosis and preventing falls is the approach that will ultimately reduce fracture mortality.
Predictors for mortality following a hip fracture are outlined in Table 9.2 and can be divided into baseline and incident predictors. Nursing home residents are at particularly high risk of mortality during the year following a hip fracture. At baseline, significant predictors include demographic characteristics, such as age, gender and residence. Poor baseline cognitive and physical function both predict higher mortality following a fracture. In terms of incident predictors, there is growing evidence that delay in surgery leads to higher mortality,13 and this is particularly important in patients with functional impairment.14 Development of postoperative delirium or pressure sores leads to a higher risk of 1-year mortality.15 At the time of hospital discharge, function as measured by the motor Functional Independence Measure (FIM) score has been shown to be highly predictive of 1-year mortality.16 Incident predictors are at least partially modifiable risk factors which, if reduced, may improve mortality outcomes.
Proximal humerus fractures
Although the proximal humerus is a common site for fragility fractures, there are less data on outcomes than for other sites, such as hip or vertebral fractures. Mortality has been found to be high in patients with proximal humerus fracture, with a mortality rate that is approximately double that of individuals without fracture.12 The impact on men appears to be greater than on women, with a median survival time of 6.5 and 11.8 years in male patients and their controls, respectively, and 9.0 and 11.5 years in female patients versus controls.17
Table 9.2 Predictors of mortality after a hip fracture
Baseline risk factors |
Male gender |
Older age |
Admission from a nursing home |
History of smoking |
Low baseline activity level |
ASA grade/significant comorbidity |
Poor cognitive status |
Poor baseline mobility |
Quadriceps weakness |
Incident risk factors |
Delay in surgery |
Incident delirium |
Incident pressure sore |
Function at hospital discharge |
Note: ASA, American Society of Anesthesiologists.
As with other fracture sites, mortality appears to be driven by underlying frailty and comorbidity. In one case series of 100 patients with proximal humerus fracture,18 patients with severe physical or mental disorders, such as dementia or severe cardiovascular disease, were much more likely to die in the year following their fracture. Forty percent of these patients died, compared with 2% of those with non-severe comorbidity and none of those without. In the case–control study above,17 most patients died of cardiovascular disease or malignancy; in other words, they died of significant comorbidities.
Vertebral fractures
Vertebral fractures are associated with an increase in mortality in both women and men, with standardized mortality rates (the ratio of observed to expected deaths) of 1.8 and 2.1, respectively.5 Similar to hip fractures, excess deaths appear to be a function of both the fracture itself and underlying comorbidity and frailty, with the predominance due to the latter.19 The excess mortality at 5 years is similar to that seen in hip fractures (Figure 9.1), however the patterns are different. Patients with hip fractures see higher mortality immediately following the fracture, whereas among patients with vertebral fractures, the mortality curves relative to expected mortality continue to diverge over a 5-year period.4
Similar to hip fracture outcomes, men have higher mortality rates than women following a vertebral fracture.4,20 Older individuals are at higher risk of mortality as well.4 Patients who sustain fractures as a result of mild to moderate trauma have an increased mortality risk, whereas those who fracture due to severe trauma do not. The most common cause for death in the former group is cardiovascular disease,4 again supporting the idea that these are more frail patients with higher comorbidity.
Distal forearm fractures
The excess mortality does not appear to be elevated among patients with forearm fractures,4,12 and, in fact, there is some evidence that women with distal fractures may have a lower mortality than the general population.20 Similar to other types of fractures, this may reflect the patient population that sustains forearm fractures; this population tends to be younger and more vigorous than their counterparts with other osteoporotic fractures.21 The mechanism for incurring a forearm fracture suggests both substantial forward momentum and preserved reflexes, consistent with a more active and robust individual.22
Other fractures
Rib fractures are also associated with an elevated mortality, particularly in women.5 There is significant excess mortality in the months following rib fractures, but the mortality curves continue to diverge for several years, suggesting ongoing elevated risk.12
FUNCTION
Function involves multiple domains, including physical, cognitive, psychological and social. Physical functional status is often measured globally in older adults via ADL and instrumental activities of daily living (IADL). ADL cover activities related to self-care and the ability to live independently, namely, dressing, toileting, transferring, grooming, bathing and feeding oneself. IADL involve more complex tasks, such as using the telephone, managing medications, shopping, taking care of household finances, doing laundry, preparing meals, doing housework and managing transportation.
Other measures were developed to assess function related to the specific location affected. For example, the Michigan Hand Questionnaire measures outcomes in six domains via 37 questions: function, ADL, pain, work performance, aesthetics and patient satisfaction.23 It is scored from 0 (poor) to 100 (excellent). A brief version that includes 12 items is also available, with a responsiveness that is similar to the original questionnaire.
The Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire is another self-reported score that is used to evaluate functional outcomes in the upper extremity.24 It provides a score from 0 (no disability) to 100 (complete disability) based on 30 questions addressing activities, limitations and symptoms. A change of 10 points is considered to be clinically meaningful.
The Constant–Murley score is a 100-point score to evaluate shoulder function that encompasses both patient report and objective measurement. It evaluates pain, ADL, strength and range of motion. Higher scores denote better function.25
Osteoporotic fractures have a huge functional impact. It has been estimated that the 5.2 million fractures of the hip, spine and distal forearm that occur among post-menopausal white women in the United States in a 10-year period would lead to 2 million person-years of fracture-related disability.26 A history of any osteoporotic fracture is associated with a two- to threefold increase in difficulty bending, lifting, reaching, walking, climbing stairs and descending stairs, and two- to almost seven times more difficulty in dressing, cooking, shopping and performing heavy housework.27
Hip fractures
The trajectory of functional recovery from a hip fracture depends on the area of function being assessed.28 Most areas improve in the first year following the fracture, with earlier recovery for depressive symptoms, upper extremity function and cognition (4 months), and longer times to recovery of social, IADL and lower extremity functioning, which take about 11 months. Understandably, the IADL that are most likely to be impacted are those that depend on lower extremity functioning, such as housecleaning and shopping (62% and 42% dependent at 1 year, respectively, for those who were previously independent), whereas those that are not as dependent on lower extremity functioning, such as medication management and using the telephone, are less impacted (28% and 22%, respectively). Limitation in function 1 year after a hip fracture is substantial (Figure 9.2)28; for those who were previously independent, new dependency in physical ADL at 1 year ranges from 20% for putting on pants to 90% for climbing five stairs. Two-thirds still have difficulty getting on and off the toilet. Most of these dependencies persist 2 years after the hip fracture.
There is considerable overlap between risk factors for mortality and those for functional impairment following a hip fracture (Table 9.3).29,30,31 and 32 Older individuals, those with dementia, depression or other significant comorbidity, and those with poor baseline functioning are at higher risk for functional impairment after a hip fracture. Postoperative anaemia has been associated with decreased ambulation and reduced functional independence31; however, a liberal transfusion approach (transfusing for a haemoglobin level of 10 g/dL vs 8 g/dL) does not appear to improve functional outcomes.33
With respect to incident risk factors, longer length of stay and being rehospitalized are associated with worse postoperative function. Prolonged immobilization and delay in start of physical therapy can lead to loss of muscle function and higher risk of several medical complications (see Chapter 7), which in turn sets the stage for poor functional recovery. A surgical approach that allows for immediate weight bearing as tolerated will foster the start and progression of physical therapy; furthermore, patients with cognitive impairment may have difficulty following restrictions such as partial toe-touch weight bearing, and this may impede progress in therapy. The amount of contact with one’s social support network following hospitalization is also predictive of functional recovery. The mechanism for this may be multifaceted. Those with more social support may have more opportunity to be physically active and may be less prone to depression that may impact progress.
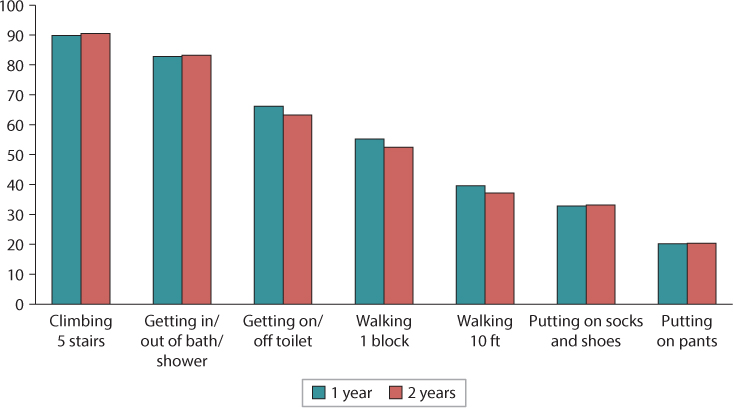
Figure 9.2 Percentage dependent among those who were independent before fracture.
Table 9.3 Predictors of poor recovery of function after a hip fracture
Baseline risk factors |
Older age |
Low pre-fracture physical function |
Depression |
Poor cognitive function, dementia |
Poor nutritional status |
Multiple comorbidities, ASA grade of 3 or 4 frailty |
Incident risk factors |
Length of stay |
Less physical therapy in hospital |
Rehospitalization |
Low level of contact with social support network |
Note: ASA, American Society of Anesthesiologists.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








