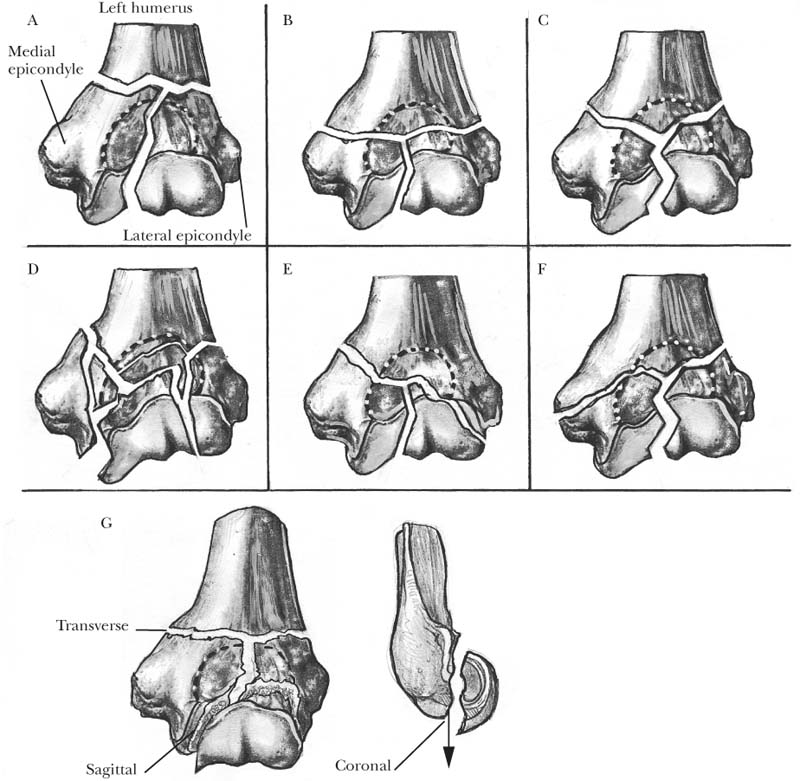
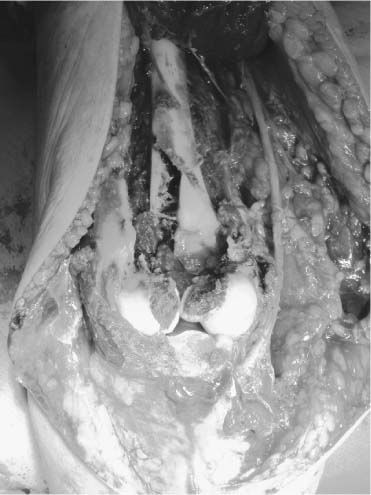
5 Although intra-articular distal humerus fractures constitute less than 2% of all fractures treated, there has been much attention paid to their method of treatment because traditionally they have proven to be some of the most challenging fracture patterns faced by orthopedic surgeons.1–3 Recommendations have included conservative treatment, open reduction with extensive internal fixation, and total elbow arthroplasty.4–9 The elbow can be envisioned as a constrained hinge joint with a single axis of rotation (flexion-extension) at the ulnohumeral articulation.10 As the distal end of the humerus splits into the two columns, the trochlea interconnects these diverging columns, giving rise to the appearance of a functional triangle at the distal humerus. Understanding of this functional anatomy is essential to biomechanical reconstruction of the distal humerus. Should there be a fracture or disruption of any one of the arms of this triangle, the entire distal humeral construct is weakened.11 Thus, rigid internal fixation of all three arms is required for effective stabilization of the fractured distal humerus. The radiocapitellar articulation at the elbow is often considered separate from the ulnohumeral articulation. The radiocapitellar joint functions predominantly in pronation and supination and as such is independent from the motion at the ulnohumeral joint. Biomechanically, however, the radiocapitellar joint provides for secondary bony stabilization of the ulnohumeral joint throughout its range of motion. The functional triangular construct of the humerus from the posterior view contains the olecranon fossa, a central triangular depression that accommodates the proximal tip of the olecranon in full extension and contains the posterior fat pad. This layer of fatty tissue may become adherent to the olecranon fossa after injury or immobilization, resulting in elbow stiffness. The medial column diverges from the shaft of the humerus at an approximate 45 degree angle. Whereas the proximal two thirds of the column is composed of cortical bone, the distal one third containing the medial epicondyle is composed of cancellous bone. Anteriorly, the supracondyloid process, which lies 7 cm proximal to the medial epicondyle, provides a reliable landmark to the medially displaced median nerve and a possible site of proximal brachial artery bifurcation into the radial and ulnar arteries.12 The medial epicondyle serves as the origin of the anterior and posterior bundles of the ulnar collateral ligament, as well as the flexor mass of the forearm. Just below the medial epicondyle lies the cubital tunnel with its constituent ulnar nerve. After an anterior ulnar nerve transposition, it is important to realize that the inferior surface of the medial epicondyle becomes available for internal fixation of both the medial column and the inferior base of the distal humeral triangle. The lateral column of the distal humerus diverges from the shaft at the same level as the medial column at an approximate angle of 20 degrees. The proximal half of this column is broad, flat, and composed of cortical bone; thus, it is ideal for plate fixation. The distal half of the lateral column beginning at the level of the mid olecranon fossa is composed predominantly of cancellous bone, and distally it curves anteriorly into the cartilage cap of the capitellum. The blending of the lateral distal humeral ridge into the lateral column characterizes the lateral supracondylar ridge, where the extensor carpi radialis longus and brachioradialis muscles originate. At its terminal end lies the lateral epicondyle, which is smaller than the medial epicondyle and serves as the origin of the lateral collateral ligament. Although not as distinct as the ulnar collateral ligament, the lateral collateral ligament blends into the annular ligament and the common extensor origin, with its anterior fibers inserting on the supinator crest of the proximal ulna. The common extensor origin lies posterior to the lateral tip of the epicondyle. More distally on the anterior surface of the lateral column a shallow depression is formed, the radial fossa, which abuts the cartilage-capped capitellum. The capitellum is an incomplete hemisphere, having an arc of 180 degrees in the sagittal plane, whereas the trochlea has an arc of 270 degrees. The rotational center of the capitellum is displaced 12 to 15 mm anterior to the humeral shaft axis, which brings it in alignment to the trochlear axis, allowing the ulna and radius to range in the same coaxial plane. FIGURE 5-1. Classification of distal humerus fractures. Refer to text for explanation of each type. Fractures of the distal humerus can be divided into three major groups: extracapsular fractures, transcolumn (transcondylar or supracondylar) fractures, and intra-articular fractures. Extracapsular fractures involving the medial or lateral epicondyle are uncommon after physeal closure. Subclassified as type A (extra-articular) fractures by the Muller13 classification (Figure 5-1), these fracture patterns are associated with metaphyseal comminution and amenable to either operative or nonoperative treatment. Transcolumn fractures are intracapsular and extra-articular and are subclassified as type A fractures by the Muller13 classification. They are associated with an increased likelihood of neurovascular injury, and a detailed neurovascular exam of the upper extremity should be undertaken on presentation.14 Intra-articular fractures, subclassified as type B (partial intra-articular) or C (complete intra-articular) fractures per the Muller13 classification, can have either single-column or bicolumn involvement. The single-column fracture patterns are subdivided as high and low. The high fracture patterns include the majority of the trochlea and are unstable, and the ulna and radius displace with the fracture fragment. Internal fixation, however, is reliable because of the dimensions of the distal fragment. In contrast, the low, single-column fractures share the exact contradistinctions. Intra-articular bicolumn fracture patterns are the most common type of distal humerus fractures and are considered to be some of the most difficult to treat as they disrupt all three segments of the distal humeral triangle. Bicolumn fractures are subdivided into the following types: Transcolumn fractures are often the result of a fall onto an outstretched hand with a posteriorly directed force on a flexed elbow. Flexion injuries resulting from application of an anteriorly directed force on the posterior aspect of the distal humerus are less common.16 It has been suggested that the mechanism of injury for single-column fractures involves the application of a large abducting or adducting force to the distal humerus during a direct blow or a fall onto an outstretched hand.17 The varus or valgus moment applied to the elbow during injury often results in associated collateral ligament injury, which is often noted at the time of surgery.18 In the past, investigators believed that bicolumn fractures resulted from the wedging effect of the olecranon on the distal humerus following a fall onto a flexed elbow.19 With subsequent cadaveric studies at the University of Southern California and the Imperial College of London, this understanding has been further modified. It was demonstrated that a direct force applied to an elbow flexed at 90 degrees reproduced a transverse olecranon fracture. However, when the elbow was hyper-flexed to 110 degrees, bicolumn fractures of the distal humerus occurred (Figure 5-1F).20 Nonoperative surgical treatment of distal humerus fractures can be utilized for stable type A fracture patterns. With the application of axial traction in neutral rotation, the distal humerus fracture can be closed reduced and immobilized in a splint, cast, or hinged fracture brace. The latter option provides for early elbow motion, decreasing the risk of elbow stiffness.21 This mode of treatment requires frequent and regular radiographic follow-up and may entail multiple adjustments to the splint or brace in the early phases of healing. Nonoperative management of types B and C distal humerus fractures has not been recommended, as they have been shown to result in compromised functional outcome due to poor articular reduction and incongruity.22 The clinical results obtained from the availability and use of rigid implants for the stabilization of distal humerus fractures have encouraged many authors to support the treatment option of open reduction and internal fixation.19,23–25 The advantages of open reduction and internal fixation over conservative management are especially significant in intra-articular (types B and C) distal humerus fractures. First, when displacement of the articular surface is present, operative management is required to accomplish anatomic reduction of the joint surface in an attempt to prevent post-traumatic arthritis following malreduction.19,23,26 Second, stable internal fixation allows for early range of motion of the elbow while maintaining fracture reduction, and elbow stiffness is minimized. Total elbow arthroplasty has been proposed as an alternative treatment for severely comminuted intra-articular distal humerus fractures in elderly patients because the poor bone stock in conjunction with the comminution may preclude stable fixation.8,9 The experience with this method is limited, however. Formal preoperative planning is highly recommended for open reduction and internal fixation of distal humerus fractures. In conjunction with anteroposterior and lateral views of the contralateral extremity, traction films of the injured extremity will better delineate the size and position of the fracture fragments.27 Other imaging techniques, such as CT and MRI, have not been recommended in the preoperative evaluation of intra-articular distal humerus fractures.6 Following evaluation of the fracture pattern, the surgical approach and the selection of implants should be considered. The type, number, position, and length of plates and screws are determined on a preoperative drawing. The procedure is usually a demanding and lengthy one. Therefore, it is recommended that surgical intervention be undertaken when trained assistants and operating room personnel are available and equipment is complete. The surgeon should request a sterile tourniquet, sharp osteotomes, an oscillating saw, dissecting instruments, a bone graft harvesting tray, smooth K-wires, Weber clamps, and suture anchors. According to the fracture pattern, a variety of implants may be used. A large fragment, small fragment, pelvis fracture, and cannulated screw instrument set, reconstruction plates, plate benders, precontoured anatomic plates, modular hand plates and screws, and Herbert screws should be readily available to the surgeon. If an olecranon osteotomy will be used, large (6.5 or 7.3 mm) cannulated screws or 18-gauge wire should also be available. General endotracheal anesthesia is preferred, because an axillary block may not provide adequate analgesia that lasts throughout the course of the procedure. Moreover, iliac crest bone graft may need to be harvested. Following induction of anesthesia, the patient is placed in the lateral position with the involved extremity on top. An axillary roll is placed beneath the dependent side just distal to the axilla, and the patient is secured into position using a beanbag. The affected extremity is supported over a roll of folded drapes so that it remains off the chest wall. The lateral position is preferred over the supine for two reasons. First, by allowing the forearm to hang over the roll, gravity helps maintain the fracture in a relatively reduced position, whereas in the supine position, an assistant is required to hold the extremity over the chest. Second, access to the iliac crest is facilitated, and a second surgeon could harvest iliac crest bone graft simultaneously, if needed. The whole upper extremity, as well as the iliac crest region, is prepped and draped in the usual fashion, and a sterile tourniquet is placed in the upper arm. The upper extremity should be free, and full flexion and extension of the elbow should be possible without obstruction. The transolecranon approach is very useful for intra-articular fractures of the distal humerus, especially when comminution is present (Figure 5-2). This approach is based on osteotomy of the olecranon in order to fully expose the articular surface of the distal humerus. The excellent visualization of the distal humerus, including the articular surface, constitutes the advantage of this approach. The accuracy of reduction of the articular fragments can be meticulously assessed under direct visualization, and fixation can be facilitated. The disadvantage of the transolecranon approach lies in the extra steps of the olecranon osteotomy and fixation. Nevertheless, the additional time is well compensated by the facilitation of the procedure afforded by this approach. Nonunion of the osteotomy site is a rare problem that can be avoided by stable fixation.
Intra-articular Distal Humerus Fractures
Anatomy
Classification
Mechanism of Injury
Treatment
Nonoperative Treatment
Operative Treatment
Preoperative Planning
Anesthesia and Preparation
Surgical Approach
Intra-articular Distal Humerus Fractures
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








