4 Cervical spondylotic myelopathy (CSM) is the most common cause of spinal cord impairment in adults.1–9 Despite valiant attempts to delineate the natural history, the risk factors associated with progression, as well as the factors associated with successful nonoperative and operative treatment, our understanding of this debilitating disorder remains limited. Furthermore, although there have been efforts to investigate the pervasiveness of its occurrence, an accurate depiction of its incidence and prevalence remains fundamentally unknown.6,10,11 It is well recognized, however, that some patients show a rapid and progressive deterioration in neurologic function, whereas others plateau after an initial deterioration and show signs of improvement over time.5,12–16 The presence of degenerative changes in the cervical spine becomes progressively more common with advancing age. Spondylosis is seen in 95% of individuals over the age of 65, whereas such manifestations are observed in only 10% of 25-year-olds.17,18 The degenerative process that accounts for the insidious spinal cord injury is believed to be initiated by aberrations in the discoligamentous complex, followed by alterations in the facet capsules (the facet joint margins and the uncovertebral joints), ligamentum flavum, and capsule-ligamentous structures as well as associated reactive tissue.2,4,14,18–20 Although ossification of the posterior longitudinal ligament (OPLL) has often been described as a separate disease process, it is frequently included by many under the umbrella of CSM.8,21,22 OPLL has been implicated in 1.5% to 2.4% of the Caucasian population and 1.9% to 4.3% of the Asian population over the age of 50 years who present with cervical spine disease.19,23 In addition, segmental alignment abnormalities may also develop secondary to degenerative pathologies (e.g., degenerative disk disease) and include dynamic as well as static spondylolisthesis.1,7,24,25 The slowly progressive deterioration in the cervical structures generally results in focal “hourglass”-type restructuring of vertebral bodies whose ends project into the spinal canal, reduce spinal canal size, and result in progressive encroachment upon the spinal cord. The ensuing spinal cord compression traumatizes the cord via static factors, from blunt compression and ischemia, as well as dynamic factors arising from dynamic compression and axial tension.4,14,18,19,25–30 This process results in spinal cord injury and specifically involves inflammation, gliosis, apoptosis, and vascular disruption.14,18,27,31–33 Ultimately this can manifest in changes on magnetic resonance imaging (MRI) seen as increased T2 signal and reduced T1 signal focally within the spinal cord.18,34–36 Unfortunately, however, although these changes have been well recognized and enable the confirmation of diagnosis, it has been challenging to interpret how these changes relate to disease severity, or how they can be used to predict postsurgical outcome. Although recent evidence derived from the AOSpine–North America prospective and multicenter study on surgical treatment for CSM has shown that intervention is not only effective at arresting disease progression but also results in clinical improvement,10 it remains challenging to identify patients with mild impairment. This is largely attributable to the insidious and often painless presentation of patients, but is also due to a general lack of recognition of this clinical entity beyond specialists. Indeed, the early manifestations may include only subtle hand and gait disturbances and are often attributed by the patient to the normal aging process. The diagnosis is often made sooner if the degenerative process impinges upon a nerve root and the resulting radiculopathy motivates the patient to seek medical attention.15,30 Even then, the general lack of awareness in the medical community results in delayed diagnosis, which contributes to further impairment by the time treatment is instigated. Recent advances have been made in understanding the pathophysiological mechanisms that result in spinal cord dysfunction; however, several fundamental phenomena remain elusive. In contrast to a long-held assumption that CSM and acute traumatic spinal cord injury share similar cellular and molecular events, emerging evidence suggests that there are distinct pathological processes at play with chronic spinal cord compression.8,14 The following processes are currently understood regarding chronic spinal cord compression and distortion of spinal cord microvasculature4,37: • Endothelial cell loss • Compromise of the blood–spinal cord barrier and potential for peripheral immune cell infiltration • Neuroinflammation • Apoptosis secondary to chronic hypoxic conditions and systemic as well as innate inflammatory processes • Resultant death of neurons and oligodendrocytes Experimental evidence links the apoptotic process with ongoing compression and a reduction in the rate of apoptosis with decompression. However, it must be noted that despite the decompression of the spinal cord, apoptotic cell loss continues, demonstrating a cell death perpetuating cycle that is initiated by chronic compression. The clinical manifestations of CSM are complicated by an unpredictable and variable rate of neurologic impairment.3,31,38 This makes the task of assessing and monitoring the clinical course of this disorder with one assessment tool difficult. A combination of validated outcome measures can be used to offer the most appropriate treatment in a timely manner and assess the efficacy of surgical interventions. Kalsi-Ryan and colleagues39 recommended the use of the following outcome measures in clinical practice for screening and monitoring patients with CSM: • Nurick scale: a six-grade clinician scale focused on impairment of gait • Modified Japanese Orthopaedic Association (mJOA) scale: an 18-point clinician-based scale with measures of upper and lower limb motor function, hand sensation, and sphincter control • Myelopathy Disability Index: a self-report scale incorporating 10 functional activities • 30-Meter Walk Test: a timed walk of 30 m and a measure of cadence • Neck Disability Index: a modification of the Oswestry Disability Index that entails a selfreport of 10 activities scored from 0 to 5 The natural history of patients with CSM is generally unpredictable. Although some patients appear to have no discernible clinical symptoms in the setting of spinal cord compression, others display serious debilitation. One of the reasons for this may stem from the fact that spinal cord compression is largely measured by static imaging, and therefore dynamic factors are generally not taken into consideration. Nevertheless, it is recognized that patients tend to worsen over time. Over half a century ago, Clarke and Robinson16 reported on 120 patients with CSM, finding that 75% worsened in a stepwise fashion, with 20% slowly worsening and 5% experiencing a rapid onset of impairment followed by a stable course. More recently, the course of progression was address by a systematic review on the natural history of CSM, which concluded that based on small and moderate-sized prospective and retrospective studies, 20 to 62% of patients deteriorate (based on at least 1-point deterioration on the JOA scale).14,15 In addition to this, Wilson et al40 found that patients with cervical spine stenosis and spinal cord compression without symptoms develop myelopathy at a rate of ~ 8% at 1-year follow-up and a median of 23% at 44-month follow-up. Indeed, these findings do not seem surprising, as advancing age and progressive wear-and-tear likely contribute to cervical joint degeneration and a greater chance for spinal cord insult over time. The insidious presentation of CSM often means that patients present late, and they attribute the deterioration in their function to the natural aging process. Unfortunately, this is accompanied by a general lack of vigilance in the medical community to assess the cervical spine for degenerative changes, resulting not only in delayed intervention but also in referrals being made to specialists only when patients have profound disease severity. A careful history will elicit a picture of vague symptoms with ambulation and hand dexterity difficulties. Gait abnormalities manifest with balance difficulties, loss of confidence on uneven surfaces, increasing reliance on walking aids, and a reduced ambulation distance from the home. Changes in hand strength and dexterity are a common early clinical manifestation. A loss of hand function manifests with clumsiness or difficult performing fine motor skills such as picking up small coins, manipulating buttons on clothing, and deteriorating hand writing.19,30 Many patients also confess to alteration in bladder function when questioned directly. This often includes symptoms of urgency and frequency.30 Clinical manifestation of spinal cord compression can vary considerably among patients in the degree of sensory, motor, and autonomic dysfunction. These findings may precede changes seen on complex imaging studies. Generally, patients with CSM present with upper motor neuron signs in the lower limbs that may include increased tone, hyperreflexia, altered plantar response, myoclonus, weakness, and sensory changes.2,15,18,19,31,33,41–46 On the other hand, the clinical presentation in the upper limbs can be variable and depends on the location and extent of the compressive pathology. For instance, a focal C6/7 compressive lesion may present with mixed upper and lower motor neuron findings in the upper limbs with normal deltoid and biceps function, wrist extension flaccid paralysis, and triceps and hand musculature spasticity.30 Gait abnormalities are also common, and their early manifestation may be a useful and sensitive tool to direct patients for further investigation. The gait pattern commonly includes a broad-based stance with reduced reciprocal fluency and a shuffling pattern. The ability to ambulate at speed is impaired, and making changes in direction require additional small stepping maneuvers. Patients may present having sourced their own walking aids due to a reduction in walking confidence.30,39,46 Fig. 4.1a,b Preoperative lateral (a) and anteroposterior (AP) (b) plain cervical X-rays. An assessment of cervical spine alignment and segmental instability should be made. Flexion and extension views may help clarify segmental instability, reversibility of cervical kyphosis if present, and degree of spinal canal compromise. Additionally, congenital fusion of vertebrae can also be easily appreciated upon inspection (not present here). A 62-year-old male retired laborer with 1-year worsening history of: • Unsteady gait • Fine motor skills • Pain in both arms • Urinary frequency and urgency Significant for: • Wide-based difficult tandem gait • Hoffman’s sign positive bilaterally Fig. 4.2 Preoperative computed tomography (CT) midsagittal image demonstrating the canal compromise by osseous encroachment. • Positive inverted radial reflex bilaterally • Hyperreflexia throughout upper and lower limbs • Grade ⅘ strength in deltoid/biceps (C5) bilaterally • Increased tone in lower limbs • Plantars upgoing • Nurick grade 2 Radiological evaluation of patients with CSM begins with plain radiographs, including anteroposterior (AP), lateral, and flexion-extension views.2,3,25,47–49 These studies yield useful information regarding cervical spine alignment and the presence of preserved or lost cervical lordosis. Additionally, careful attention should be paid to the presence of facet joint arthrosis, the disk space height, and the presence of disk marginal osteophytes. Segmental alignment anomalies are usually accentuated on the flexion views if there is dynamic instability. Although an accurate measurement of stenosis is difficult to assess on plain X-rays, they will give an early indication of congenital or acquired stenosis changes. Fig. 4.3a–c Preoperative sagittal (a,b) and transverse (c) magnetic resonance imaging (MRI) scans. Canal compromise and the offending structures responsible for the compression are shown, in addition to spinal cord compression and spinal cord parenchymal changes. Fig. 4.4a–c Postoperative plain X-rays (a,b) and sagittal T2 MRI (c) demonstrating C2–T1 decompression and instrumented fusion. Note the placement of the screws in the pars of C2 and pedicles of T1. Magnetic resonance imaging is the goldstandard imaging modality for evaluating soft tissues, including the neural elements, intervertebral disks, ligamentum flavum, and spinal cord, including the cerebrospinal fluid (CSF) space. Signal abnormalities within the spinal cord such as focal areas of increased T2 signal change and reduced T1 signal change are emerging as variables that can help determine prognosis.6,10,13,27,47,50,51 Having said this, however, strong evidence guiding how signal changes ought to be interpreted does not presently exist. Multiplanar computed tomography (CT) scan of the cervical spine is also necessary to fully evaluate the extent of the osseous pathology. Osteophytes adjacent to the disk margins as well as foraminal osteophytes from the uncovertebral joints and facet joints can be delineated accurately with CT. Additionally, OPLL is readily demonstrated with CT.18,52 In the absence of CT scanning, plain radiographs may provide a useful alternative. It is necessary to highlight the importance of correlating the findings on an MRI scan with the clinical picture, as the MRI may be overly sensitive, especially if reliance is placed on short-time inversion recovery (STIR) sequences. Furthermore, it is necessary to evaluate the radiographs or CT along with MRI to determine the possibility of congenital fusion of cervical vertebrae. Although fusion of the vertebrae may occur circumferentially at the periphery of vertebral bodies, there may be disk elements in the center; thus, thick sagittal slices on MRI may not provide a clear indication of vertebral fusions. This is important, as patients with fusion of the vertebrae have been recognized as particularly susceptible to spine degeneration.53 In cases where imaging has not resolved equivocal clinical findings, electrodiagnostic studies may provide useful information. Additionally, electrodiagnostic studies may be employed to exclude suspected peripheral nerve entrapment syndromes.30,54 The imaging results guide the decisionmaking process as to whether cervical laminectomy and fusion are the most appropriate surgical strategy; in general, however, surgery has historically been reserved for patients with rapidly progressive, long-standing, and severe functional loss. In the presence of significant or progressive myelopathy with or without radiculopathy or neurogenic claudication, surgical intervention should be considered and the risks and benefits discussed with the patient. The clinical manifestations of the cervical pathology are the main influencing factor in the decision-making process. Although patients with mild cord compression may be closely followed with conservative treatment, as was discussed in the natural history of CSM earlier in the chapter, many will progress to more debilitating disease over time. The undertaking of decompression surgery for symptomatic myelopathy aims to accomplish the following1,3,5,7,9: • Decompress the spinal cord • Promote an environment for spinal cord recovery • Preserve spinal column alignment and prevent deterioration in cervical spine alignment in the future • Minimize the risk of axial neck pain, risk of recurrence, and requirements for reoperation • Provide the most cost-effective treatment • Arrest the progression of myelopathy Although limited, an improvement in the quality of life through the recuperation of functional deficits may occur in some cases as well10; fundamentally however, the surgical indication remains based on arresting disease progression. To maximize the risk/benefit analysis it would be useful to have a tool to help determine the chances of the myelopathy progressing and to predict the likely benefit that can be expected from decompression and stabilization of the spine. Such a tool, in the form of a clinical prediction model, was developed by Tetreault et al44 using data from the AOSpine–North America study. The model was composed of six clinical and one imaging factor: age (odds ratio [OR], 0.97; 95% confidence interval [CI], 0.94–0.99; p = 0.0017), duration of symptoms (OR, 0.78; 95% CI, 0.61–0.997; p = 0.048), smoking status (OR, 0.46; 95% CI, 0.21–0.98; p = 0.043), impairment of gait (OR, 2.66; 95% CI, 1.17–6.06; p = 0.020), psychological comorbidities (OR, 0.33; 95% CI, 0.15–0.69; p = 0.0035), baseline mJOA score (OR, 1.22; 95% CI, 1.05–1.41; p = 0.0084), and baseline transverse area of the cord on MRI (OR, 1.02; 95% CI, 0.99–1.05; p = 0.19). Using this model the discrimination between a “successful” (mJOA ≥ 16) and “failed” (mJOA <16) postsurgical outcome at 1-year can be predicted with a 79% probability. In light of the fact that conservative management of CSM patients has a limited role and should be considered only in patients with mild cord compression, it is universally agreed that patients with progressive clinical manifestations require surgical treatment. Fifty years ago, it was realized that the main mechanism leading to neurologic deficit in patients with CSM was direct spinal cord compression17 and that a critical reduction in the diameter of the spinal canal was associated with the development of myelopathy.2 Despite this, however, not all stenosis necessarily leads to myelopathy. In a large series of asymptomatic patients, Hayashi et al21 found that 10% of patients had critically reduced canal diameter measuring less than 10 mm in the absence of neurologic deficits.21 The debate continues as to whether motion of the spinal column at the site of a spinal cord injury produces deleterious forces that either continue to produce spinal cord cell injury or limit the potential for cellular and spinal cord recovery. Laminectomy alone achieves decompression of the stenotic area of the canal and thus alleviates the pathological compression on the spinal cord, provided that adequate posterior drift of the cord is attainable from areas of anterior compression.19 However, it is well recognized that the results of laminectomy alone are inferior to decompressive procedures that are combined with a stabilization and fusion.24 This is likely due to the ongoing tensile load placed on already injured neurons, which limits the ability of the damaged neurons to recover or causes further neuronal damage. Additionally, fusion may also prevent further migration of disk elements into the canal that would otherwise potentially contribute to compression of the anterior cord. We can also extrapolate the following conclusions from the experience with traumatic spinal cord–injured patients: Elimination of the motion around an injured segment of the spinal cord is the mainstay of surgical management— the biological rationale is based on the assumption that motion around the injured spinal cord may limit the ability of the spinal cord to recover, and that ongoing motion, in the presence of established injury, leads to further neuronal damage and neuronal death. It is worth noting that the increased range of motion has also been implicated as a risk factor involved in the progression of OPLL after laminoplasty.26 Support for surgical intervention, however, is limited by the relatively few published studies on clinical as well as radiographic outcomes of cervical laminectomy and fusion in the treatment of CSM.27,31–33 Detailed preoperative imaging is evaluated prior to beginning the surgery. A thorough appreciation of the local anatomy and the location of key neural and vascular elements must be understood during this planning phase. In particular, the surgeon must have a clear understanding of the course and caliber of the vertebral artery, especially if fixation into C2 or bicortical lateral mass screws are intended to be used. The CT scan is useful for determining the bony anatomy, and the use of CT angiography is recommended. The alignment of the spine is critical when it comes to instrumentation and should be set at the beginning of the case by the surgeon and rechecked prior to definitive fixation. Intraoperative fluoroscopy or plain radiographs can be helpful for this process. Generally speaking, a parallel alignment between the vertebral column and the ramus of the mandible indicates a well-positioned patient. Additional maneuvers such as holding the shoulder girdle depressed with the use of tape and placing the arms by the sides in a wellpadded fashion will aid with imaging. Posterior cervical procedures are generally utilized for multilevel decompression and rely on direct and indirect decompression. Direct decompression occurs with removal of the posterior compressive elements, and indirect decompression occurs through the ability of the spinal cord to translate posteriorly and away from pathological elements that are compressing the cord at the anterior. Cervical laminectomy involves removal of the posterior spinal vertebral elements that contribute to the compressive process and thereby allow the dura and the spinal cord to expand and migrate posteriorly. Stabilization and eventual fusion is obtained most commonly with the use of a variable-angle lateral mass or a pedicle screws and rod construct. It should also be noted that intraoperative hypotension should be avoided. The incision can be planned using intraoperative imaging or by palpating the prominent bony landmarks of C2 and C7. The avascular interval between the cervical paraspinal musculature is utilized, and the dissection is carried laterally to the medial margins of the facet joints in a subperiosteal fashion. Care is taken to avoid violating the facet capsule of joints that are not intended to be incorporated in the fusion. Otherwise, the joint capsules should be excised and the joints prepared for the fusion process. A combination of curette, narrow nibblers, and small bur can be used to adequately prepare the joint surfaces for fusion (Fig. 4.5). The muscle attachments to C2 are carefully preserved to avoid C2/3 instability if C3 is the upper extent of the fusion. Predrilling the lateral mass screw holes is advisable, as it helps prevent removing excess lateral mass bone in the process of performing the laminectomy. Bleeding from the bone can be controlled with a hemostatic agent or bone wax. The orientation of the screws is determined by the orientation of the facet joints. This can be gauged by placing a narrow elevator in the facet joint space. The screw starting position is determined by the outline of the lateral mass. This can be obscured by spondylotic changes. The starting point is generally in the midline in the cephalad-caudal plane and 1 mm medial to the midline in the medial lateral plane. The trajectory of the screw is through the middle of the lateral mass in a 15-degree cephalad and 30-degree lateral direction. The cephalad direction should avoid injury to the nerve root, and the lateral trajectory should avoid injury to the vertebral artery. Bicortical fixation may be desired, and care should be undertaken to avoid overpenetration of the far cortex. The screw canal can be palpated with a small ball-tipped probe and the length measured and recorded. Tapping of the cortex to accept a 3.5-mm variable angle screw is undertaken prior to sealing the hole with hemostatic agent or bone wax. The use of intraoperative fluoroscopy or navigation is employed by some surgeons to minimize the risk of screw misplacement.
Laminectomy and Fusion for Cervical Spondylotic Myelopathy
 Introduction
Introduction
 Pathobiology
Pathobiology
 Classification and Outcome Measures
Classification and Outcome Measures
 Natural History of Cervical Spondylotic Myelopathy
Natural History of Cervical Spondylotic Myelopathy
 Patient History
Patient History
Examination Findings
 Illustrative Case
Illustrative Case
History
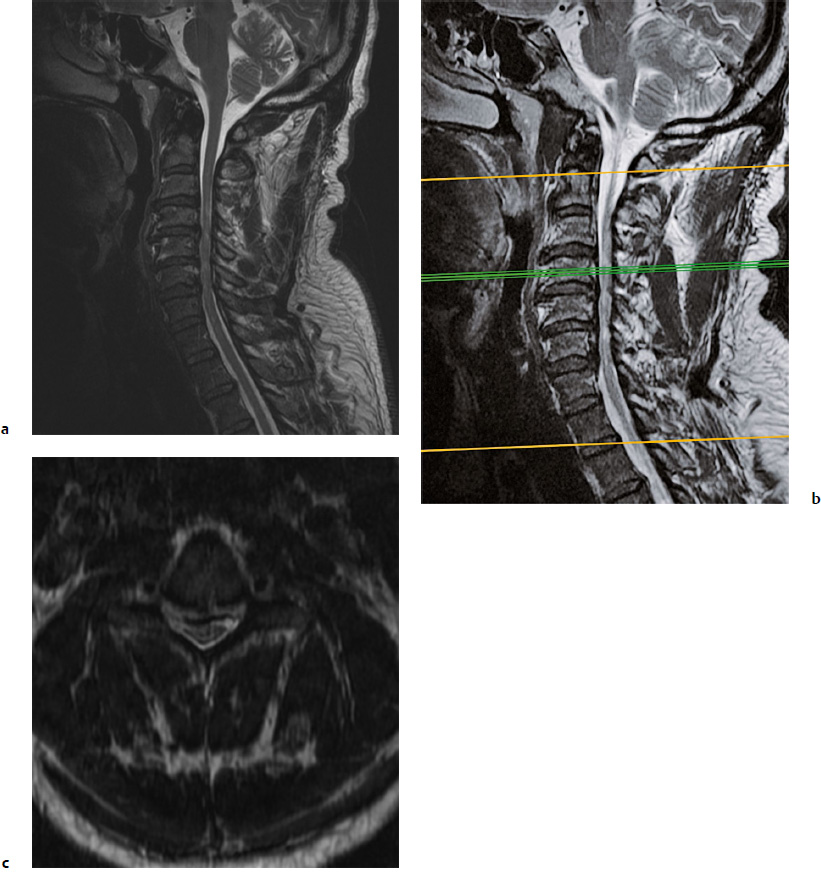
Physical Examination (Figs. 4.1, 4.2, 4.3, 4.4)
 Imaging
Imaging
 Cervical Laminectomy and Fusion
Cervical Laminectomy and Fusion
Indications, Technique, Benefits, Outcomes, and Complications
Objective
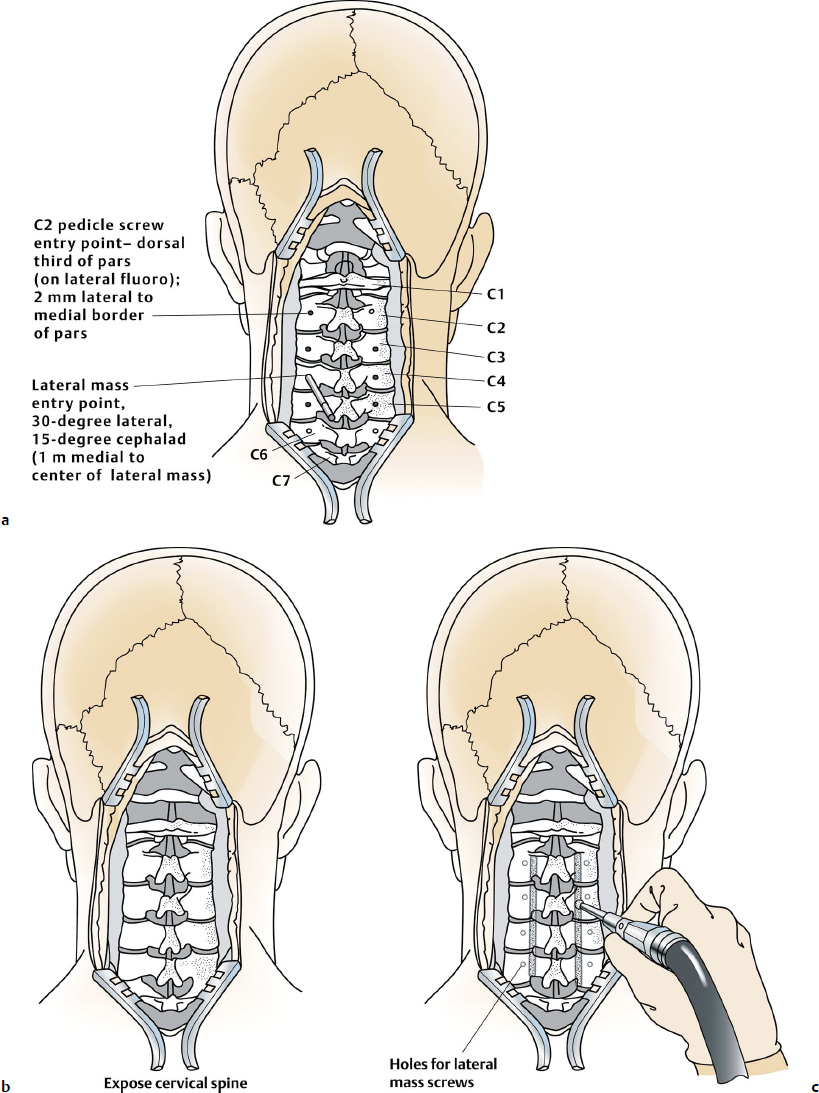
Technique: Cervical Laminectomy and Fusion
Overview
Preoperative Preparation
Surgical Procedure
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree