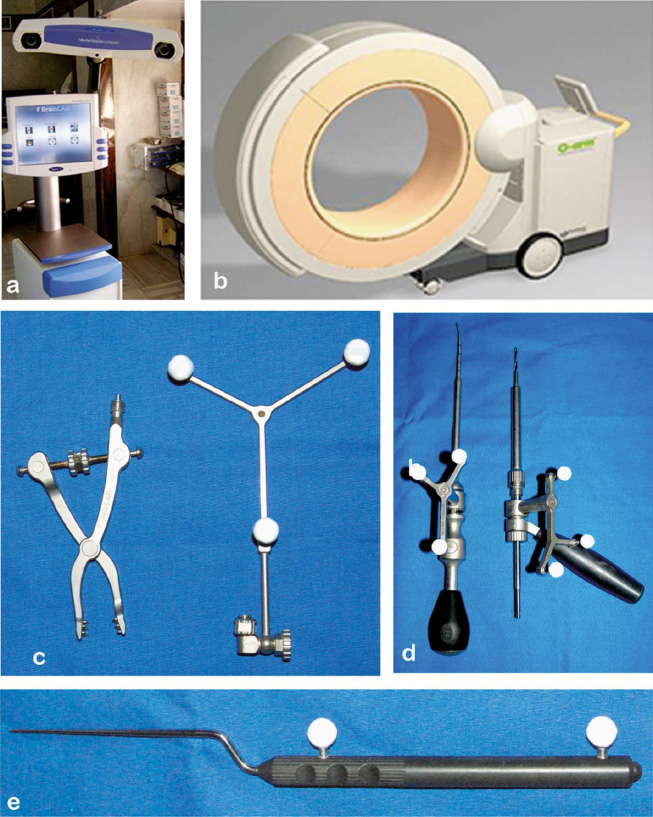
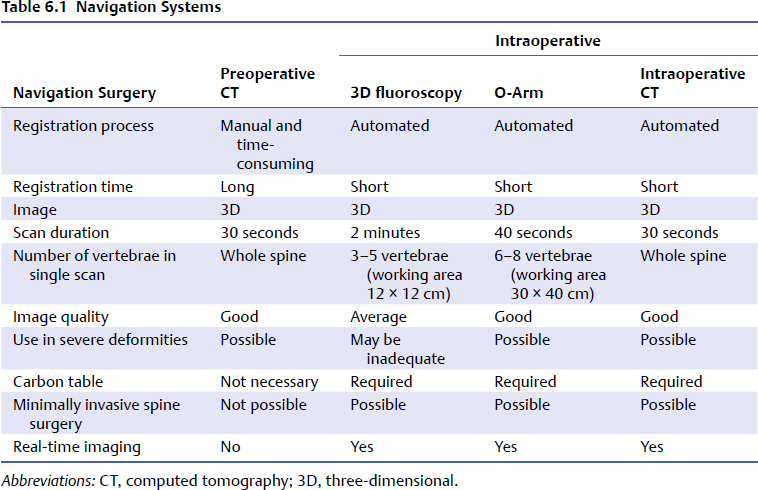
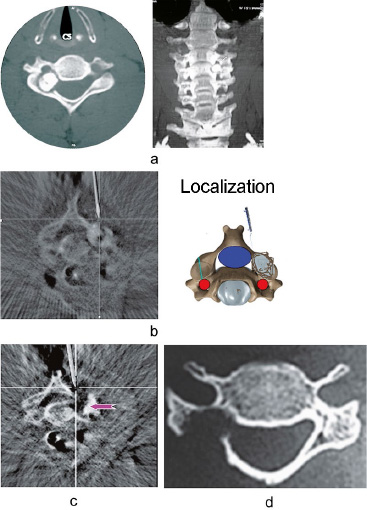
6 Spinal instrumentation has become an integral part of spine surgery, as it augments the spine surgeon’s ability to achieve stability, correct deformity, and increase the rate of fusion. The traditional stabilization techniques, which use loops, wires, and lateral mass screws, have a poor healing potential and may need to be supported with an external orthosis. Pedicle screw fixation has the advantage of providing three-column fixation, better mechanical stability, and better deformity correction. However, its use in the cervical spine has certain inherent problems due to the smaller size of the osseous elements, the inconsistent anatomic landmarks, the high incidence of anatomic variations, and the close proximity of vital neurovascular structures to the screw trajectory. Achieving accurate screw placement is additionally challenging in patients with altered spinal anatomy, in children requiring spinal instrumentation, in patients requiring revision surgery, and in conditions such as ankylosing spondylitis where the anatomic landmarks are obliterated. In the upper cervical spine, a high incidence of anatomic variation of the osseous and vascular anatomy has been observed. In a multicenter study on C1–C2 fusion involving 102 adult patients, Aryan et al1 were unable to identify the C2 pedicle in 23 patients (22%). Abumi et al,2 using the conventional technique of cervical pedicle screw insertion, reported a perforation rate of 6.8% (45 of 664 screws) with only two screws causing radiculopathy. The malposition of the screws can have multiple implications, including poor stability of the fixation, potential damage to the neurovascular structures, and medicolegal implications. Safety concerns regarding the violation of the spinal canal, leading to potential harm to vascular and neural structures, has prompted the development of spinal navigation techniques to increase the safety of instrumentation. Spinal navigation is a computer-based technology that improves the surgeon’s intraoperative orientation to the unexposed anatomy during spinal procedures, practically enabling vision beyond what the human eye can usually see. The technology merges the three-dimensional images of the spine acquired either preoperatively or intraoperatively with that of the surgical instrument, enabling the surgeon to visualize in real time the exact position of the hand-held instruments in relation to the bony anatomy. Spinal navigation, in addition to improving the surgeon’s hand–eye coordination and accuracy of implant placement, also reduces the entire surgical team’s radiation exposure and shortens the surgical time. Apart from increasing the accuracy of screw placement, spinal navigation also has applications in ensuring complete excision of tumors and in planning of osteotomies. The currently available spinal navigation systems share the same basic principles and components, with differences mainly in the manner in which the images are acquired, processed, and presented to the surgeon. The basic components are (1) the system of image acquisition and processing, and (2) an image-processing computer workstation interfaced with a two-camera electro-optical localizer. The basic component of any navigation system is the referencing device, the dynamic reference array (DRA), which is attached to the patient during navigation. The DRA is attached to a fixed point on the patient, which is usually the spinous process. Alternately, in patients with absent posterior structures, the DRA can be attached to a Schanz pin placed in the pedicle or a neighboring bony structure at the iliac crest. The light-emitting diodes (LEDs) are attached to the DRA and can be tracked by an electro-optical camera. The LEDs are called the active arrays, as the light emitted by them is recognized by the electro-optical camera. The reflective spheres reflect the infrared rays emitted by the camera and hence are called passive arrays (Fig. 6.1). Specialized instruments (screw drivers, probes, drill guides, etc.) can be fitted with reflective spheres and used for navigation. The infrared light that is transmitted from or reflected by these instruments is relayed to the computer workstation, which calculates the precise location of the instrument tip in the surgical field as well as the location of the anatomic point on which the instrument tip rests.3 The acquisition of three-dimensional anatomic images of the operative field of interest is the first step in navigation surgery. Image acquisition can be preoperative or intraoperative and can be accomplished with either fluoroscopy or computed tomography (CT). • CT-based image guidance • Preoperative • Intraoperative • Fluoroscopy-based image guidance • Two-dimensional (2D) fluoroscopy • Three-dimensional (3D) fluoroscopy The CT scan of the planned surgical level is acquired preoperatively using thin contiguous 1- to 3-mm slices. The data are then loaded onto the computer workstation, which then reconstructs the axial, coronal, and sagittal views of the spine. The images are then referenced to the patients spinal anatomy through a fixed frame (DRA), which is firmly attached to the spine (usually to the spinous process). This is then followed by registration, which is performed using the registration probe fitted with LEDs by pairedpoint matching and surface matching techniques. This information enables the computer workstation to create a contour map of vertebrae, thus providing 3D visualization of the spine. This technique completely eliminates the surgical team’s intraoperative radiation exposure and delivers high-quality images even in patients with obesity, osteoporosis, or a deformity. However, this technique has several disadvantages. The preoperative CT scan should be done using a specific protocol, so if the patient had already had a CT scan, this need for a new scan entails additional cost and radiation exposure. The registration process is done manually and is time-consuming; also, it may need to be repeated depending on the number of vertebrae to be instrumented. Because the data acquisition is done with the patient in the supine position, the changes in position required during intraoperative positioning can lead to navigational inaccuracy and the need for repeated registration and verification of accuracy at every single level of instrumentation. Fig. 6.1a–e Two of the most commonly used navigation platforms: (a) the isocentric C-arm–based three-dimensional (3D) fluoro-navigation station, and (b) the O-arm. Some of the essential navigation instruments are also shown: (c) dynamic reference array (DRA) with attached light emitting diodes; (d) calibrated drill bit and pedicle probe; and (e) the navigation probe. This technique merges the standard 2D C-arm fluoroscopy with image-guided navigational technology. Anteroposterior, lateral, and oblique views are obtained with a fluoroscope with an attached calibration target. The images are then automatically transferred to the image-processing computer workstation, which then correlates the data with the intraoperative spinal anatomy. The main advantage of virtual fluoroscopy is that it uses the standard C-arm image intensifier, which is familiar to the surgeon and the operating room personnel. However, this technique is contraindicated and rarely used in cervical spine surgery Because it provides only 2D imaging with no axial images. But the complexity of cervical spine anatomy requires high-quality axial images; thus, the role for this technique in cervical spine surgery is limited. This technique utilizes an isocentric C-arm fluoroscope with an image-guided navigational technology to acquire the image by automatically rotating around the patient through a 190-degree arc while maintaining the relevant area of spine in its center. Isocentricity ensures that the center of rotation is precisely maintained on the spine while the C-arm is moved angularly in the orbital direction and good-quality axial images are provided. Image acquisition can be acquired in the high-resolution mode in 2-minute cycle (100 image acquisitions) or in low resolution mode in a 1-minute cycle (50 image acquisitions). The registration frame attached to the isocentric C arm and the DRA attached to the patient are continuously tracked during the process of image acquisition, thus enabling automatic registration. The images are reconstructed into sagittal, axial, and coronal formats and then directly transferred to the navigation workstation through an interface. The advantages of isocentric C-arm–based navigation include automated registration, intraoperative postpositional acquisition of images, the ability to confirm proper positioning of implants, and the ability to use it in minimal access surgery. In addition, the position of the implant and the adequacy of tumor removal can be confirmed by a postprocedural intraoperative scan. However, the quality of image is dependent on the resolution of acquired fluoroscopic images. This is a disadvantage and can affect navigation in patients with osteoporosis, obesity, or a deformity. Intraoperative CT-based navigation is an advanced state-of-the-art navigation technology that provides high-quality intraoperative images for the purpose of spinal navigation. The O-arm navigation system is one such device that uses the flat panel detector technology to improve intraoperative image acquisition and quality. The O-arm consists of an oval telescopic gantry containing the X-ray tube and the flat panel and obtains images in a 360-degree arc, and hence provides images of high resolution. In a single acquisition a field of interest of 30 × 40 cm scan be imaged, and hence the entire cervical spine and up to six levels in the adult lumbar spine can be included. The images obtained intraoperatively with a DRA attached to the patient are transferred to a workstation that performs multiplanar reconstruction and automated registration. Postprocedurally, the O-arm can be used as a stand-alone CT scanner to confirm screw placement, spine decompression, tumor resection, and alignment. The advantages include shorter acquisition time, improved resolution of the images, larger field of view, and reduced radiation exposure. Brain suite is another such intraoperative CT navigation system that combines vector vision sky navigation with an intraoperative CT scanner and an operating table with a radiolucent tabletop. The CT scanner is a sliding, 40-slice gantry with an enlarged bore diameter of 82 cm. It enables enhanced decision processing by improving surgical navigation, planning, data management, integration, and image registration. The data acquisition time is short and the whole spine can be imaged at the same time. The major limitations of intraoperative CT-based navigation are the cost as well as the space and infrastructure needed for a special operating room. A comparison of various navigation systems is shown in Table 6.1. The advances in spinal navigation and surgeons’ increasing familiarity with the system has led to the introduction of this technology in the surgery of this anatomically challenging region of the cervical spine. In the cervical spine, spinal navigation was initially used for instrumentation of the subaxial and upper cervical spine in the adults. In the past few years, refinements and advances in the technology have extended its use to decompression procedures, fixations in complex pediatric craniocervical junction problems, tumor resections, and minimally invasive surgery. These used have been made possible mainly because of the better preoperative planning and the intraoperative control provided by the navigation systems. Navigation can be used in the following parts of the cervical spine: the upper cervical spine, the craniovertebral junction, and the subaxial cervical spine. We discuss the latter area first. The other two areas are discussed later in the chapters. The traditional stabilization techniques using loops, wires, and lateral mass screws have a poor healing potential and may need to be supported with external orthosis. Lateral mass screws, though technically easier to use, provide less mechanical stability than do pedicle screws and are associated with neurovascular complications in 3 to 18%.4,5 Biomechanical studies6,7 have demonstrated better pullout strength and more stability, especially in multilevel fixation with pedicle screws when compared with lateral mass screws. Pedicle screw fixation enables multidimensional control and provides greater rigidity and improved fusion rates. After the first reported use of the cervical pedicle screw (CPS) by Abumi et al2 in 1994, excellent clinical results using the CPS have been reported for traumatic, degenerative, and congenital diseases of the cervical spine. The complex anatomy of the normal cervical spine including the narrow diameter of the pedicles, the anatomic variations in the sagittal and axial angulations of the pedicles, as well as in the course and size of the vertebral artery, makes CPS instrumentation a challenging procedure. Abumi et al,2 using conventional techniques, reported a perforation rate of 6.8% (45 of 664 screws), with only two screws causing radiculopathy. However, a later study by Ludwig et al7 reported an alarming perforation rate of 87.5% (65.6% critical perforations) using topographic guidelines, which reduced to 55% (39.6% critical perforations) when using laminoforaminotomy. Misplacement of the screws, apart from causing neurovascular injuries, can also impact the biomechanical strength of the construct. The navigation system provides additional anatomic data and thus improves the accuracy of pedicle screw fixation and reduces the risk of neurologic and vascular injury. Image guidance also enables placement of larger-diameter screws and in a more medial trajectory, resulting in increased construct stability. The clinical efficacy of a navigated CPS has been demonstrated in many clinical studies.8,9 In Kotani et al’s8 study comparing the conventional and computer-navigated techniques for CPS insertion, the rate of pedicle wall perforation was significantly lower in the computer-assisted group than in the conventional group (1.2% vs 6.7%). There was a 2% neurologic complication rate in the manual group, whereas the navigated group had no adverse events. The presence of a deformity and altered anatomy (due to congenital anomalies) adds to the difficulty in performing CPS fixation. Rajan et al10 achieved a high rate of “perfectly placed screws” (90.8% of 98 cases) and concluded that the isocentric C-arm 3D technique increased the accuracy of screw insertion in the presence of cervical deformity. Rajasekaran et al11 performed a prospective study evaluating the accuracy of pedicle screw placement in children with complex cervical deformities. Of the 55 CPSs placed, 88.3% were fully contained and 11.7% had a noncritical breach; none had a critical breach. In complex deformities, however, O-arm and intraoperative CT navigation provides better images than the isocentric C-arm 3D navigation system. We have also found navigation to be beneficial in lateral mass screw fixations in situations were the landmarks are obliterated either because of previous surgery or ankylosing spondylitis Currently, many navigation systems, in collaboration with implant manufacturers, provide navigation-ready (calibrated) instruments, Kirschner wires, and drill guide insertion instruments. These instruments provide accurate, 3D, and real-time instrument tip information, serving as an effective tool for safe and reliable pedicle screw placement in the cervical spine. We have also used navigation to localize and excise spinal tumors like osteoid osteomas and osteoblastomas through a minimally invasive approach without compromising spinal stability.12 The technology also enables verification of the complete excision of the tumor by performing a repeat intraoperative image acquisition at the end of the procedure (Fig. 6.2).
Navigation for Cervical Reconstruction Surgery
 Introduction
Introduction
 Principles of Spinal Navigation
Principles of Spinal Navigation
 Image Acquisition
Image Acquisition
Classification of Spinal Navigation
Preoperative CT-Based Image Guidance
Virtual Fluoroscopy
Intraoperative 3D C-Arm Fluoroscopy
Intraoperative CT-Based Navigation
 Applications of Spinal Navigation in the Cervical Spine Surgery
Applications of Spinal Navigation in the Cervical Spine Surgery
Application of Navigation in the Subaxial Cervical Spine
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree