45 Neck Pain
Epidemiology
Pain is an evolutionary protective mechanism to prevent further tissue damage. Neck pain is a ubiquitous condition with a lifetime prevalence of 67% to 71%.1 The point prevalence of neck pain ranges between 10% and 15%, with total annual costs for neck and low back pain corresponding to 1% of the gross national product (GNP) in Sweden, and direct health service costs representing only a small fraction of this percentage.2–4 The medical and legal expenses associated with neck pain can be enormous, as in whiplash injuries, which alone can cost $29 billion annually in the United States.5
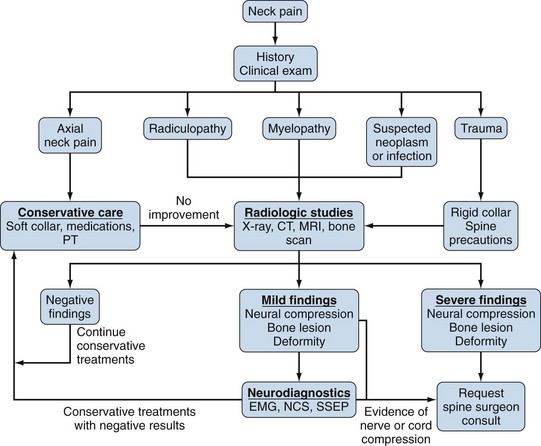
Neck pain may originate from various anatomic sources, including paraspinal soft tissues, intervertebral joints and disks, compression of the spinal cord or nerve roots, and referred visceral pain (Figure 45-1). The origin of neck pain has a wide differential diagnosis, which can include trauma, degenerative changes, infection, and autoimmune disorders such as rheumatoid arthritis and ankylosing spondylitis.
The perception and resultant reporting of this pain vary significantly according to cultural and social circumstances. Honeyman and Jacobs noted that Australian Aborigines significantly underreport pain and are rarely disabled by pain.6 Social circumstances also play an important role in an individual’s ability to cope with and overcome neck pain. Studies have demonstrated worse outcomes following diskectomy for patients with a workers’ compensation claim or litigation surrounding their condition.7 These studies indicate nonorganic contributions to neck pain for secondary gain. Fortunately, most episodes of acute neck pain resolve with “tincture of time” and patient education.
Anatomy
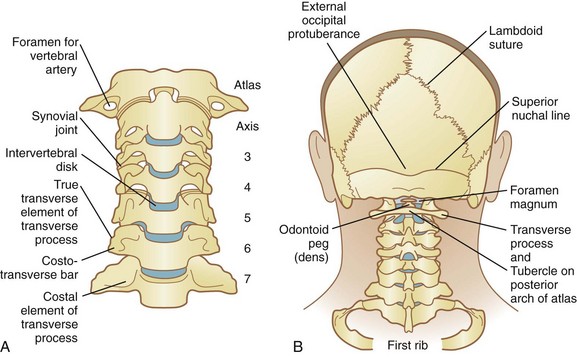
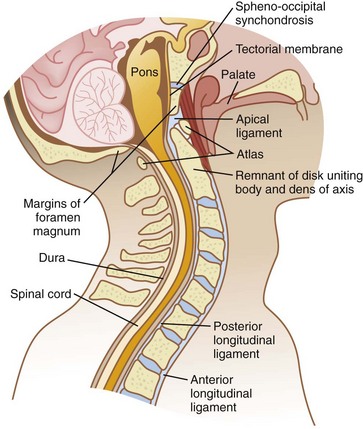
The cervical spine consists of seven vertebrae (C1 through C7). The bony anatomy of the atlas (C1) and axis (C2) is unique, whereas C3-C7 demonstrates fairly consistent anatomy (Figure 45-2). The atlas has no vertebral body, and its lateral masses articulate with the occipital condyles of the skull, forming the atlanto-occipital joints supported by anterior and posterior occipital membranes.8 The atlanto-occipital joint is responsible for approximately 50% of total flexion and extension in the neck, and functional implications are clear when this motion is lost. The axis (C2) has the dens or an odontoid peg that projects upward and anterior to articulate with the posterior aspect of the anterior arch of the atlas. The principal stabilizer of the odontoid to the anterior arch of the atlas is the transverse ligament; alar and apical ligaments act as secondary stabilizers. This true synovial joint is susceptible to inflammatory processes such as those seen with rheumatoid arthritis. No intervertebral disk is present between the atlanto-occipital joint and the atlantoaxial joint, and without conferred stability from a disk, destructive inflammatory arthritides may result in instability.9 The atlantoaxial articulation provides approximately 50% of rotatory motion of the cervical spine.
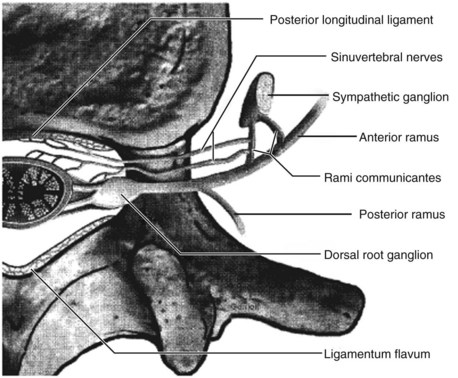
Intervertebral disks increase in size from C2 downward, giving the cervical spine its characteristic lordotic shape. Each disk consists of an outer annulus fibrosus and an inner nucleus pulposus, as well as cephalad and caudad end plates. The annulus fibrosus consists of type I collagen, which helps give form to the disk and provides tensile strength. The annulus fibrosus is innervated by the sinuvertebral nerve, formed by branches of the ventral nerve root and the sympathetic plexus.10 The nucleus pulposus consists of type II collagen and proteoglycans, which interact with water to resist compressive stress. Pressure within the disk is greatest with flexion, which may explain why those with a disk herniation find this position most uncomfortable.11 Disk degeneration with aging includes loss of water content and resultant loss of height, annular tears, and myxomatous changes, increasing the risk of disk herniation. This typically occurs in the posterolateral aspect of the disk, where the posterior longitudinal ligament is not present and annulus fibrosus is at its weakest, medial to the uncovertebral joints.
The spinal column is supported by the interplay of ligaments and muscles (Figure 45-3). The anterior longitudinal ligament (ALL) and the posterior longitudinal ligament (PLL) course along the anterior and posterior aspects of the vertebral bodies; the anterior longitudinal ligament resists hyperextension, and the posterior longitudinal ligament resists hyperflexion. The ligamentum flavum joins the laminae of adjacent vertebrae and may become thickened, creating stenosis in the spinal canal. In a similar manner, the interspinous ligament joins the spinous process of adjacent vertebrae. The supraspinous ligament originates as the nuchal ligament at the occiput and extends caudally as an aponeurosis until it is attached to the tip of the spinous processes of C7; it then continues to the lumbar region. Fourteen paired anterior, lateral, and posterior muscles help to orchestrate complex movements of the neck.
A brief review of the spinal cord and nerve roots is beneficial for a thorough evaluation. Grossly, the spinal cord is divided into the posterior column, the lateral column, and the anterior column. The posterior column mediates proprioceptive, vibratory, and tactile sensation; the lateral column is a conduit for motor fibers, along with pain and temperature sensation from the contralateral side of the body; the anterior column conveys crude touch sensation. Eight total cervical nerve roots are present as the dorsal and ventral roots converge to form the spinal nerve within the vertebral foramen. Cervical nerve roots enter the intervertebral foramina by passing over the top of the corresponding pedicle, except the C8 cervical nerve, which lies between C7 and T1. Therefore, C5-C6 posterolateral disk herniation will affect the C6 nerve root. The nerve root occupies approximately one-third of the foramen (Figure 45-4). Space available for the nerve root is decreased with neck extension and degenerative changes, and is increased with neck flexion.
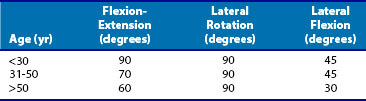
The cervical spine is the most mobile segment of the spine; an approximate 90-degree arc of motion occurs in flexion and extension, three-quarters of which is due to extension (Table 45-1). The maximal range of motion in the sagittal plane within the subaxial spine is seen at the C5-C6 level, making this a common site of disk degeneration. Rotation encompasses approximately 80 to 90 degrees of motion, and 50% of this occurs at the atlantoaxial joint. As is seen with extension, rotation reduces the cross-sectional area of the spinal canal. The cervical spine demonstrates 30 degrees of lateral mobility in each direction; this typically occurs with some degree of rotation secondary to the orientation of the facet joints.
Axial Neck Pain
Axial neck pain may originate from any tissue that receives innervation, including zygoapophyseal joints, cervical disks, vertebral periosteum, posterior neck muscles, cervical dura mater, occipito-atlantoaxial joints, and vertebral arteries. Sources may include degenerative, traumatic, malignant, infectious, or systemic inflammatory processes. Zygoapophyseal joints and cervical disks have the greatest quantity of direct supporting data suggesting these sites as the origin of axial neck pain. Provocative injection into the facet joint in asymptomatic volunteers invokes a reproducible pattern of occipital or axial neck pain.12 This pattern of pain can be accurately diagnosed and treated for at least a short time with anesthetic injections targeted at the joint capsule itself, or with blockage of the respective dorsal primary ramus.13–15 Degenerative arthritis within the upper cervical spine can manifest as suboccipital headaches denoted as cervicogenic headaches, which are thought to result from irritation of the greater occipital nerve. Typically, arthritis within the atlanto-occipital joints is made worse by provocative neck flexion and extension, whereas atlantoaxial arthritis is made worse by rotation. This is supported by investigators who injected asymptomatic volunteers at the atlanto-occipital and atlantoaxial joints, reproducing this pattern of pain.16 Relief of suboccipital pain may be attained with fluoroscopically guided injection of corticosteroid into the diseased joint, or fusion of these joints in recalcitrant cases.
The cervical disk is a controversial source of axial neck pain, which occurs as the result of insult to the highly innervated annulus fibrosus. This idea is based on provocative diskography, whereby a diseased disk is fluoroscopically injected to a given pressure, and pain is reproduced in reliable patterns. In a true-positive or concordant study, an adjacent normal disk should not produce pain when injected. Using this method, several studies have implicated cervical disks as the source of axial neck pain.17–19 Even with careful technique, a false-positive result can occur, and it is not unusual to have a nonconcordant study in which multiple disks elicit a pain response despite being normal.17 Interventions directed at treating the disk for isolated axial neck pain have been found to be unpredictable, although the cervical disk is likely to contribute to axial neck pain.
Myofascial pain due to irritation of the muscles about the neck can contribute to axial neck pain. Patients with chronic myofascial pain have been shown to have a lower level of high-energy phosphates in involved muscle tissue.20 Myofascial pain can be the original source of neck pain or, more commonly, a manifestation of postural adaptations and compensatory overuse of normal tissue that remains after the injured structure heals. A more generalized form of this is fibromyalgia, a widespread disorder defined by diffuse pain affecting all four quadrants of the body, with at least 11 of 18 pressure points noted as positive. Patients have associated symptoms of fatigue, cognitive difficulties, and irritable bowel syndrome, and a nondermatomal pattern of dysesthesias, weakness, and paresthesias.21
Systemic inflammatory arthropathies causing neck pain typically demonstrate the classic pattern of morning stiffness, polyarticular involvement, rigidity, and associated cutaneous manifestations. Rheumatoid arthritis (RA) often involves the cervical spine, initially causing stiffness and later causing pain, potentially leading to instability. After the hands and feet, the cervical spine is the most common site of disease involvement in RA.22 The upper cervical spine is most commonly involved (occiput to C2), followed by the subaxial cervical spine (C3-C7). The likelihood of developing cervical spine pathology can be predicted by the extent of rheumatoid changes that occur in the hands and feet. Basilar invagination is one such manifestation, whereby C1 lateral masses erode, allowing the odontoid peg to settle into the foramen magnum, placing pressure on the brain stem with potential for instantaneous death. The atlantoaxial joint can demonstrate instability with potential for neurologic injury. Because of these potentially catastrophic complications, dynamic radiographs of the cervical spine should be obtained before any procedure requiring intubation is performed. Seronegative spondyloarthropathies that can manifest with neck pain include ankylosing spondylitis, psoriatic arthritis, and reactive arthritis. In 70% of patients, psoriatic arthritis will manifest with skin lesions before arthritis develops; reactive arthritis rarely involves the cervical spine.
Infection and neoplasms can cause axial neck pain through bone destruction with irritation of vertebral body periosteal nerves and altered biomechanics of the facet joints and cervical disks. The onus is upon the clinician to identify these patients at the initial visit because a delay in diagnosis can have catastrophic consequences. Red flags for axial neck pain that require further workup at the initial presentation include elderly patients, patients with a history of malignancy, immunocompromised patients, and those with fever, chills, unexplained weight loss, fatigue, nighttime awakening, recent antecedent bacteremia, and severe nonmechanical neck pain.21
Radiculopathy and Myelopathy
In radiculopathy, mechanical distortion of the nerve leads to increased vascular permeability, resulting in chronic edema and eventually fibrosis. This causes hypersensitivity of the nerve root with an inflammatory response mediated by chemicals released from the cell bodies of sensory neurons and cervical disks.23 Compression of the dorsal root ganglion is felt to be especially important in producing radicular pain.24 Clinically, this presents with pain in a dermatomal distribution; dermatomes for the higher cervical nerve roots, including C3 and C4, are found along the posterior scapula, and the pain should not be confused with isolated axial neck pain.25 Minor symptoms that are tolerable may be treated with conservative care, but persistent compression on a nerve root can lead to sensory loss and weakness. Disabling deficits should be treated operatively given that prolonged nerve compression can result in irreversible changes. In patients without a neurologic deficit, it is reasonable to expect a good outcome with conservative care.26
Myelopathy has a clinical presentation of long tract signs resulting from compression of the spinal cord. Factors that contribute to the development of myelopathy include a congenitally narrow spinal canal, dynamic cord compression, dynamic thickening of the spinal cord, and vascular changes. The anterior-posterior diameter in the subaxial spine for a normal adult measures 17 to 18 mm. The cord measures 10 mm, and diameters less than 13 mm are considered to be congenitally stenotic. The shape of the spinal cord deformity has a strong association with the development of myelopathy; patients with a banana-shaped cord on axial views had evidence of myelopathy 98% of the time.27 Ono and associates described a ratio whereby the anterior-posterior diameter of the spinal cord is divided by the transverse diameter of the cord. Patients with a ratio of less than 0.40 tended to have severe neurologic deficits.28 Patients may have dynamic cord compression with signs and symptoms of myelopathy only during neck flexion and extension. The space available for the cord is decreased during neck extension owing to infolding of the ligamentum flavum and overlapping of the lamina. In addition, the spinal cord shortens during neck extension, effectively increasing the diameter and making it more prone to compression by posterior structures. In flexion, the cord lengthens and drapes over anterior degenerated disks and osteophytes.29
Myelopathy can be exacerbated by altered biomechanics from degenerated segments, as when a given level stiffens, the level above can become hypermobile.30 A certain subset of patients can develop myelopathy in the absence of mechanical compression; this has been attributed to ischemic insult.31 It has been shown in a canine model that in the setting of spinal cord compression, additive ischemia results in significantly worse outcomes, because over time the spinal cord demonstrates permanent irreversible changes.32 Patients with mild cases of myelopathy that does not affect activities of daily living can be closely followed.33 Those with more severe deficits or progressive deficits tend to deteriorate over time with conservative care, and it is recommended these patients should undergo surgery to decompress the spinal cord.34
Clinical Features
In terms of functional anatomic pathways, neck pain is mediated via somatic or autonomic pathways.35 Somatic pain is the most common, being perceived in dermatomes, myotomes, or sclerotomes. Pain originating in the autonomic pathway, or in the sympathetic nervous system, may fall into somatic segmental distributions, vascular supply distributions, peripheral nerve distributions, or nonconforming patterns. Because pain mediation pathways may have significant overlap, additional clinical information regarding characteristics of neck pain, along with diagnostic studies, complements the determination of pain origin when localization based on functional anatomy is not sufficient.
Patient History
Articular symptoms arise from innervation to the facet and uncovertebral joints causing local pain and stiffness. Patients often state that their symptoms are made worse with inactivity and describe feelings of clicking, grating, or “sand” in the neck. Pseudoarticular pain may be felt in the shoulder and elbow, with true pathology originating from the neck. Vascular symptoms result from compression of the vertebral artery by osteophytes or a protruding disk. Symptoms may intensify with neck movement or with certain postures. Tenosynovitis and tendinitis may involve the rotator cuff and tendons about the elbow, wrist, or hand. Stenosis or fibrosis of tendon sheaths or palmar fascia may be present, along with trigger points over the affected joints, giving a false impression of local pathology.36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree