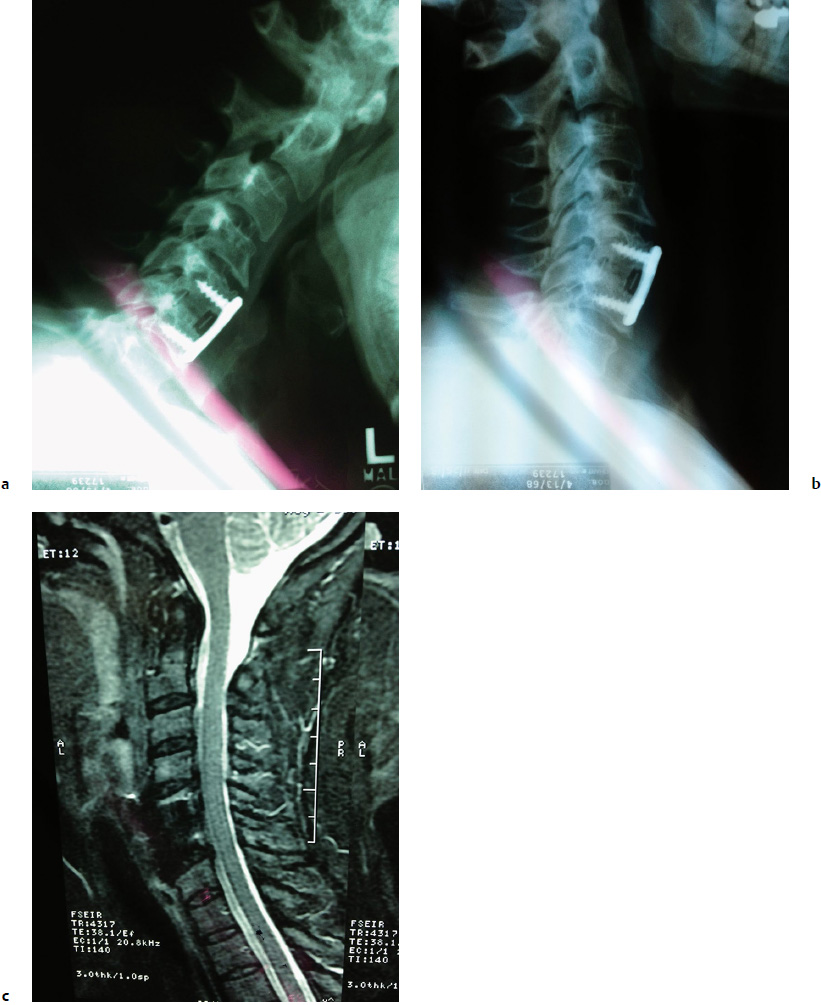
10 The number of cervical and lumbar fusions that have been performed has increased significantly in recent decades. Between 1998 and 2008, the annual number of spinal fusion discharges in the United States increased 2.4-fold (137%) from 174,223 to 413,171. In contrast, during the same time period, laminectomy, hip replacement, knee arthroplasty, and percutaneous coronary angioplasty yielded relative increases of only 11.3%, 49.1%, 126.8%, and 38.8%, whereas coronary artery bypass graft experienced a decrease of 40.1%.1 Anterior cervical diskectomy and fusion (ACDF) was first introduced in 1950s2,3 and has become the standard of care for a wide variety of cervical pathology. The clinical success rate of these procedures is generally high, and adverse events are infrequent and manageable. However, awareness of potential adverse events is critical to reduce their incidence and to adequately inform patients regarding the surgical risk. These potential complications can be categorized as those occurring intraoperatively (esophageal injury, vertebral artery injury, dural tear, spinal cord/nerve root injury), those occurring in the early postoperative period (airway compromise, epidural hematoma, radiculopathy), those occurring in the intermediate postoperative period (dysphagia, dysphonia, wound infection, and bone graft dislodgment), and long-term sequelae such as adjacent-segment degeneration (ASD) and nonunion.4 Adjacent-segment disease was first described by Lee5 in 1988 in the lumbar spine following fusion surgery. In his report, Lee presented 18 patients who developed new symptoms from a segment adjacent to lumbar fusion after being completely asymptomatic for an average of 8.5 years. Since then, several studies have described a similar phenomenon in cervical spine. Unfortunately, there is a lack of precision in the terminology used to describe the entities associated with segments adjacent to fusion. Hilibrand and Robbins6 distinguished two kinds of adjacent-level pathology after fusion. The term adjacent-segment degeneration (ASD) describes radiographic changes observed at levels next to the previously fused segment or segments (Fig. 10.1); this degeneration may not correlate with clinical symptoms. In contrast, adjacent-segment refers to the development of new radiculopathy or myelopathy referable to a motion segment adjacent to the site of a previous anterior arthrodesis in the cervical spine More recently the term adjacent-segment pathology (ASP) has been proposed as an umbrella term to refer to the breadth of clinical or radiographic changes at adjacent motion segments that developed subsequent to a previous spinal intervention. Under this umbrella, radiological ASP and clinical ASP (CASP) are then used to categorize radiographic features (e.g., degenerative changes on magnetic resonance imaging [MRI]) and clinical manifestations (e.g., new radiculopathy), respectively.7 Fig. 10.1a–c X-ray in flexion (a) and extension (b), and magnetic resonance imaging (MRI) (c) of a patient 3 years after a prior anterior cervical diskectomy and fusion (ACDF) at C5–C6. Radiographic changes are observed at the adjacent segment (C4–C5) in all images. Although the existence of ASP has become universally accepted, the etiology of ASP has not been established. Some studies have suggested that fusion causes increased stress and strain on neighboring segments, which can potentially cause rapid degeneration in these segments. In 1999, Hilibrand et al8 studied the incidence, prevalence, and radiographic progression of symptomatic adjacent-segment disease, which was defined as the development of new radiculopathy or myelopathy referable to a motion segment adjacent to the site of a previous anterior arthrodesis of the cervical spine. They found that symptomatic adjacent-segment disease occurred at an incidence of 2.9% per year (range, 0.0 to 4.8% per year) during the 10 years after the operation. Interestingly, they found, contrary to the initial hypothesis, that the risk of new disease at an adjacent level was significantly lower following a multilevel arthrodesis than it was following a single-level arthrodesis (p < 0.001). They suggest that patients should be informed of the substantial possibility that new disease will develop at an adjacent level over the long term following fusion surgery. In 2002, Eck et al9 published a biomechanical study performed to determine the effect of cervical spine fusion on adjacent-level intradiscal pressure. In six cadaveric specimens, intradiscal pressures and segmental motion at C4–C5 and C6–C7 were recorded first on intact specimens, and then after anterior cervical plating at C5–C6. They found that significant increases in intradiscal pressure and segmental motion occur at levels adjacent to fusion during the normal range of motion (ROM). In another study, Lopez-Espina et al10 demonstrated stress increases of up to 96% in the annulus, nucleus, and end plates after fusion in the levels below and above the fused segments. In 2013, Anderst et al11 published a study to evaluate cervical intervertebral ROM during dynamic flexion-extension in patients who had undergone a single-level arthrodesis and compare that to asymptomatic control subjects. Data from 10 patients treated with C5–C6 arthrodesis and 20 controls were included in the analysis. The authors found that the adjacent segment (C4–C5) moved through a larger extension ROM and a smaller flexion ROM in the subjects with the fusion. Further, posterior translation was greater compared with the controls. Despite this, it is important to keep in mind that even without surgery, the spine undergoes degenerative changes with age. Boden et al12 performed MRI of the cervical spine in 63 asymptomatic volunteers. Radiographic abnormalities were noted in 14% of those younger than 40 years; this is in contrast with abnormalities in 28% of those 40 years of age or older. Matsumoto et al13 used MRI to analyze degenerative changes in the cervical intervertebral disks of 497 asymptomatic subjects. Not surprisingly, degenerative findings were present in only 17% of men and 12% of women aged 20 to 29 years compared with 86% of men and 89% of women 60 years of age or or older. Gore14 followed 159 asymptomatic volunteers and reported that 15% of study subjects had pain at the 10-year follow-up. These studies pose a serious challenge when establishing a causation of the adjacent segment with surgical fusion versus that occurring simply as a natural aging process. However, more recently in another paper Matsumoto et al15 performed follow-up MRIs on 64 patients who underwent ACDF (48 males, 16 females; mean age 47.3 years; mean follow-up 12.1 year) and 201 asymptomatic volunteers (113 males, 88 females; mean age 41.1 years; mean follow-up 11.7 years). All these subjects had undergone a previous MRI as well. The patients and control subjects underwent follow-up MRI in this study. They evaluated these MRIs on (1) a decrease in signal intensity of disk (DSI), (2) posterior disk protrusion (PDP), (3) disk space narrowing, and (4) foraminal stenosis. Their results showed that progression of DSI was significantly more frequent in the ACDF group at C4–C5. Progression of PDP was significantly more frequent in the ACDF group than in the control group at all levels except for C5–C6, and progression of disk space narrowing and foraminal stenosis was significantly more frequent in the ACDF group at C3–C4 and at C6–C7, respectively. These MRI findings also had some correlation with clinical symptoms. Those patients with progression of disk space narrowing at the adjacent segment after ACDF had significantly more frequent headache and neck pain; stiff shoulder was significantly more frequently observed in patients with progression of foraminal stenosis than in those without (p < 0.05). This study demonstrated that although progression of disk degeneration at the interval of 10 years was observed both in the ACDF and the control groups, the incidence of progression was significantly higher in the ACDF group than in the control group especially in posterior disk protrusion. One huge limitation of this study is that it is practically impossible to have perfectly matched cohorts. Patients who undergo ACDF for disk degeneration are obviously more susceptible to degeneration, whether it is secondary to genetic factors, environmental factors, or other factors, and are inherently at increased risk of degeneration at other levels. In yet another study published in 2011, Song et al16 radiographically assessed disk degenerative changes, anterior ossification formation, and segmental instability in 87 patients who had undergone single-level anterior cervical decompression and fusions with at least 5 years of follow-up. In segments adjacent to the fusion (above or below), degenerative changes developed in 28 segments (16%), and two of those patients (2%) developed new clinical symptoms. In nonadjacent segments, degenerative changes developed in 10 segments (3%), and two of those patients (0.7%) also developed new clinical symptoms. Additional operations were performed in one patient in each group. This study showed that “although, fusion per se can accelerate the severity of adjacent-level degeneration, no significant difference was observed between adjacent and nonadjacent segments in terms of the incidence of symptomatic disease.” The authors concluded that adjacent-segment disease is more a result of the natural history of cervical spondylosis than of the presence of fusion. Other authors have suggested that soft tissue injury during surgery may be a contributing factor to the development of ASP. For example, many surgeons insert a needle into the disk to confirm the appropriate level during ACDF; meanwhile, attempts to study the natural history of disk degeneration involves the very same procedure of inserting a needle at the center of the disk through the annulus fibrosus and into the nucleus pulposus,17–19 and therefore the question has been raised whether or not a needle puncture could potentially lead to degenerative changes in an incorrectly marked disk level. Nassr et al20 published a retrospective study to determine the relative risk of adjacent-level disk degeneration after incorrect needle localization in patients undergoing ACDF; 87 patients were included in the study (36 underwent one-level ACDF and 51 underwent two-level ACDF). Seventy-two had correct needle localization at the level of planned surgery; 15 had incorrect needle localization (one level above the operative level). There were no differences between the two groups in age, sex, and length of follow-up. Patients in the incorrectly marked group were statistically more likely to demonstrate progressive disk degeneration with an odds ratio of 3:2. The authors concluded that either needle-related trauma or unnecessary surgical dissection may contribute to accelerated ASD. Additionally, adjacent-level ossification has been associated with plate placement within 5 mm of the adjacent level.21 Although no association has been established thus far among adjacent-level ossification, degeneration, and ultimate disease, both of these studies emphasize the importance of soft tissue anatomy at the adjacent level. Because the real cause of ASP is yet to be determined, several investigators have attempted to pinpoint some of the possible contributing risk factors. Lawrence et al22 published a systematic review of five studies (four retrospective cohorts and one database study) in an attempt to determine the risk and to define potential identifiable risk factors for the development of ASP after cervical fusion surgery. In their review the prevalence of CASP ranged from 11 to 12% at 5 years, 16 to 38% at 10 years, and 33% at 17 years. Some of the factors that may contribute to the pathology included age younger than 60 years, fusion adjacent to the C5–C6 or C6–C7 levels, a preexisting disk herniation, and/or dural compression secondary to spinal stenosis with a mean anteroposterior diameter spinal canal of 13 mm or smaller. Postsurgical sagittal imbalance has also been suggested as a risk factor.23 Another potential factor is the initial indication for spinal fusion. In a systematic review by Lee et al,24 radiographic ASP (RASP) following surgical fusion for degenerative disease, for trauma, or for conditions requiring fusion in pediatric population were assessed. Their results showed that in the cervical spine, the rate of RASP in patients with fusion for degenerative reasons is greater, suggesting that the preexisting health and status of the adjacent level at the time of fusion may play a contributory role in the development of ASP. Because the concept that interbody fusion of the cervical spine leads to accelerated degeneration of adjacent disk levels due to increased stress from the fusion is widely postulated, in recent years cervical disk replacement (CDR) has been proposed as a viable alternative method of managing cervical spondylosis. The advocates of CDR argue that it should offer the same benefits as fusion while providing motion, thereby protecting the adjacent level disks from the abnormal stresses associated with fusion. Several in vitro studies have shown theoretical advantage of CDR over ACDF by demonstrating difference in motion at the adjacent level between the two. Chang et al25 performed a study to compare adjacent-level intradiscal pressure (IDP) and facet force following arthroplasty with the fusion model. Their results showed that unlike in specimens treated with fusion, those treated with arthroplasty maintain adjacent-level IDPs near the preoperative values in all modes of motion. Several other in vitro studies have demonstrated similar findings as well.26,27 Despite the theoretical advantage of CDR over ACDF demonstrated in these studies, the clinical data are more variable. In 2002, Goffin et al28 published their short-term results in a prospective, concurrently enrolled, multicenter trial of patients with single-level degenerative disk disease undergoing Bryan Cervical Disk Prosthesis surgery. Analysis included data regarding 60 patients at 6 months, and with 30 of those patients at 1 year. Clinical success at 6 months and 1 year after implantation was 86% and 90%, respectively. Although this study has some early promising results, the follow-up period was too short to draw any conclusions on ASP. In 2011 Maldonado et al29 published a prospective cohort study to evaluate the incidence of ASD in patients who underwent CDR as compared with ACDF. Radiographic evidence of ASD was found in 11 (10.5%) patients in the ACDF group and in seven (8.8%) subjects in the CDR group; this finding was not statistically significant, and the authors concluded that preservation of motion was not associated with a reduction of the incidence of symptomatic adjacent-segment disease. In another prospective, randomized United States Food and Drug Administration (FDA) investigational device exemption (IDE) pivotal trial conducted at 21 centers across the United States, 269 patients were enrolled and randomly assigned to either cervical total disk replacement (136 patients) or to ACDF (133 patients). There were no significant differences between the disk replacement and ACDF groups when comparing operative time, blood loss, length of hospital stay, and the reoperation rate at the index level. The ROM in the CDR group decreased at 3 months but was significantly greater than the preoperative mean at 12- and 24-month follow-up. The ROM in the ACDF group was significantly reduced by 3 months and remained so throughout the follow-up. As for adjacent-level degeneration, there were no significant differences between groups when evaluating the different levels of adjacent-level degeneration preoperatively. However, at the 2-year follow-up, there were significantly more patients in the ACDF group with severe adjacent- level radiographic changes (p < 0.0001). However, there were no significant differences between groups in adjacent-level reoperation rate.30 Kelly et al26 performed post-hoc analysis of data acquired in a prospective randomized controlled trial involving 209 patients at 13 sites who were treated in a prospective randomized controlled trial of ACDF versus total disk arthroplasty for single-level symptomatic cervical DDD. Changes in ROM were assessed using flexion/extension radiographs; 199 patients had at least a 2-year follow-up. The authors found no significant difference in adjacent-segment ROM between ACDF and arthroplasty. Their analysis showed time to be a significant predictor of changes in adjacent-segment ROM, and no association between the treatment chosen and ROM could be observed. Similarly, Jawahar et al31 in a randomized, prospective IDE trial between arthroplasty and anterior cervical diskectomy and fusion that included 64 patients (25 fusion and 39 arthroplasty) with median follow-up of 37 months, demonstrated that ASD developed in 16% of arthroplasty patients and 18% of fusion patients; this difference was not statistically significant (p = 0.3). In an excellent systematic review, Harrod et al32 attempted to answer if there is evidence that total disk replacement is associated with a lower risk of radiographic or clinical ASP compared with fusion. Unfortunately, they found a paucity of high-quality literature comparing motion-preserving devices to fusion. They found that the risk of reoperation for clinical ASP ranges from 1.0 to 4.8%, and there is no statistically significant difference between the two groups in this regard. More recently, in 2013 Blumenthal et al33 published their data collected from multiple prospective, randomized studies conducted at the same site to compare the reoperation rates in cervical total disk replacement and anterior cervical fusion patients; 136 patients were included (84 total disk replacement, 52 ACDF) with a mean follow-up of 55.1 months. The re-operation rates as well as the length of time after the index surgery before the reoperation occurred were compared between the two groups. The authors found that the reoperation rate was significantly lower in the arthroplasty group (8.3% vs 21.2%; p < 0.05). Further, a trend was observed that ASD was less likely the cause of reoperation in the arthroplasty group compared with the fusion group (4.8% vs 13.5%; 0.05 < p < 0.07). Reoperations occurred significantly later in the arthroplasty group. As with most other spine conditions, the treatment options are surgery versus conservative management. Unfortunately, no comparative studies have evaluated the effectiveness and safety of operative versus nonoperative treatments for cervical ASP. Elsawaf et al,34 in a small series and using conservative treatment methods, successfully treated four of five patients who developed ASD after ACDF with an average follow-up of 28 months. Unfortunately, this case series does not provide details about the treatment protocol. Other similarly small series exist in the literature utilizing a wide variety of protocols such as physical therapy, immobilization, traction, anti-inflammatory medications, and injections; however, as previously stated, no prospective randomized studies compare patients with ASD who were treated conservatively with those undergoing surgery. Further, very few studies support any one conservative treatment strategy. As for surgical treatment, the options include laminoplasty, fusion, and arthroplasty. On review of the literature, two small case series exist on patients with ASD treated with laminoplasty. Baba et al35 described 18 patients treated with laminoplasty for ASD after ACDF and followed up for an average of 2.8 years. Another study by Matsumoto et al36 included 31 patients who underwent laminoplasty for cervical myelopathy resulting from adjacent-segment disease and age- and sex-matched 31 patients with myelopathy who underwent laminoplasty as the initial surgery. Both of these studies used the Japanese Orthopaedic Association assessment scoring system to evaluate the patients. Baba et al demonstrated 10 good/excellent results (56%), with a greater proportion of good/excellent results in men and in patients with a longer symptom-free period before presentation with ASD. Matsumoto et al had 11 patients with good/excellent results (38%) but found the population of patients undergoing primary surgery for myelopathy demonstrated greater gains. The evidence for effectiveness of fusion for treatment of ASD is poor as well. In 1997, Hilibrand et al37 published a retrospective review of all patients surgically treated for adjacent-segment disease of the cervical spine over a 20-year period; 38 patients who were treated by diskectomy with interbody grafting or corpectomy with strut grafting were included in this study. Arthrodesis was evaluated by flexion-extension lateral radiographs, and clinical outcomes were assessed at least 2 years after surgery. At a follow-up of 68 months, the investigators found that 84% of the patients had self-described excellent or good outcomes. Gause et al38 published a retrospective study that included 56 consecutive patients who underwent anterior treatment for junctional cervical stenosis. Forty-nine of these patients were treated with an anterior diskectomy and instrumented arthrodesis using iliac crest autograft, and seven underwent a corpectomy. Unfortunately, this study did not include a patient-related outcome measure; however, it did demonstrate a solid fusion in 81.6% of patients in the study group. The rate of fusion was significantly higher in those undergoing a single-level arthrodesis adjacent to a one-level fusion at 95.2% compared with those with longer preexisting fusion segments at 81.3% (two-level) and 57.1% (three-level). More recently, in 2013 O’Neill et al39 published a retrospective review of 40 patients undergoing ACDF for ASD to determine its clinical outcomes and cost utility. They found that this procedure results in significant improvement in outcome measures. Patient-reported health status also significantly improved. The mean 2-year cost-per-quality adjusted life years was determined to be $60,526, which suggests surgical intervention to be cost-effective. The final surgical treatment option for symptomatic ASP in the cervical spine is artificial disk replacement. Again, there is a paucity of literature on the topic. Sekhon et al40 reported a series of 15 patients treated with arthroplasty after having previous surgery of the cervical spine. Six of these patients had undergone posterior foraminotomy and nine had anterior fusion. The indication for surgery for those with previous fusion was neural compression at levels adjacent to a previous fusion site. The follow-up duration ranged from 12 to 43 months (mean 24.2 months). Unfortunately, the results are not broken down based on the original procedure in this report, but overall these patients did well, and good results were obtained in all cases as reflected by an increase in the visual analogue scale (VAS) score of 6.4 in terms of neck/arm pain. Phillips et al41 have provided the only prospective study on this topic to date. Unfortunately, this study does not provide a direct comparison of patients with ASP treated with arthroplasty versus those treated with other surgical options. Rather, in this study, those patients with ASP after previous ACDF treated with arthroplasty are compared with those patients undergoing arthroplasty without a previous operation and ASP. The cohorts included 126 patients with arthroplasty as a primary procedure with a mean age of 44.4 years and 26 patients with previous adjacent-level fusion with a mean age of 46.4 years. Patient-reported outcome measures such as the Neck Disability Index (NDI) and neck and arm VAS scores, and all complications and adverse events were recorded at 6-week, 3-month, 6-month, 1-year, and 2-year follow-up. Clinical outcome scores were significantly improved after surgery in both groups with no significant difference. Revision surgery occurred in two of 126 primary patients, and in two of 26 patients in the adjacent-to-fusion group. The authors concluded that disk replacement adjacent to a previous fusion has comparable outcomes to primary disk replacement surgery. However, the number of subjects in the adjacent-level group was small, and it is possible that the study is too underpowered to detect the differences in the two groups; further, the follow-up period is very short, and therefore definitive conclusions cannot be made based on this study. Adjacent-segment degeneration in the cervical spine remains a controversial topic, and there is a paucity of high-quality literature addressing this issue. At the current time, there is no strong, undisputed evidence on the etiology, risk factors, incidence, treatment, or even the terminology. Most recently, adjacent-segment pathology (ASP) has been proposed as the general term to describe changes that occur adjacent to a previously operated on segment. These changes may be radiographic (RASP) or associated with clinical symptoms (CASP). The current accepted rate of the development of CASP after arthrodesis is estimated between 1.6% and 4.2% per year with the reoperation rate of 0.8% per year. It remains unclear whether or not CASP is secondary to surgical intervention or is part of the natural history of the cervical spine. Some early evidence had suggested that fusion may cause extra stress on the adjacent segment and accelerate the rate of degeneration. Because of that, many believed that motion-preserving surgery could help prevent ASP. However, there is a lack of high-quality literature comparing motion-preserving devices or treatment methods to fusion, and at current time we do not have strong data that would support a significant difference in the development of RASP and CASP after cervical arthroplasty versus ACDF at short- to midterm follow-up. As for treatment, again limited data are available on options such as laminoplasty, fusion, and arthroplasty. All of the existing studies are of poor quality, with small sample sizes and limited follow-up and it is impossible to make any strong recommendations on the treatment of choice based on the current data. Further studies are needed that use a standardized definition of ASP and carefully document its development. We also need higher-powered studies that evaluate the treatment options in double-blinded prospective randomized fashion. Pearls Pitfalls
Adjacent Segment Pathology of the Cervical Spine
 Introduction
Introduction
 Definition
Definition
 Etiology
Etiology
 Risk Factors
Risk Factors
 Motion-Preserving Surgery
Motion-Preserving Surgery
 Treatment
Treatment
 Chapter Summary
Chapter Summary
 Adjacent-segment pathology may occur at a higher rate than natural spinal degeneration after surgical intervention.
Adjacent-segment pathology may occur at a higher rate than natural spinal degeneration after surgical intervention.
 The risk of developing new symptoms secondary to ASP after cervical fusion surgery ranges from 1.6 to 4.2% per year.
The risk of developing new symptoms secondary to ASP after cervical fusion surgery ranges from 1.6 to 4.2% per year.
 Not all patients with ASP require reoperation.
Not all patients with ASP require reoperation.
 Currently, there is no strong evidence that motion-preserving surgery can decrease the risk of cervical ASP compared with fusion surgery.
Currently, there is no strong evidence that motion-preserving surgery can decrease the risk of cervical ASP compared with fusion surgery.
 Arthroplasty and ACDF result in clinically similar kinematic changes at short-term follow-up.
Arthroplasty and ACDF result in clinically similar kinematic changes at short-term follow-up.
 There is no consensus on the treatment of ASP. Arthroplasty, laminoplasty, and fusion have been described and all seem to be effective.
There is no consensus on the treatment of ASP. Arthroplasty, laminoplasty, and fusion have been described and all seem to be effective.
 More high-quality studies are required on this topic.
More high-quality studies are required on this topic.
 There is some evidence that the following are risk factors for increased ASP: fusion adjacent to the C5–C6 or C6–C7 levels and a preexisting disk herniation. In addition, dural compression secondary to spinal stenosis with a mean anteroposterior diameter spinal canal of 13 mm or smaller appears to increase the risk of symptomatic adjacent segment pathology.
There is some evidence that the following are risk factors for increased ASP: fusion adjacent to the C5–C6 or C6–C7 levels and a preexisting disk herniation. In addition, dural compression secondary to spinal stenosis with a mean anteroposterior diameter spinal canal of 13 mm or smaller appears to increase the risk of symptomatic adjacent segment pathology.
 Postsurgical sagittal imbalance has also been suggested as a risk factor; therefore, postoperative kyphosis should be avoided, if possible.
Postsurgical sagittal imbalance has also been suggested as a risk factor; therefore, postoperative kyphosis should be avoided, if possible.
Adjacent Segment Pathology of the Cervical Spine
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree