11
Neurological System
Katie M. Walsh and Tamara C. Valovich McLeod
At the completion of this chapter the reader should be able to do the following:
1. Describe the anatomy and function of the nervous system
2. Recognize and assess an athlete with a suspected sport-related concussion
3. Describe a return-to-play progression for an athlete after sport-related concussion
4. Recognize and refer an athlete with signs or symptoms of a life-threatening neurological condition
5. Identify conditions that make an athlete susceptible to migraines and stroke
6. Recognize the symptoms of complex regional pain syndrome
7. Describe chronic neurological conditions and their effect on athletic participation
8. Differentiate when to make a referral to a physician for further neurological evaluation
Introduction
Neurological disorders in athletes are generally placed in two categories: life-threatening conditions such as encephalitis, meningitis, or stroke; and those with chronic implications, which may include Guillain-Barré, multiple sclerosis, migraines, amyotrophic lateral sclerosis (ALS), complex regional pain syndrome (CRPS), or epilepsy. In addition, there has been increased emphasis on sport-related concussion because of the incidence of and possible short- and long-term consequences of concussive injuries. Because of the age range and close living quarters shared by many college athletes, they are more susceptible to certain neurological diseases, such as meningitis. In addition, outdoor practices in the late afternoon warm weather are favorable to mosquitoes, the carrier of certain types of encephalitis. The health care provider who appreciates these conditions will be better able to recognize and possibly prevent contact with and spread of these deadly disorders. Infectious neurological conditions (encephalitis and meningitis) are discussed in Chapter 15.
Neuroanatomy
Skull
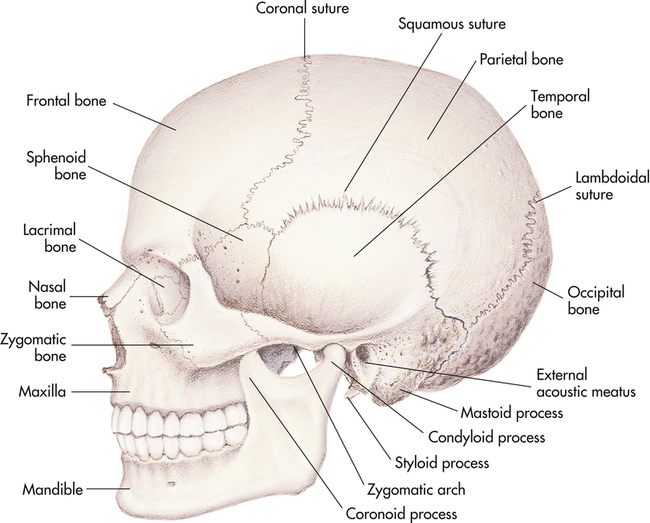
The human skull is made up of two main components: the cerebral cranium, which protects the brain and brainstem, and the anterior facial bony structure. The cerebral cranium consists of eight bones that include the frontal, two temporal, two parietal, occipital, sphenoid, and ethmoid bones. The facial skeleton is made up of the mandible, two zygomatic, two maxillary, and two nasal bones (Figure 11-1).
Meninges
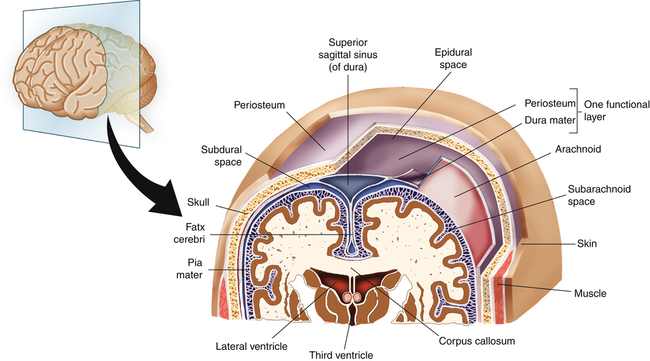
The inner lining of the dura mater forms folds in the cerebral hemispheres. The membranous plate known as the falx cerebri divides the hemispheres into right and left halves as seen in Figure 11-2. Another plate formed by the dura, the tentorium cerebelli, separates the cerebral hemispheres from the cerebellum and brainstem.
Meninges also provide a protective covering to the brainstem and spinal cord.
Cerebrum
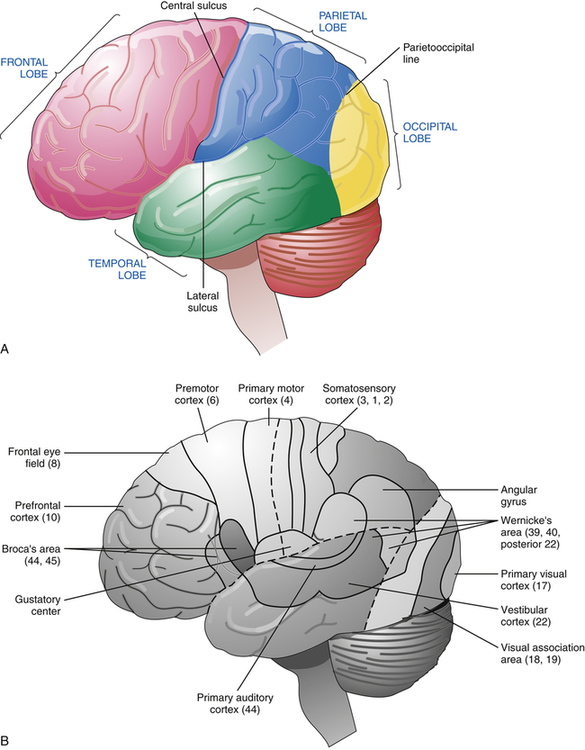
The two cerebral hemispheres are composed of neural tissue. These hemispheres are divided into four principal lobes: frontal, temporal, parietal, and occipital (Figure 11-3, A). The lobes have been extensively researched in attempts to isolate the locations of specific brain physiological functions and pathological processes. The most commonly used classification is Brodmann’s classification system, which identifies specific functional cortices of each lobe by numbers (see Figure 11-3, B).
Autonomic Nervous System
Box 11-1 lists the major functions of the parasympathetic and sympathetic nervous systems, which are generally antagonistic. The sympathetic nervous system is responsible for the fight-or-flight response and is catabolic in nature, expending energy as it prepares the body for danger. Conversely, the parasympathetic nervous system dominates during times of rest.
Disruption of the sympathetic system can lead to several clinical conditions. Horner’s syndrome is a neurological condition manifested by facial flushing of the affected side, ipsilateral miosis, and moderate ptosis of an eye. It is caused by a lesion or tumor at the level of the carotid plexus, cervical sympathetic chain, upper thoracic cord, or brainstem. Sympathetic pathway disruption at the level of the peripheral vascular system can lead to the severe vasoconstrictive episodes characteristic of Raynaud’s disease (see Chapter 14). Reflex sympathetic dystrophy and causalgia also involve abnormalities at the level of the peripheral blood vessels leading to sympathetic overactivity.
Spinal Nerves
and also contain axons from muscle spindles and skin and joint mechanoreceptors. The ventral roots are composed primarily of motor neuron fibers from skeletal muscle, as well as muscle spindle fibers, autonomic axons, and axons carrying thoracic and abdominal visceral sensory information.
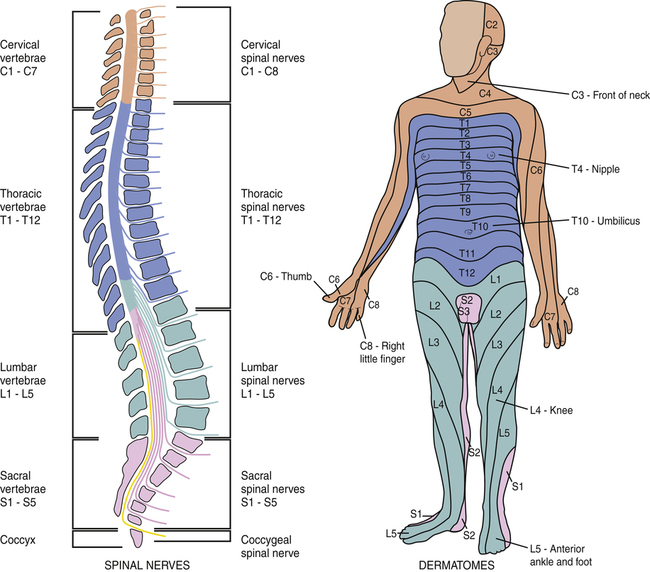
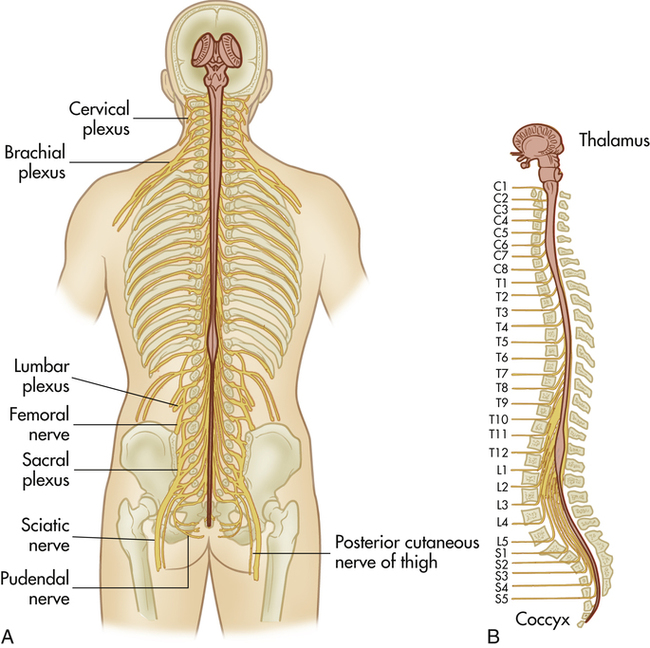
The spinal nerves combine to form the cervical, brachial, lumbar, and sacral plexuses and then innervate the limbs via peripheral nerves (Figure 11-4). Therefore peripheral nerves generally contain fibers from several different spinal nerves. Dermatomes represent the area of skin supplied by a specific spinal nerve and are clinically significant in diagnosing the sensory area of nerve injury (Box 11-2). Nerve injury needs to be distinguished from the cutaneous innervation of the peripheral nerves. A myotome is a muscle or group of muscles supplied by one ventral (motor) nerve. Motor deficits may be attributed to damage in specific myotomes.
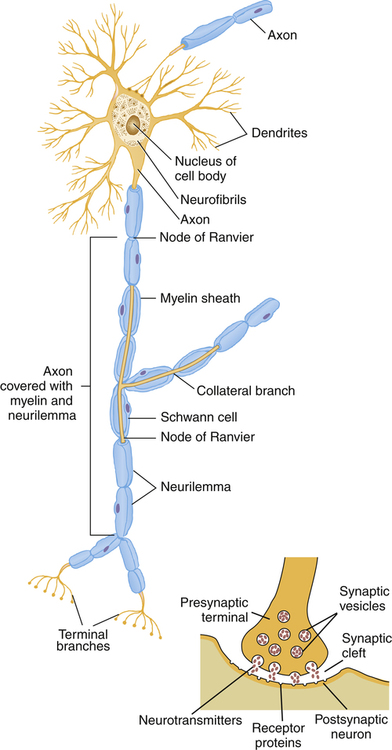
Myelination is a process in which a nerve is enveloped in a myelin sheath. In the peripheral nervous system, this is accomplished by the encircling of a nerve axon by Schwann cells. Gaps between the Schwann cells are called the nodes of Ranvier (Figure 11-5) and expose unmyelinated axons. The significance of this is that nerve conduction in these myelinated nerves is saltatory, jumping from node to node, which increases the conduction velocity.1 This type of myelination ceases just before the interface of the dorsal or ventral nerve root with the spinal cord. At this juncture between the peripheral nervous system (PNS) and the central nervous system (CNS), known as the Obersteiner-Redlich zone, astrocytes and oligodendrocytes form the myelin covering.
Assessment of the Neurological System
Warning Signs of Neurological Diseases
The physical examination of the athlete begins with a visual inspection of the spinal column, assessing for deviations, muscular imbalance, or surgical scars. The athlete’s musculature, although typically stronger on the dominant side, should not be particularly unilaterally hypertrophic. The health care provider assesses bilaterally for tremors, atrophy, and muscular tone. The dermatomes are bilaterally assessed for sensation as described in Chapter 2, followed by bilateral comparison of the reflexes. Evaluation of the cranial nerves (described in the next section) and muscular strength tests follow. Muscular strength tests include both range of motion and break tests for the brachial plexus as well as heel and toe walking for the lower extremities. The practitioner notes any weakness or differences and refers the athlete to a physician when a discrepancy occurs in either. Functional knowledge of the myotomes and dermatomes is instrumental in assessment of any neurological issue. The physical examination for SRC should include the assessment of cognition and coordination (balance) along with the aforementioned evaluation of strength, myotomes, and dermatomes.
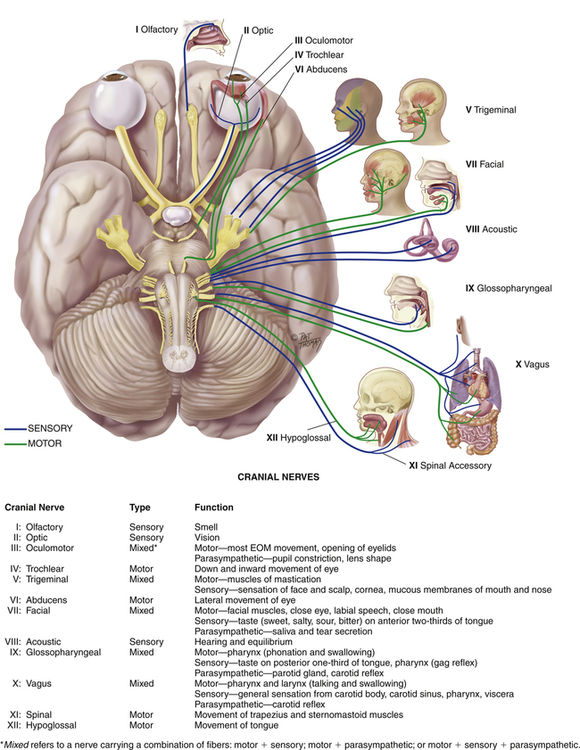
Understanding the basic anatomy and physiology of the neurological system also helps in identification of injury to higher neurological systems. Cerebral injuries may present with aphasias, apraxias, paresis, paralysis, sensory deficits, and visual and auditory dysfunction. Cerebellar damage leads to varying degrees of ataxia and incoordination, as well as dysmetria and tremors. Neurological injury to the brainstem may manifest with cranial nerve palsies (CN III to CN XII). In addition to these symptoms, many other common signs associated with neurological disease have special terminology (Box 11-3).
Cranial Nerves and Cranial Nerve Testing
The cranial nerves emerge from the cranium, as opposed to spinal nerves, which emerge from the spinal cord (Figure 11-6). The cranial nerves provide sensory and motor innervation to the head and neck, including voluntary as well as involuntary muscle function, and sensation (see Table 2-4, Cranial Nerve Function). Testing these nerves is essential to ascertaining their integrity as well as noting discrepancies that may indicate a medical condition.
nerve are usually unilateral. The clinical spectrum of pathology can range from normal function to anosmia, in which the patient can discern only ammonia, to organic dysfunction, in which the patient cannot recognize any smells.
The optic nerve (CN II) carries visual information within the complex visual system. The fibers of the optic nerve carrying information from the right half of the retina cross over and join with those same fibers of the contralateral optic nerve. Together, these fibers form the optic tract. The optic tract then forms optic radiations that eventually synapse on the primary visual cortex. Different clinical visual defects will occur depending on the area of lesion within the optic pathway.1 Complete assessment of the optic nerve requires testing the visual fields, acuity, and pupillary light reflex.
To test the visual fields, the health care provider faces the athlete, who is looking straight ahead. The athletic trainer moves the fingers of one hand within the athlete’s peripheral vision and monitors the athlete’s response about which finger is moving. Next, the practitioner focuses on individual eye deficits by repeating this test while the athlete closes one eye. The Snellen eye chart, which is described in Chapter 12 is used to test visual acuity. Alternatively, the athlete may be asked to read something.
The trochlear (CN IV) and abducens (CN VI) nerves can also be tested by monitoring the movements of the extraocular muscles. The athlete is asked to visually follow a pen as it is slowly moved within the visual field. Then the athletic trainer passes the pen across the midline space toward the athlete’s nose, watching for movement of both eyes in toward the midline and testing for convergence. Saccadic eye movements are tested by having the athlete look in each direction and watching the coordination and quality of movement. Specifically, the trochlear nerve (CN IV) is responsible for upward eye movement and the abducens nerve (CN VI) coordinates eye movement laterally away from the nose (Figure 11-7).
The health care provider tests response of the trigeminal nerve (CN V) and the facial nerve (CN VII) by observing for symmetry when the athlete bares teeth, whistles, looks up at the ceiling, and clenches eyes closed (Figure 11-8). Sensory testing of the trigeminal nerve is performed with light touch and pinprick in the divisions of the trigeminal nerve on both sides. If any abnormalities are found, further tests are warranted. When testing the motor function of the trigeminal nerve, the athletic trainer has the athlete clench teeth while placing a hand under the athlete’s chin to resist jaw opening. Any noticeable muscle atrophy or elicited muscle weakness indicates an abnormal test. Sensory testing of CN VII as well as CN IX (glossopharyngeal) appraises the athlete’s ability to distinguish taste. For example, the athlete might be asked to tell the difference between sweet and sour.
Testing of the vestibulocochlear nerve (CN VIII) involves auditory testing of hearing and equilibrium. Auditory testing is performed using the Rinne test and the Weber test (see Box 13-2). In both tests a vibrating tuning fork is placed at various points on the patient’s head and the patient is asked to identify which placement is louder. Conductive deafness occurs when conduction of sound is impaired, as opposed to sensorineural deafness, in which there is neurological disruption. Auditory testing may also be conducted by creating a sound—such as snapping fingers—behind each of the athlete’s ears and looking for a response.
The athletic trainer tests the spinal accessory nerve (CN XI) by focused examination of the sternocleidomastoid and trapezius muscles on both sides of the body. The strength of the trapezius muscle is assessed through a resisted shoulder shrug (Figure 11-9), and the sternocleidomastoid muscle is assessed by resisting both turning and lifting of the chin. The presence of atrophy or weakness during resisted muscle movement suggests nerve injury.
Pathological Conditions
Brain and Spinal Cord Disorders
Sport-Related Concussion
Sport-related concussion (SRC) is a common injury in recreational activities and sports that may have possible short- and long-term sequelae. Reports have estimated that approximately 1.6 to 3.8 million SRCs occur annually.1 It is also speculated that these numbers may be higher due to those SRCs that are not recognized by the athlete, and thus not reported to medical personnel.2–4 Data from two national injury surveillance systems found that concussion represented 8.9% of all high school and 5.8% of all collegiate athletic injuries.5
An evidence-based definition was published after the Third International Conference on Concussion in Sport, held in 2008.6 This definition, provided in Box 11-4, is more comprehensive in nature and identifies clinical, pathological, and biomechanical features of concussion that are important in identifying these injuries.6 It was found that an unacceptably high percentage of high school players were playing with residual symptoms from a prior head injury7 (Figure 11-10).
Signs and Symptoms
The health care provider should be able to identify signs and symptoms associated with SRC. These signs and symptoms are often categorized as somatic (physical), emotional, cognitive, and sleep-related.8 Box 11-5 lists the specific symptoms that warrant referral to a medical facility. Each athlete may present differently with respect to the severity and duration of reported symptoms. In a National Collegiate Athletic Association (NCAA) concussion study,9 there was an increase in reported symptoms immediately after concussion, followed by a gradual decrease in symptom complaints throughout the first week, with 91% of athletes returning to their baseline symptom levels by day 7 postinjury. Headache is the most common symptom reported and tends to last the longest.10–12
Differential Diagnosis and Referral
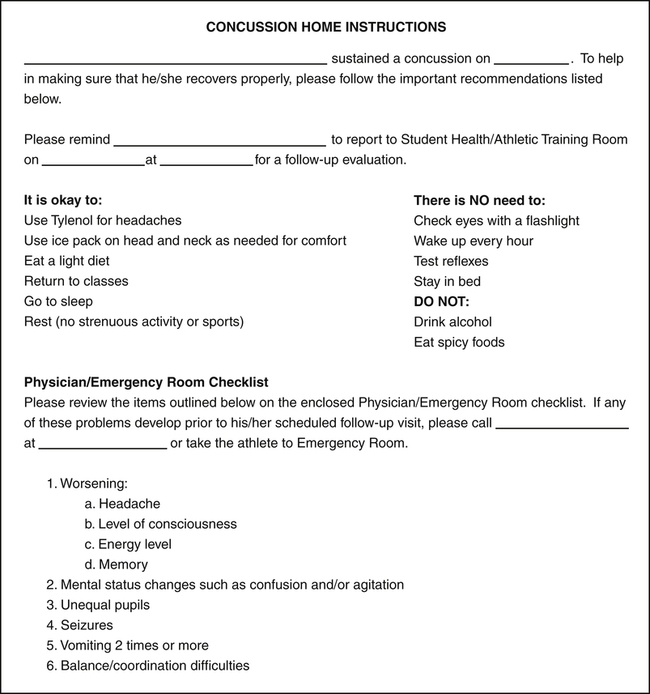
As part of the initial assessment of SRC, the health care provider should attempt to rule out more severe head injuries including skull fracture, cerebral contusion, and epidural hematomas.6,7,13,14 Assessment of these injuries may reveal acute localized swelling, deformity, prolonged loss of consciousness (LOC), irretractable vomiting, and frequently, multiple positive neurological examination findings such as cranial nerve abnormalities and motor or sensory weakness. Positive findings during an initial examination for one or more of these indications should warrant immediate transfer to an emergency department capable of managing a neurosurgical emergency.13 In addition, the clinician should continue to monitor the athlete for any signs of altering or deteriorating condition in the acute injury phase and throughout the first week postinjury that would increase suspicion of a subdural hematoma. Patients should be given a home instruction form that lists the red flag warnings for immediate referral and other information about home care of the SRC (Figure 11-11).
Physician referral is also indicated for athletes who are not experiencing a typical recovery, for those who may still be symptomatic in the weeks after their initial injury, and for those who demonstrate an increase in symptoms in the postacute phase. At this time, referral to a specific specialty may be necessary. For example, an athlete with sleep disturbances may benefit from a referral to a neurologist, whereas an individual with cognitive difficulties may be best suited for a referral to a neuropsychologist.13
Diagnostic Tests
Because SRC is a functional injury and does not normally include structural injury to the brain, most diagnostic tests will result in negative imaging findings, thus making neuroimaging of little value for most SRCs.6,7,13 Suspicion of an intracranial hemorrhage or hematoma should result in immediate referral for a computed tomography (CT) scan, Functional magnetic resonance imaging (MRI), or other imaging study. Moreover, the sudden presence or deterioration of symptoms that had previously resolved or had remained stable necessitates neuroimaging for a subdural hematoma, which may not be noted on a CT scan or MRI for 1 to 2 weeks after the initial concussion.13 However, it is imperative to understand that a negative imaging finding does not rule out an SRC and should not be used to prematurely return a patient to activity.
Assessment and Management
The assessment of SRC should begin off-season or during preseason in conjunction with the preparticipation physical examination (PPE) to obtain an adequate concussion history and to assess baseline measures of symptom reports, postural stability, and neurocognition. The PPE should include a thorough neurological injury history, including a history of sport-related concussion and other concussive injuries (e.g., motor vehicle accidents, falls).15,16 The PPE should contain an adequate series of questions regarding concussion history, including queries about perceived previous concussions and those focusing on earlier concussion-related symptoms sustained during both sport and nonsport activity.6,15,17 Knowledge of an athlete’s concussion history is important as research has demonstrated a relationship between previous concussions and increased risk for sustaining subsequent injuries.18–20 In addition, baseline measures of symptoms, neurocognitive function, and postural stability should be obtained from the athlete when he/she is in a healthy state for future comparison with postconcussion scores.
After a concussion, the athlete should be assessed immediately for symptom reports, mental status, and postural stability. Serial assessments using the tools described below should take place at planned intervals (postgame, 24 and 48 h postinjury) to assess the athlete’s recovery (Box 11-6). Once the athlete reports that he/she is symptom free, the more complex neurocognitive assessments should be administered to determine whether cognitive recovery has occurred as well. Scores on all assessment tools should meet or improve on baseline scores before a return-to-play progression is begun.