(1)
Paediatric and Young Adult Orthopaedic Unit, The Royal London and Barts and The London Children’s Hospitals, Barts Health, London, UK
Introduction
This chapter covers those conditions in which there are significant musculoskeletal consequences of neurological or muscular pathology. The topics covered are:
Cerebral palsy.
Myelodysplasia (spina bifida).
Poliomyelitis.
Duchenne muscular dystrophy.
Hereditary motor and sensory neuropathy.
Cerebral Palsy
Cerebral palsy (CP) is the term given to a group of conditions in which a non-progressive brain lesion at or around birth gives rise to disorders of posture and movement. The lesion may be a discrete focus of haemorrhage or cyst formation, or it may be the result of more diffuse damage from ischaemia or infection. The premature brain is especially vulnerable to ischaemic damage, and babies born under 30 weeks gestation are at high risk of ischaemic hypoxic encephalopathy. There is also a wide range of autosomal recessive inherited syndromes with neurodisability similar to that seen in CP. Overall, CP is relatively common, with an incidence of about 2 per 1000 live births.
As a result of the central lesion, damage to the corticospinal tracts results in impaired control of the spinal reflex arc, which in turn gives rise peripherally to the characteristic movement disorder of spasticity. This is an exaggerated response to the normal stretch reflex. Spastic muscles resist stretch, which is essential for the normal growth and development of muscle. As a consequence, spastic muscle does not grow properly, and contractures and deformity can result (Fig. 3.1). Other movement disorders include athetosis (uncontrolled writhing movements) and dystonia (variable posture). Unlike spasticity, which is a disturbance of pyramidal system function, these latter disorders involve extrapyramidal tracts. The outcome of surgical interventions in these disorders is much less reliable and predictable than that of spasticity.
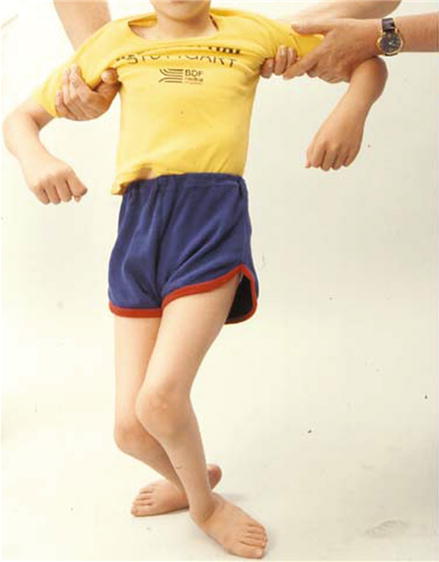
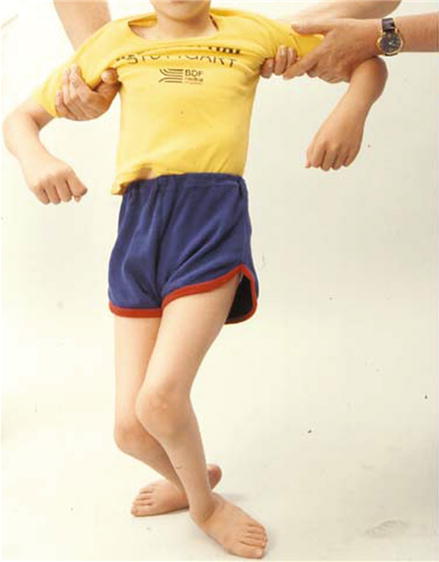
Figure 3.1
Bilateral flexion contractures at the knee (Reproduced from Benson et al. Children’s Orthopaedics and Fractures, 2009, Springer)
A child with CP may have:
Unilateral involvement, as in a stroke (hemiplegia).
Involvement predominantly of the lower limbs (diplegia).
Global involvement (quadriplegia).
Although global involvement used to be called quadriplegia, it now tends to be referred to as total body involvement (TBI), in recognition of the important effects on the axial skeleton in the form of scoliosis, and effects on the bulbar system involving swallowing and allied functions.
The role of the orthopaedic surgeon in the management of CP varies according to the extent of neurological involvement. Children with hemiplegia and many with diplegia will be able to walk, and the emphasis here is on treating contractures, foot and upper limb deformities, and torsional deformity in the lower limbs. Children with TBI are at particular risk of progressive hip dislocations and scoliosis. However severe the physical disability, it is important to remember that there may be little or no cognitive impairment.
Hemiplegia
This results from a focal lesion in the brain such as a cyst or haemorrhage. The effects are seen on one side of the body in the form of spasticity, which may lead in turn to contractures and deformity. Some muscle groups are involved more than others, giving rise to the typical upper limb posture of adduction and internal rotation at the shoulder, flexion at the elbow, pronation in the forearm, and flexion at the wrist and fingers. In the lower limb, there is typically equinus or equinovarus at the foot and ankle due to involvement of the calf muscles.
Diplegia
This is frequently the result of ischaemic or hypoxic damage to the immature brain and is seen in children who were born prematurely. The most obvious neurological abnormalities are seen in the lower limbs, with the upper limbs and axial skeleton relatively spared. Most of these children have some standing and walking ability, and surgical interventions are directed at maximising their walking potential. Many of them will develop calf and hamstring contractures, and they may have valgus feet and ankles.
Management of both hemiplegia and diplegia in the early years involves joint ranging and stretching exercises to maintain muscle length and encourage muscle growth. Serial casting is a technique that uses the stress-relaxation properties of muscle and tendon to achieve a gradual increase in muscle-tendon length. Children can be helped to adopt a normal gait sequence with the use of ankle-foot orthoses. Tone reduction can be achieved on a temporary basis by use of botulinum toxin, which interrupts motor endplate function by acting as a competitive inhibitor of presynaptic cholinergic receptors. Spasticity may also be reduced by selective destruction of the dorsal spinal roots (selective dorsal rhizotomy) or by continuous intrathecal infusion of baclofen, a tone-reducing drug which is thought to act as a GABA agonist, although its mechanism of action is not fully understood.
Ultimately it may be necessary to lengthen surgically the muscle-tendon unit. Surgery is best avoided in the early years as it interferes with muscle growth. Surgery may also unmask the underlying weakness of the involved muscles, and extensive releases in older heavier children may make it difficult for them to rehabilitate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








