Fig. 28.1
Moving valgus stress test
28.4 Essential Radiology
The workup of medial elbow pain in the overhead athlete begins with an anteroposterior and lateral radiograph of the elbow. Radiographs should be examined for osteophytes associated with posteromedial impingement, radiocapitellar arthritis, and intra-articular loose bodies. An oblique view has been described for optimal visualization of posteromedial olecranon spurs, but in our experience, a good lateral radiograph is sufficient. Stress radiographs have fallen out of favor and are not routinely obtained. Magnetic resonance imaging (MRI) of the elbow is usually performed with contrast to evaluate for an injury to the MUCL and intra-articular pathology. A T-sign has been described to diagnose tears of the MUCL as fluid extravasates between the MUCL and its origin on the humerus where it has peeled off [22] (Fig. 28.2). Whereas nonenhanced MRI has a high specificity (100 %) but a low sensitivity (57 %) [22], saline-enhanced MRI arthrography increases the sensitivity to 92 % [23]. Stress ultrasound is emerging as an alternative technique to MRI in the evaluation of MUCL injuries [24].


Fig. 28.2
T-sign
28.5 Disease-Specific Clinical and Arthroscopic Pathology
MUCL injuries are often partial-thickness tears associated with chronic overuse injuries and microtrauma. Full-thickness tears may be seen in patients who sustain contact-associated valgus loading of the elbow. Ulnar neuritis may develop in association with medial elbow instability as traction is applied to the ulnar nerve from valgus instability.
Several authors have described arthroscopic techniques to assist with diagnosis of an MUCL injury [25, 26]. Only the most anterior 25 % of the anterior bundle can be visualized arthroscopically [26]. Because the ligament cannot be visualized in its entirety arthroscopically, a cadaveric study looked at the degree to which the medial compartment gaps open with stress arthroscopically. Field and Altchek found that at 70° of elbow flexion, sectioning of the anterior bundle of the MUCL leads to 1–2 mm of opening, whereas sectioning of the entire MUCL leads to 4–10 mm of opening [26]. The advantage of arthroscopy is that it can be used to address intra-articular pathology that otherwise might not be accessible from an open medial exposure of the ulnohumeral joint. Chondral lesions typically present on the radiocapitellar joint surface due to lateral compressive loading. Microfracture and chondroplasty are arthroscopic techniques that can be used to address chondral lesions. Posteromedial olecranon spurs can be removed arthroscopically or from an open medial approach (Figs. 28.3, 28.4, 28.5, and 28.6).





Fig. 28.3
Setup for elbow arthroscopy

Fig. 28.4
Chondral full-thickness lesion

Fig. 28.5
Microfracture

Fig. 28.6
Removal of posteromedial osteophyte with burr
28.6 Treatment Options
Surgical treatment options for MUCL insufficiency generally involve reconstruction of the ligament. Repair of the MUCL is mainly of historical interest only. There is some evidence to suggest that repair of the MUCL may be beneficial in the younger, nonprofessional athlete. Savoie et al. performed a repair using mostly suture anchors in 60 patients (average age 17) and reported good to excellent outcomes in 93 % with return to play at 6 months. There were 4 failures and the average follow-up was 5 years. Other studies have shown higher failure rates with MUCL repair compared to reconstruction [27].
The Jobe technique is the first procedure to describe reconstruction of the MUCL. The procedure involves elevation of the flexor-pronator mass off the medial epicondyle, creation of tunnels in the sublime tubercle and medial epicondyle, and passage of a free graft (usually palmaris longus autograft) in a figure-of-eight fashion. Ten of 16 (68 %) patients returned to previous level of play in his original series [6].
A muscle-splitting approach was described by Smith and Altchek to minimize the morbidity associated with surgical dissection of the flexor-pronator musculature [28]. Twenty-two patients underwent repair or reconstruction using a muscle-splitting approach without neuropathy. It involves tunnel placement and graft passage through the raphe of the flexor carpi ulnaris in the safe interval between the median and ulnar nerves.
Andrews described a modified Jobe technique that involved routine transposition of the ulnar nerve under a fascial sling. Cain et al. reported Andrews’ experience using this technique in 1,281 athletes with 79 % follow-up at 2 years. Eighty-three percent of reconstructions returned to the same level. Sixty-three percent of repairs returned to the same level. Athletes returned to play on average at 11.6 months and initiated a throwing program at 4.4 months.
Altchek coined the docking technique, which involved “docking” of the graft into a single tunnel on the ulna and the humerus with the sutures tied over smaller tunnels to create a bone bridge. This reduces the number of large drill holes in the medial epicondyle from three to one. Dodson et al. described Altchek’s experience using the docking technique in 100 consecutive patients. A subcutaneous ulnar nerve transposition was performed selectively in a few cases. Ninety out of 100 competed at the same level or higher for more than 12 months. There were 2 poor results. There were 3 postoperative complications (2 late ulnar nerve transpositions and 1 arthroscopic lysis of adhesions).
Another technique is called the DANE TJ procedure named to give credit for those who envisioned it (David Altchek, Neal ElAttrache, Tommy John). It involves a hybrid form of fixation with a docking technique proximally and interference screw fixation distally. Dines et al. described the results of the DANE TJ technique in 22 athletes. Nineteen of 22 achieved excellent outcomes, 4 of 22 (17 %) had complications, and 3 required second surgery (2 with arthroscopic lysis of adhesions, 1 with posteromedial osteophyte debridement, all achieved excellent outcomes). Advantages of this technique include its application for revision procedures and sublime tubercle insufficiency where tunnel fracture and/or placement may be potential issues. Proponents of this technique argue that optimal graft tensioning is easier. Ahmad et al. described a technique that involved interference screw fixation proximally and distally in an attempt to more closely recreate ligament isometry [29].
In the initial reports of reconstruction of the MUCL, ulnar nerve transposition was routinely concomitantly performed. However, high incidences of postoperative ulnar neuropraxia led to more selective use of ulnar nerve transposition. When Conway et al. reported Jobe’s 13-year experience, there was transfer of the ulnar nerve in 56 patients that led to 68 % return to previous level of performance, 24 % ulnar nerve-related symptoms(both transient and non-transient), and a 13 % reoperation rate for ulnar nerve-related symptoms [30]. In a later report of 83 patients without nerve transfer using the Jobe technique and the muscle-splitting approach, 82 % returned to their previous level of performance, 5 % had transient nerve-related symptoms, and there were no reoperations [31]. Today most surgeons recommend nerve transposition on a select basis.
Biomechanical studies using a cyclic loading protocol compared the docking technique, figure-of-eight technique, interference screw fixation, and suspensory fixation (Endobutton) [32]. All failed at lower loads than the native MUCL. The docking technique and suspensory fixation showed the highest peak loads to failure. Clinically, excellent outcomes and low failure rates have been obtained with many of these techniques, and none has demonstrated superiority.
28.7 Authors’ Preferred Treatment
We prefer the docking technique as described by Altchek. The first stage of the procedure involves arthroscopy of the elbow, if indicated, to address intra-articular pathology such as chondral injury or posteromedial osteophytes. The graft is then harvested (Fig. 28.7). We use a palmaris longus autograft if available from the ipsilateral or contralateral extremity. If not available, we use a gracilis autograft from the contralateral (plant leg when throwing) lower extremity. The palmaris longus tendon is harvested from a 1 cm incision placed over the volar wrist crease. The visible portion of the tendon is tagged with a no. 1 Ethibond suture in a Krackow fashion. The proximal portion of the tendon is harvested with a tendon stripper. The incision is closed and the tendon is placed in moistened lap sponge.


Fig. 28.7
Harvest of palmaris longus tendon
The arm is exsanguinated and a tourniquet is elevated. We make an 8–10 cm incision over the medial elbow from the distal third of the intermuscular septum to 2 cm beyond the sublime tubercle. Branches of the medial antebrachial cutaneous nerve are identified with vessel loops and carefully retracted. A muscle-splitting approach is developed through the posterior third of the common flexor-pronator mass musculature and within the anterior fibers of the flexor carpi ulnaris (Fig. 28.8). An incision is made longitudinally along the anterior bundle of the MUCL.
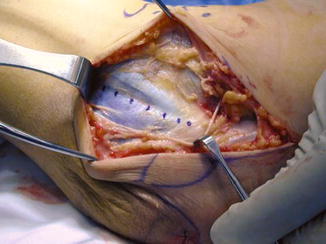
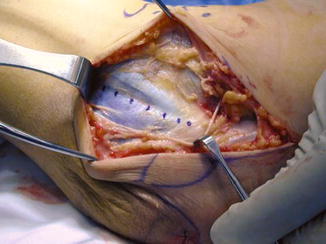
Fig. 28.8
Muscle-splitting approach
The location of the ulnar tunnel is identified after exposing 4–5 mm posterior to the sublime tubercle in a subperiosteal fashion. We use a 3 mm burr for creation of anterior and posterior tunnels on the sublime tubercle with a 2 cm bone bridge between tunnels. The tunnels are connected with a small, curved curette. A suture passer is passed through the tunnels to shuttle looped sutures through them and aid with graft passage. Sutures are passed and tied over the bony bridge after the graft is docked in the ulnar tunnel. The humeral epicondyle is carefully exposed without dissection of the ulnar nerve unless transposition is planned. The origin of the humeral tunnel is identified and a longitudinal tunnel is created using a 4 mm burr. Two smaller anterior tunnels are created with the use of a 1.5 mm burr anterior to the intramuscular septum approximately 5–10 mm apart. The incision in the native MUCL is repaired with 2-0 absorbable suture. Sutures are shuttled through the tunnels using a suture passer and shuttling technique as previously described.
The forearm is supinated and a slight varus stress is applied to the elbow. The limb of the graft with sutures is passed through the ulnar tunnel from anterior to posterior and “docked” into the humeral tunnel with sutures exiting one of the smaller 1.5 mm tunnels. The graft is tensioned in flexion and extension to determine what length is optimal before securing the second limb of the graft in the humeral tunnel. The other limb is marked and a no. 1 Ethibond suture is placed in a Krackow fashion. The excess graft is removed and the graft is docked into the humeral tunnel with the sutures exiting the other 1.5 mm tunnel (Fig. 28.9). The elbow is taking through full range of motion prior to final graft tensioning, and once satisfied, the sutures are tied over the bone bridge on the medial epicondyle (Fig. 28.10). The tourniquet is deflated and hemostasis is obtained. The flexor-pronator fascia is reapproximated and the wound is closed in layers. We perform an ulnar nerve transposition only if indicated based upon preoperative examination. The elbow is placed in a well-padded, plaster splint at 45° of flexion.










