Fig. 27.1
Osteochondritis dissecans during the initial asymptomatic phase. Upper: the elbow at AP 45° of flexion (tangential view). Lower: the elbow in oblique view at 45°. Yellow arrow: lesion. Red arrow: lesion boundary
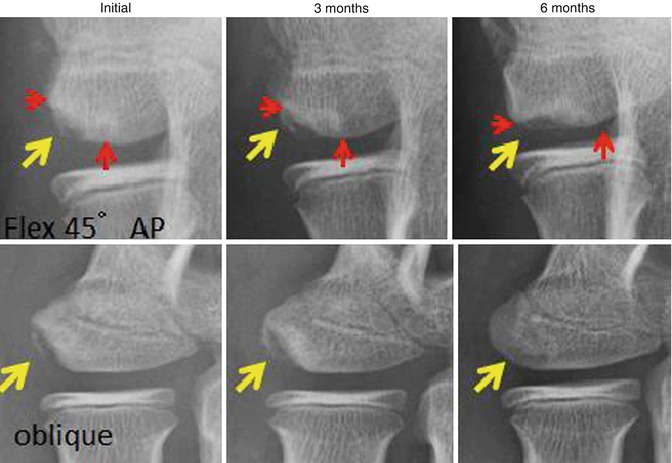
Fig. 27.2
Osteochondritis dissecans discovered after throwing-related pain is reported. Upper: tangential view. Lower: oblique view. Yellow arrow: lesion. Red arrow: lesion boundary
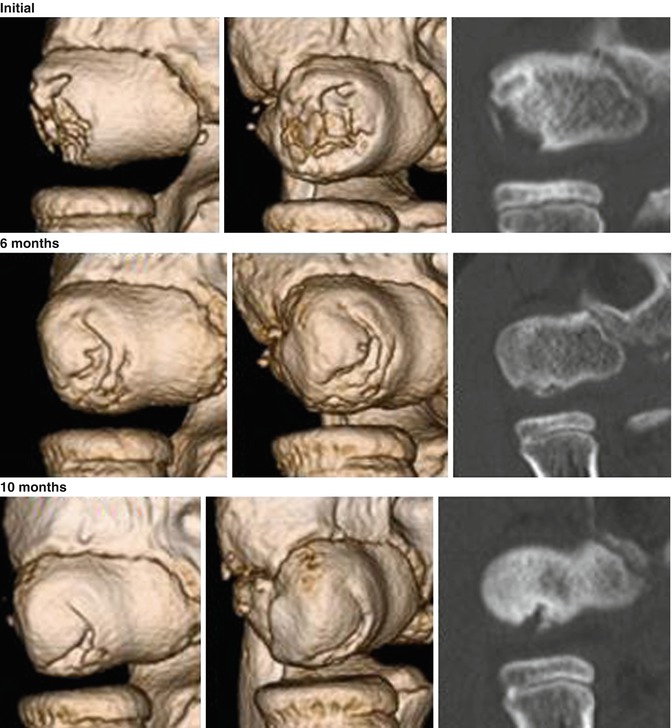
Fig. 27.3
Three-dimensional computed tomography and coronal view. The lesion originates from the lateral aspect of the capitellum and spreads to the center (initial → 6 months). The lesion is repaired from the outside (6 → 10 months)
Imaging findings vary depending on exacerbation or repair (Fig. 27.4). If the repair process stops before the entire lesion heals, lesions will be left within the central portion of the capitellum. The epiphyseal line is usually already closed (Fig. 27.4, case 1). When the repair process stops to soon, the lateral walls will not be sufficiently repaired (Fig. 27.4, case 2). When the repair process does not advance, extensive lesions will persist on the entire capitellum from the outside to the center (Fig. 27.4, case 3). In this case, extensive reconstruction of the articular surface will be required.
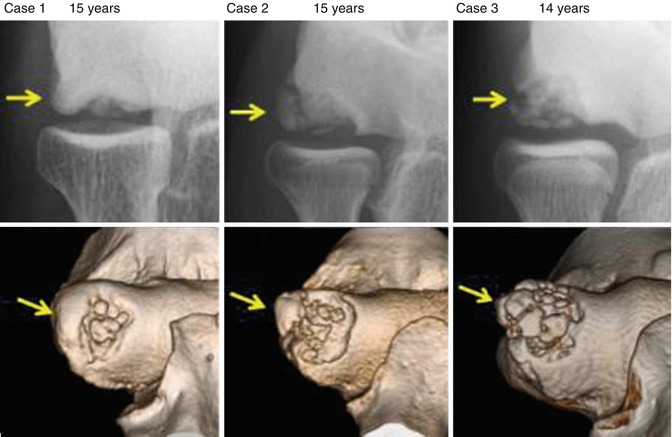
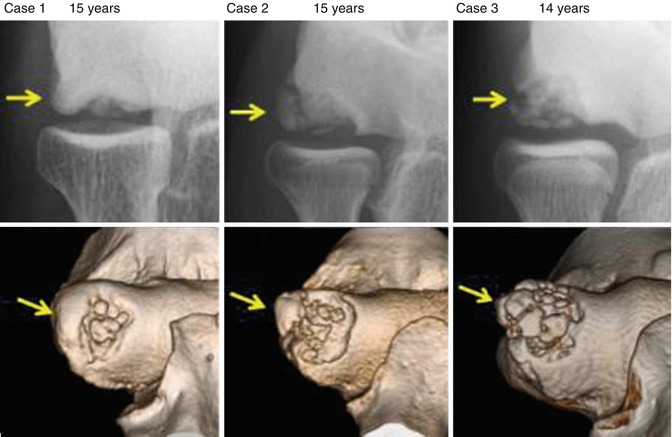
Fig. 27.4
Differences in the lesions depend on when recovery arrests. Case 1. Lateral walls are repaired, but a lesion remains in the center. Case 2. Lateral wall recovery was arrested and some fragments remain. Case 3. Lateral walls are not restored and extensive lesions remain
27.2.3 Preferred Classification
Minami et al. [5] reported a plain radiographic classification for OCD for the first time (1979). Based on plain radiographic images, the classification was defined as follows (Fig. 27.5): translucency type (stage I), translucency of localized bone on the humeral capitellum; separation type (stage II), perifocal bone sclerosis or a clear zone between the lesion and surrounding bone tissues; and free type (stage III), the lesion is completely detached from the humeral capitellum and exists as a free body in the joint.
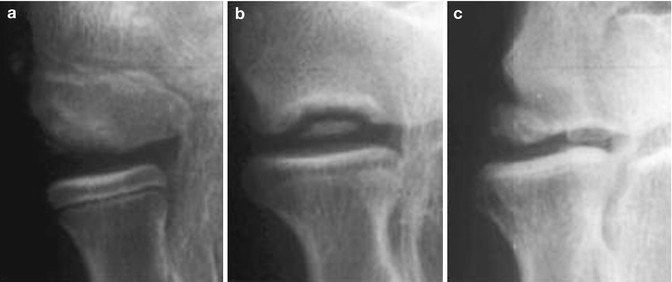
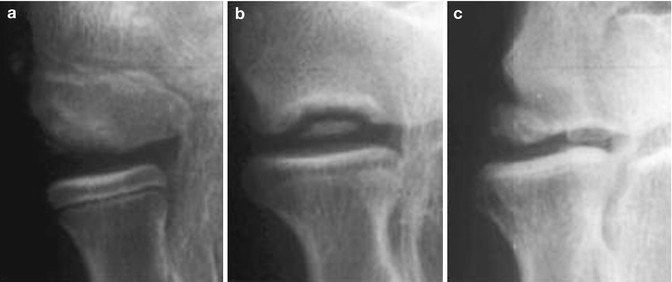
Fig. 27.5
Radiographic classification of osteochondrosis of the humeral capitellum. Stage I was characterized by translucency (a). In stage II, nondisplaced fragments were present (b). Loose bodies and sclerotic change indicated stage III (c) (Matsuura et al. [4])
The conditions for acquiring images were defined as 45° flexion view (tangential view) to assess the disease stages in detail: translucency period, exterior type and central type; separation period, first-term type and latter-term type; and free body period, internal or external to the lesion.
Based on lesion sites, it can be classified as follows: central localized type, external localization type ranging from the outer wall of the lateral epicondyle to less than one-third of the articular surface on the radial head, and extensive type, ranging from the outer wall of the lateral epicondyle to one-third or more of the articular surface on the radial head. It is important to understand the lesion site and its range in surgical treatment.
27.2.4 Statistics of Surgical Patients with OCD
Between 1990 and 2012 (23 years), 741 patients with OCD underwent surgery in our hospital (mean age, 14.5 years). Approximately 90 % of these patients had baseball-related disorders. The others suffered from OCD induced by tennis, handball, basketball, or gymnastics. The age distribution (Fig. 27.6) shows that the majority of patients were 13–15 years of age.
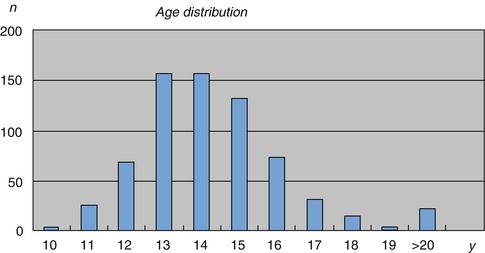
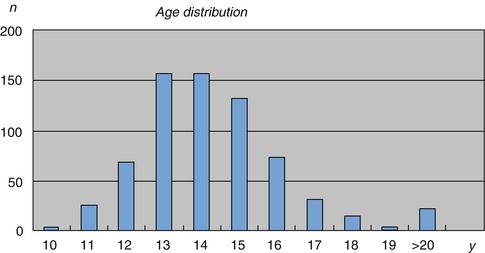
Fig. 27.6
Mean age at surgery of the 741 patients with osteochondritis dissecans
Approximately 600 patients with baseball-related disorders visit our hospital annually. Approximately 80–100 patients with OCD have visited annually over the past 10 years. Of these patients, approximately half required surgery (Fig. 27.7).
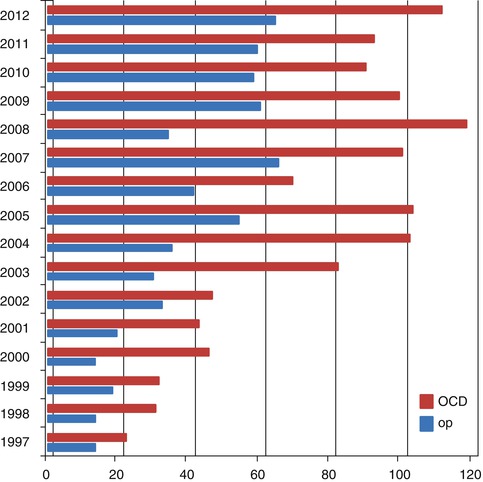
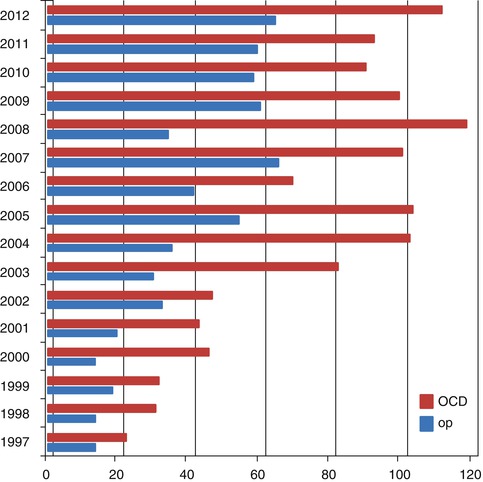
Fig. 27.7
The annual number of outpatients with osteochondritis dissecans (OCD) (in red) and the annual number of surgeries performed for OCD (in blue)
27.3 Clinical Presentation and Essential Physical Examination
Initial symptoms of OCD include discomfort, swelling, and limited extension of the elbow joint after baseball training. However, the pain is commonly mild and can be improved with rest. Consequently, players can continue playing baseball unless such conditions progress, and they are likely to delay visiting medical institutions. In physical examination, patients complain of swelling and reduced range of motion as well as localized tenderness when the capitellum is compressed on the anteroinferior side with the elbow joint in flexion. Bulging may be found in the soft spot outside of the elbow because of synovial fluid or swelling of the synovial plica. Compared with the unaffected side, flexion or extension of the elbow joint shows apparent limited range of motion, but forearm pronation and supination are usually not limited. For patients in whom flexion or extension and pronation and supination of the forearm cause catching, clicking, locking symptoms, or pain, detachment of the cartilage surface or the presence of a free body is suspected. Conservative treatment before epiphyseal closing leads to a better therapeutic effect. Recovery tends to stop when the epiphyseal line closes.
Patients with bone sclerosis around the lesion and tenderness of the capitellum often tend to have instability of the articular cartilage. In that case, compared with imaging findings, surgery findings include extensive destruction of the articular surface beyond the surgeon’s expectation and show differences in cartilage degeneration (Fig. 27.8). Thus, it is difficult to preoperatively determine a specific surgical method.
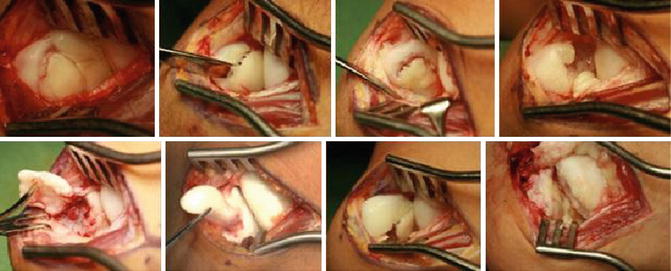
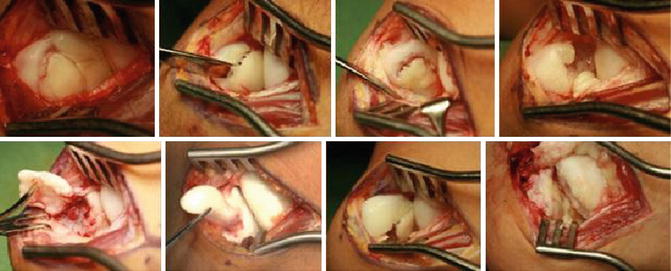
Fig. 27.8
Various findings on operation. Plain radiographs showed that the lesion is in the separation type, but the articular cartilage shows various statuses
27.4 Essential Radiology
27.4.1 Plain Radiographs
For patients with a throwing elbow disorder, plain radiographs must be obtained from four directions. Tangential and oblique views at 45° in particular are required to detect OCD since it is likely to be overlooked when only plain anterior-posterior (AP view) and lateral radiographic images are used (Fig. 27.9).


Fig. 27.9
Upper: the elbow in flexion from the AP view and lateral directions. Lower: the elbow in 45° of flexion (tangential view), the elbow in oblique view. Arrow: lesion
The above images were obtained from the same patient. The upper images were obtained from the AP view and lateral directions, in which the OCD is unclear. The lower tangential and oblique views visualize the OCD outside the capitellum. In the initial diagnosis of OCD, taking a sufficient sports history into consideration is important and diagnostic examinations are essential for identifying OCD. Plain tangential and oblique radiographs are available for follow-up of bone regeneration of the lesion treated by conservative treatment or surgical therapy.
27.4.2 Ultrasonography (US) Aids in the Diagnosis of OCD
Its advantages include early detection is possible; the subchondral bone and the articular cartilage can be observed simultaneously; more detailed tomographic images than plain radiographs can be obtained; not only osteogenic but also cartilaginous free body can be detected; and observation is possible during flexion and extension of the elbow joint (Fig. 27.10). It can also be useful as a screening examination outside of medical institutions (fieldwork) when portable US devices are used.
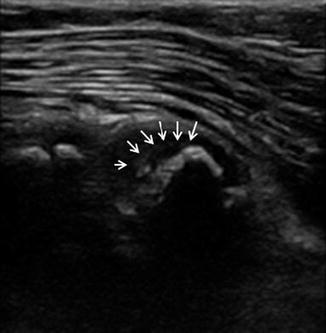
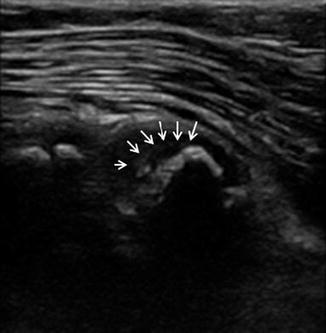
Fig. 27.10
Ultrasonography of osteochondritis dissecans of the humeral capitellum (sagittal view). Arrow: defect of the subchondral bone
27.4.3 Computed Tomography (CT)
CT can visualize even an unclear subtle lesion on plain radiographs. It is useful for confirming bone fragment properties, free body location, exact affected width and depth, subchondral bone status, and bone sclerosis absence or presence. CT can also be used to determine the healing effects of conservative and surgical treatment. In addition, three-dimensional (3D) CT is available to observe lesion dimensions, which is helpful for planning surgery. However, it should be noted that it is difficult to understand the state of the cartilage and detect cartilage-rich free bodies.
27.4.4 Magnetic Resonance Imaging (MRI)
MRI can be used to detect initial OCD that is difficult to detect on plain radiographs. MRI is also available to evaluate cartilage degeneration and fissure as well as lesion instability. T1-weighted imaging reveals a low-intensity area of the capitellum from the early stage of OCD. T2-weighted fat suppression imaging in the sagittal section shows changes in articular cartilage (Fig. 27.11). Surgical treatment is considered when lesion instability is evaluated by synovial fluid penetration into the subchondral bone or articular cartilage discontinuity. However, screening is not usually performed because of the time and cost involved. Nelson et al. [6] classification (Table 27.1) can be used to classify OCD using MRI.


Fig. 27.11
Magnetic resonance imaging. T1-weighted image in the upper left shows low-intensity lesions. T2-weighted fat suppression images in the upper right and lower right and left show high-signal articular cartilage and low-signal subchondral bone
Table 27.1
The MRI grading system for osteochondritis dissecans lesions
Grade | Description |
|---|---|
0 | Normal |
1 | Intact cartilage with signal changes |
2 | A high-signal breach of the cartilage |
3 | A thin, high-signal rim extending behind the osteochondral fragment, indicating synovial fluid around the fragment |
4 | Mixed- or low-signal loose body, either in the center of the lesion or free within the joint |
Diagnostic imaging techniques have undergone tremendous technological advances in this decade. Diagnostic techniques such as 3D CT and US are progressing remarkably, while MRI precision improves yearly. MRI will be available for further detailed evaluation. However, to decide whether surgical treatment should be provided or conservative treatment should be continued, it is necessary to evaluate local findings and various imaging studies.
27.5 Arthroscopic Pathology
27.5.1 Advantages of Arthroscopy
The International Cartilage Repair Society (ICRS) [2] classifies OCD lesions into four classes based on arthroscopy findings of knee joint lesions (Table 27.2). Baumgarten et al. [1] proposed a classification for OCD of the humeral capitellum using arthroscopy (Table 27.3).
Table 27.2
ICRS classification system for OCD lesions
Stage I: Stable lesion with a continuous but softened area covered by intact cartilage |
Stage II: Lesion with partial discontinuity that is stable when probed |
Stage III: Lesion with a complete discontinuity that has not yet dislocated (“dead in situ”) |
Stage IV: Empty defect, or defect with a dislocated fragment or a loose fragment within the lesion bed |
Table 27.3
Classification system for osteochondritis dissecans
Grade | Description |
|---|---|
1 | Intact but soft ballottable cartilage |
2 | Fissuring of the overlying cartilage |
3 | Exposed bone or attached osteoarticular fragment |
4 | Loose, but nondisplaced, osteoarticular fragment |
5 | Displaced fragment with resultant loose body |
These classifications show the degree of lesion instability by probing under arthroscopy. Arthroscopy can be used to understand the status of the affected cartilage and diagnose lesions to choose the appropriate surgical method. It is available for evaluating lesions and treating complicated lesions such as free body removal (Fig. 27.12) as well as resection of osteophytes on the olecranon or the synovial plica.


Fig. 27.12
Free body resected under arthroscopy
27.5.2 Postures for Arthroscopy
The authors perform arthroscopy of the elbow with the elbow in anterior flexion and the patient in a supine position (Fig. 27.13). The supine position is easy to set up and enables the surgeon to switch to open surgery as needed (such as with osteochondral mosaicplasty). We place a sandbag under the patient’s shoulder to stabilize the arms and position the forearm on an armrest to hold the upper extremities.


Fig. 27.13
Arthroscopy posture. A sandbag is placed under the patient’s shoulder joint in the supine position and the elbow is positioned in flexion on the armrest
We then inject 10–15 mL of 1 % lidocaine with epinephrine into the joint. After confirming the optimal portal site using a 23 G needle, we perform arthroscopic surgery from the posterior, posterolateral, and soft-spot portals. Implantation from the anterolateral and anteromedial portals is performed with special attention paid to the cutaneous nerves of the forearm. The scalpel is inserted to run parallel to the skin’s surface. Minor forceps are then bluntly inserted subcutaneously from the muscular fasciae into the joint capsule to extend the portal. We then observe the lesion using 30° or 70° arthroscopy with a diameter of 2.7–4.0 mm.
To perform bone peg grafting or osteochondral mosaicplasty, we immediately switch to open surgery. Open surgery is superior for extensive lesions requiring articular surface reconstruction and can be used to reconstruct the articular surface from ideal directions. Since long-time arthroscopy may result in periarticular edema and the working space is small, manipulation under arthroscopy is not required. Except in simple surgeries such as drilling, arthroscopy is not suitable when reconstructive surgery of the articular surface is required.
27.5.3 Pitfalls of Arthroscopy
The articular cartilage observed through arthroscopy, even if it is an apparently extensive lesion on CT or MRI, may be graded as grade 1 according to the ICRS scale. Caution should be taken because arthropathic changes may progress if such a lesion is treated with drilling only. Attention should be paid to adapt arthroscopic drilling, as it should not be performed in extensive lesions since it can promote destruction of the articular surface.
Although the lesion in Fig. 27.14 has no subchondral marrow, it was treated by arthroscopic drilling because the cartilage surface was clean. In this case, the patient visited our hospital several months after surgery. Plain radiographs showed that the joint space of the humeroradial joint had disappeared and the radial head was enlarged. On 3D CT, the humeroradial joint, transformation of the trochlear, and a superiorly extended radial head were found. Remarkably limited range of motion was also seen at elbow extension of 45° and flexion of 90°. Arthrography showed that the articular cartilage of the capitellum and the radial head were destroyed (Fig. 27.15).

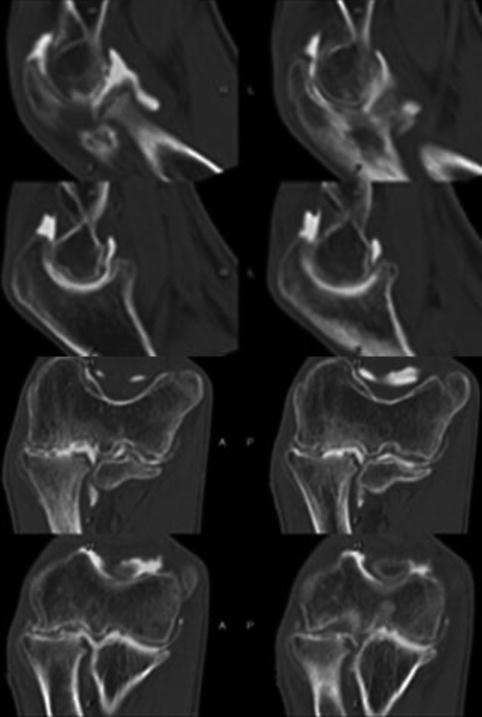

Fig. 27.14
Deformation progressed in the extensive osteochondritis dissecans lesion treated with drilling
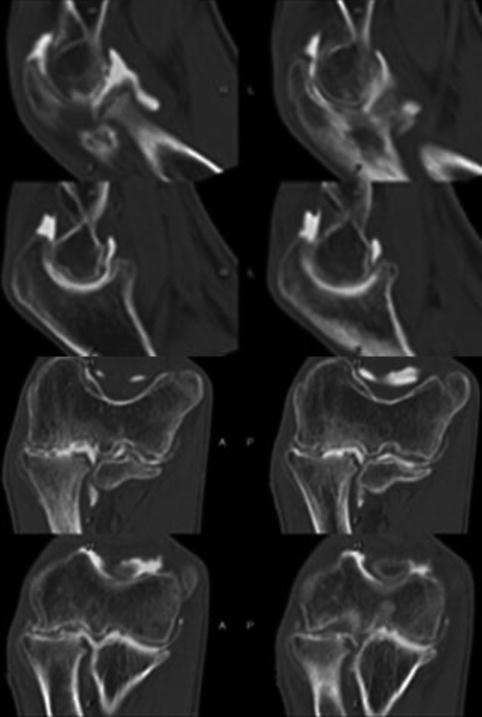
Fig. 27.15
Arthrography + computed tomography image. The articular cartilage of the humeral capitellum and the radial head have almost disappeared
The arthroscopy in Fig. 27.16 shows that alignment of the joint surface was maintained and the cartilage surface was very clean without softening (ICRS I). However, it was revealed unstable when the bone fragment was pushed up from under the lateral walls with probe. In such a case, it is often difficult to confirm instability using arthroscopy. It is hazardous to determine a surgical method by evaluating only the articular cartilage condition because the OCD lesion is caused by necrosis of the bone marrow beneath the articular cartilage.
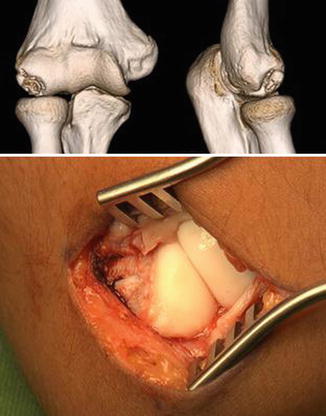
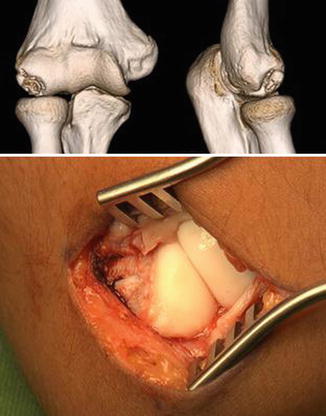
Fig. 27.16
The surface of the articular cartilage of the extensive type of osteochondritis dissecans. Note the small fragments in the lateral walls and the deficiency of the subchondral bone in the center in MRI. In the intraoperative photograph, the articular cartilage is clean and its instability cannot be confirmed from the surface view. However, the surface was unstable when the lateral wall was pushed up with the probe
27.6 Treatment Options
27.6.1 Nonoperative Treatment
For OCD in school-age children, conservative treatment is given priority. Especially for baseball players, throwing and batting are forbidden and fielding practice is prohibited. Healing tends to occur late when motions other than throwing are permitted. For patients with extensive lesions ranging from outside the capitellum to its center, bicycle riding is also prohibited. If patients show clear swelling and pain on motion, it is desirable that they wear a splinting with the elbow in 45° of flexion whenever leaving home (for 4–8 weeks) (Fig. 27.17).


Fig. 27.17
Wearing of the splint at 45° of flexion of the elbow. This brace is taken off while bathing, eating, and sleeping
Conservative treatment is initially provided for at least 4–6 months. If healing process is seen upon various imaging examinations, the same conservative treatment is continued. Lesions in which continuity of the subchondral bone is confirmed on MRI and/or CT are likely to respond to conservative treatment (Fig. 27.18).
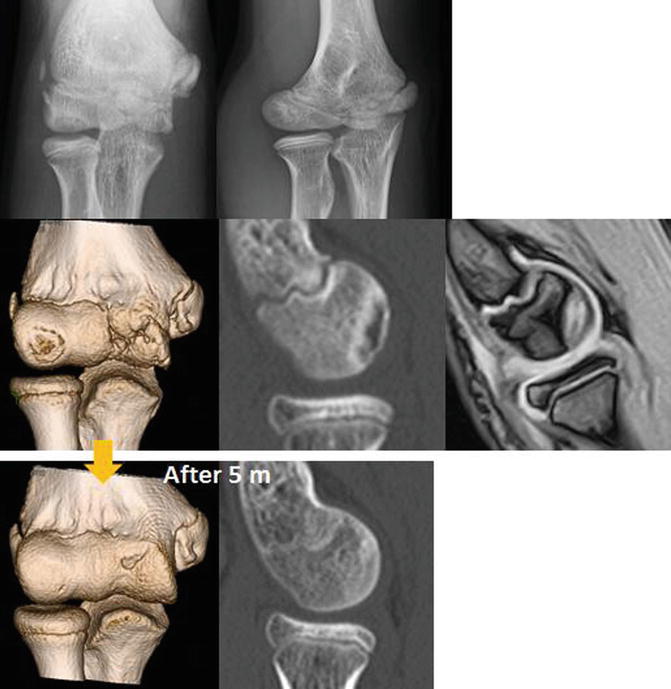
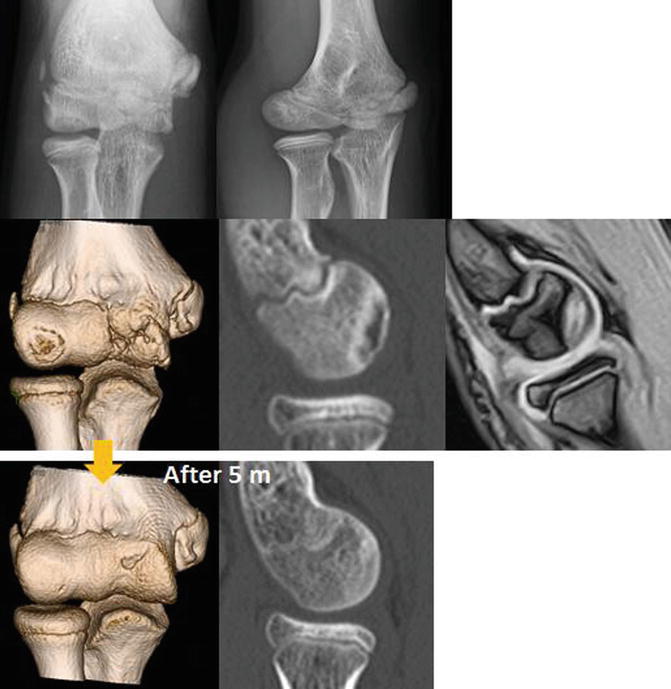
Fig. 27.18
Plain radiographs in the translucency period. Computed tomography and magnetic resonance imaging show the continuity of the subchondral bone and cartilage. The lesion was completely repaired 5 months after treatment initiation
After the healing process declines after considerable improvement, and their lesions are classified into the central type, and the lesion area is stable and <30 % of the area of the capitellum, the authors allow the patients to return to sports with awareness that if they have no pain. A free body may subsequently form, in which case its removal should be performed earlier.
27.6.2 Low-Intensity Pulsed Ultrasound (LIPUS) Treatment
LIPUS treatment is currently used as an adjuvant fracture treatment. However, there is no evidence whether LIPUS treatment for OCD promotes recovery and whether a case of delayed union is also repairable. Accordingly, if the number of the cases to be switched to surgery decreases or if it promotes recovery, the effectiveness of LIPUS for OCD will be expected.
The authors compared the patients treated with LIPUS (LIPUS) or without LIPUS (non-LIPUS) in similar stages of OCD. As shown in Fig. 27.19, clean repair in the LIPUS group took 2 months and 3 days, while that in the non-LIPUS group took 5 months and 21 days. This finding suggests that the repair period can be shortened.
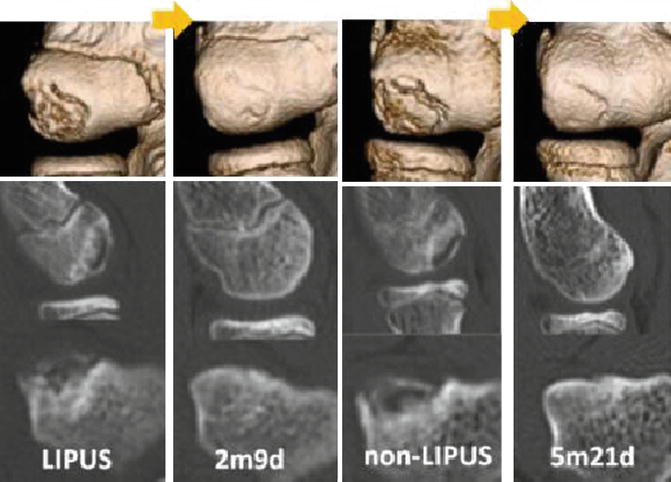
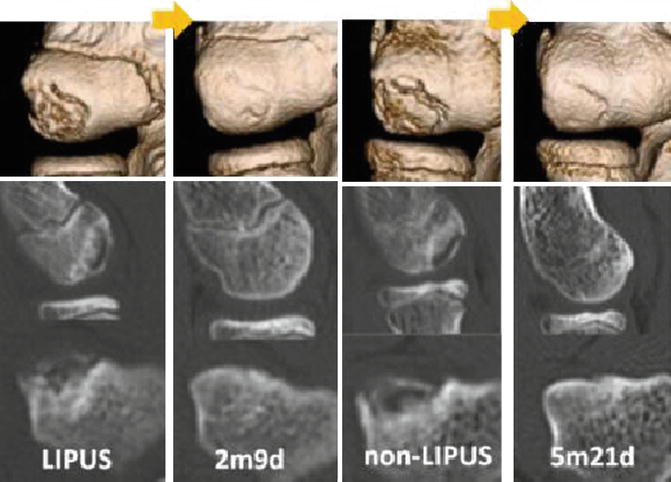
Fig. 27.19
Comparison of the images of osteochondritis dissecans in the translucency period. Left: low-intensity pulsed ultrasound was performed. The entire lesion was repaired at 2 months and 9 days after treatment initiation. Right: the lesion was treated with rest only as conservative treatment
In another study, the authors performed LIPUS in 51 patients with OCD regardless of disease stage and found that LIPUS was effective and ineffective in 22 and 29 patients, respectively. The repair period was approximately 6.4 months in the effective group, including 14 patients in the advanced disease stages, which showed earlier recovery than the usual repair period (10–12 months). Recovery seems to be rapid when the surface of the articular cartilage has not fissured. The recovery state on CT was also examined from the viewpoint of the presence or absence of perifocal osteosclerosis. As a result, in the group without osteosclerosis, 19 of 35 patients (54.3 %) showed an almost fully repaired state. In the group with osteosclerosis, 3 of 16 patients (18.8 %) showed a repaired state (Table 27.4). The difference between groups was significant.
Table 27.4
Conservative treatment (LIPUS) of the osteochondritis dissecans
Sclerotic change | +
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|





