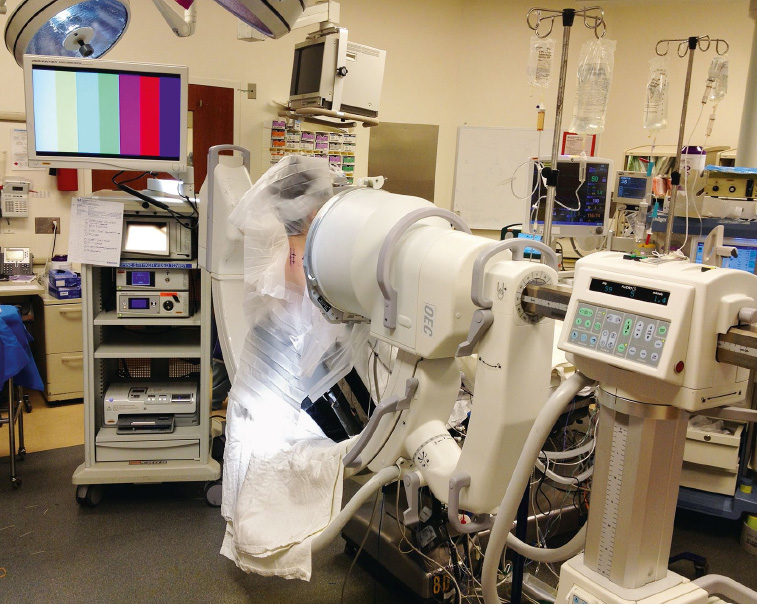
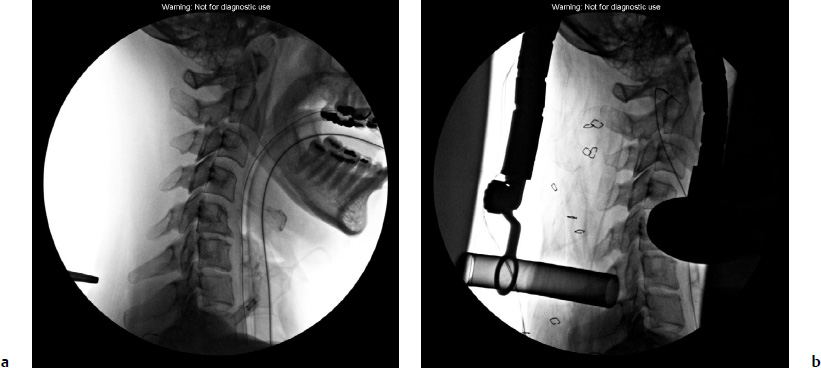
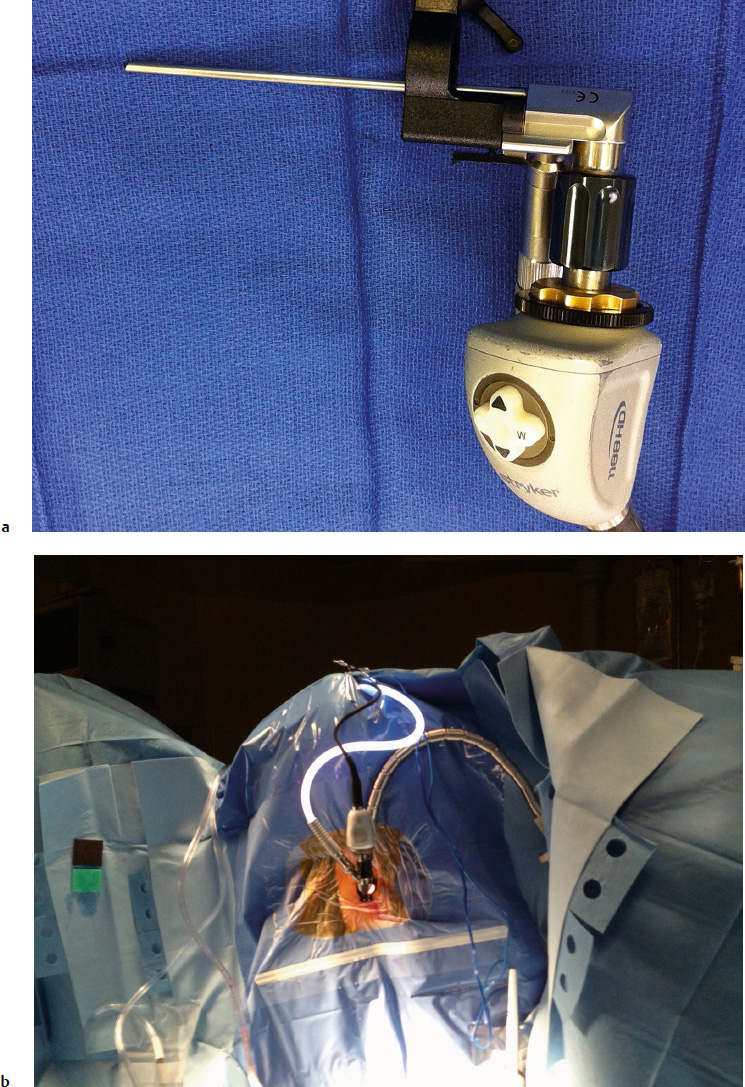
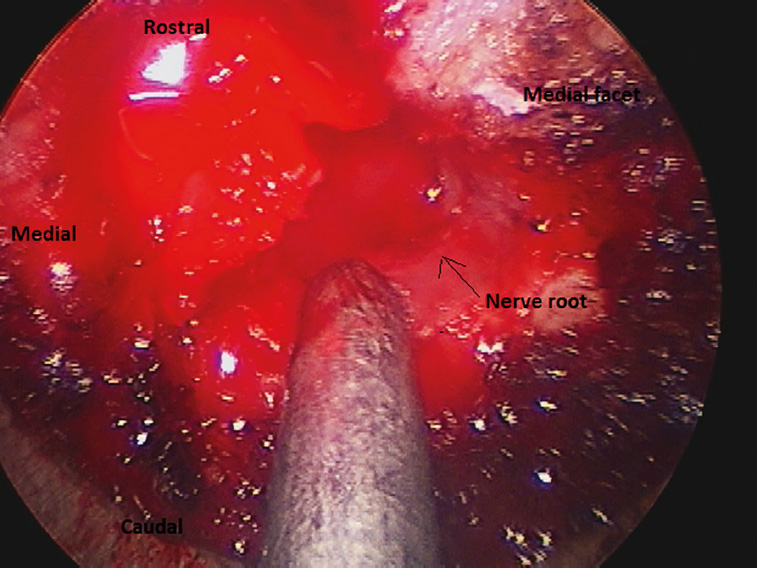
5 Cervical spondylosis is a degenerative spinal condition that can result in progressive foraminal or central stenosis of the spine leading to radiculopathy or cervical spondylotic myelopathy. Degenerative disk disease, cervical disk herniation, and foraminal stenosis may be treated with anterior cervical diskectomy with fusion or cervical arthroplasty. The anterior cervical approach provides direct decompression of ventral pathology with excellent improvement in preoperative clinical symptoms. However, this approach carries an associated risk of injury to anterior neck structures such as the recurrent laryngeal and hypoglossal nerves, the sympathetic plexus, esophagus, trachea, and thoracic duct. Additionally, a frequent complaint of patients from an anterior cervical approach is postoperative dysphagia. This may result from prolonged esophageal edema or the elevated profile from the cervical plate and instrumentation. Conversely, posterior cervical approaches minimize the risk of injury to vital anterior neck structures, may indirectly decompress the spinal cord from ventral spinal pathologies, and directly decompress posterior cervical disease (hypertrophic ligaments, facet joints, or soft disk herniations).1–3 However, a posterior cervical approach may result in increased postoperative pain from dissection of the posterior neck musculature, disruption of the posterior tension band and potential increased spinal instability, and increased risk of wound infections. This chapter describes the surgical technique for a minimally invasive posterior cervical microendoscopic foraminotomy (cMEF), reviews the current literature on the potential complications and outcomes of a posterior cMEF, and provides recommendations on the management of symptomatic posterior cervical spondylosis. Degenerative disease of the cervical spine may present as a radiculopathy, myelopathy, or myeloradiculopathy. Myelopathic symptoms occur due to compression of the spinal cord and may be treated with a minimally invasive decompression or with an open laminectomy with or without fusion. This chapter focuses specifically on cervical radicular symptoms that are amenable to a cMEF approach. This approach is often used for the treatment of mild to moderate cervical monoradiculopathy caused by “soft” disk disease or hypertrophic facets.4 Patients presenting with mild symptoms of radiculopathy and without clinically significant weakness may be initially treated with medical management.5,6 Surgical intervention is warranted if symptoms are intractable to medical management or progressive weakness is present.7 Several retrospective studies have shown significant improvement in clinical symptoms after posterior cervical foraminotomy in patients with cervical radiculopathy.8–19 The traditional open posterior cervical laminotomy and facetectomy has successfully treated cervical radiculopathy. However, the surgical approach requires significant soft tissue dissection of the paraspinal muscles, which may lead to chronic neck pain.3,20,21 Burke and Caputy12 were the first to successfully describe decompression of the cervical nerve roots comparable to an open approach on a cadaveric cervical spine with tubular retractors. A minimally invasive approach that employs a small incision, splitting of the muscle fibers with tubular retractors, and minimal soft tissue or bony resection to achieve a cervical foraminotomy may help limit the postoperative pain and recovery period. Prior to surgical intervention, a thorough history and physical examination as well as review of pertinent imaging (X-rays/magnetic resonance imaging [MRI] of the cervical spine) are always completed. Any ambiguity in the surgical level may be clarified with adjunctive tests; nerve conduction studies (NCS), electromyography (EMG), and nerve blocks may be helpful in confirming the level of the pathological nerve root. The patient is intubated under general anesthesia, pinned in three-point fixation with the Mayfield head holder, and placed in the “sitting position” (Fig. 5.1), which decreases pooling of blood in the operative field and improves visualization for the surgeon. A pillow is placed underneath the patient’s buttocks to prevent slipping down the surgical table. Neuromonitoring with electromyography, somatosensory evoked potentials, and motor evoked potentials is performed to detect early signs of injury to the neurologic elements during the procedure. Antibiotics are given prior to incision, and corticosteroids are administered at the discretion of the surgeon. Fluoroscopy is positioned for lateral X-rays, and the surgical field is prepped and draped in the usual sterile fashion. The operative levels are confirmed with fluoroscopy, and local anesthesia is infiltrated into the incision to minimize intraoperative bleeding and postoperative pain (Fig. 5.2a). An ipsilateral incision (2-cm length) is completed with a scalpel, measured 1.5 cm from the midline. Hemostasis is achieved with bipolar electrocautery. An Army-Navy retractor or similar hand-held blunt retractor is used to expose the underlying fascia and muscular bundles. Metzenbaum scissors are used to bluntly split the muscular bundles down to the bony lateral mass. The initial tubular dilator is placed over the lateral mass and the surgical level is confirmed by lateral fluoroscopy. A medial trajectory with the dilator should be avoided to minimize potential injury to the spinal cord. Serial muscle-splitting tubular dilators are positioned onto the ipsilateral lateral mass of the surgical level until the final 18-mm tubular retractor is locked into position and confirmed with fluoroscopy (Fig. 5.2b). The endoscope (Fig. 5.3a) or microscope is brought into the surgical field to maximize visualization (Fig. 5.3b). Fig. 5.1 The patient is placed in the sitting position to facilitate drainage of the surgical field. The fluoroscopy is placed for lateral X-rays and the endoscope monitor is positioned for optimal viewing capabilities. Fig. 5.2a,b (a) The operative level is confirmed with lateral fluoroscopy at C6-C7. (b) The final tubular retractor is locked into place and confirmed with X-rays. Fig. 5.3a,b (a) A close-up view of the endoscope used for cervical microendoscopic foraminotomy (cMEF). (b) The endoscope is locked onto the final tubular retractor to optimize visualization of the surgical field. The soft tissue overlying the laminofacet junction is removed with a combination of monopolar electrocautery and pituitary rongeurs. An up-angled curette is used to define the sub-laminar plane, and Kerrison rongeurs complete the laminotomy. Alternatively, a high-speed drill may be used for the laminotomy. The medial facet joint is similarly removed with the drill and rongeurs until the cephalad and caudad pedicles are easily palpated with a nerve hook. This exposure provides adequate decompression without increasing the risk of spinal instability (Fig. 5.4).22,23 The underlying ligamentum flavum is dissected free from the thecal sac with an up-angled curette or nerve hook. Kerrison rongeurs are used to completely resect any ligament that may be contributing to central or foraminal stenosis. The lateral recess is decompressed and the symptomatic nerve root is mobilized to ensure there is no residual compression (Fig. 5.5). A ball-tipped nerve hook may be used to palpate ventral to the nerve root and dislodge any residual compressive pathology (residual disk fragment, ligament, or osteophyte). Hemostasis is achieved with bipolar electrocautery, bone wax, and Gelfoam (Baxter Healthcare, Glendale, CA), followed by antibiotic irrigation. As the tubular retractor is removed, bipolar electrocautery of residual soft tissue bleeding minimizes the risk of postoperative hematoma formation. The fascia and subcutaneous tissue are closed with absorbable sutures and the skin is approximated with a subcuticular suture and a skin adhesive (Dermabond, Ethicon, Somerville, NJ).
Posterior Cervical Minimally Invasive Microendoscopic Foraminotomy
 Introduction
Introduction
 Cervical Spondylosis: Natural History
Cervical Spondylosis: Natural History
 Surgical Technique
Surgical Technique
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree