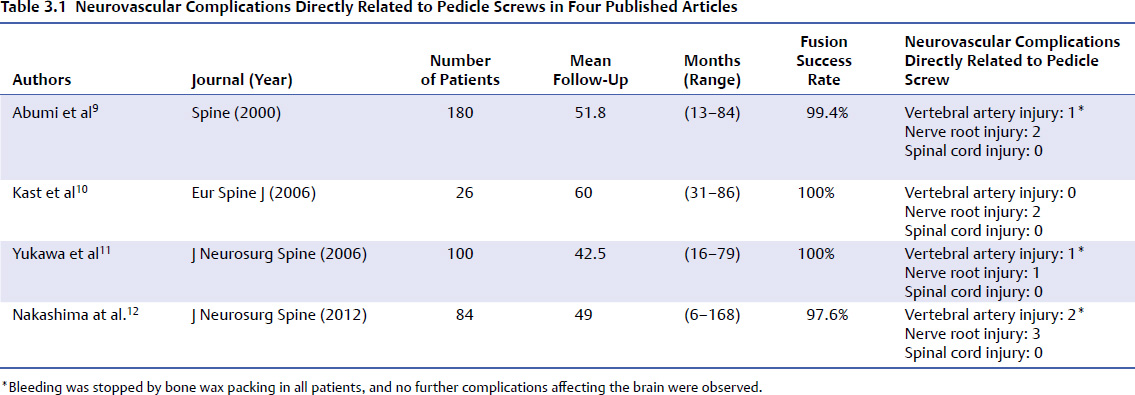
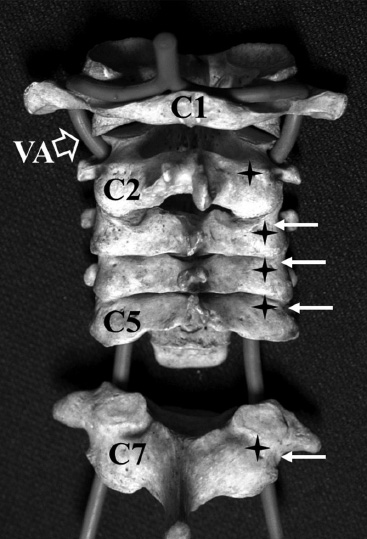
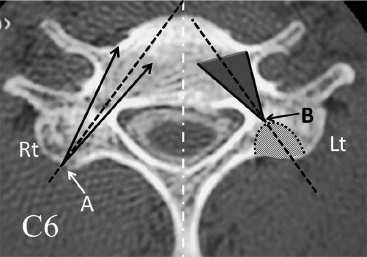
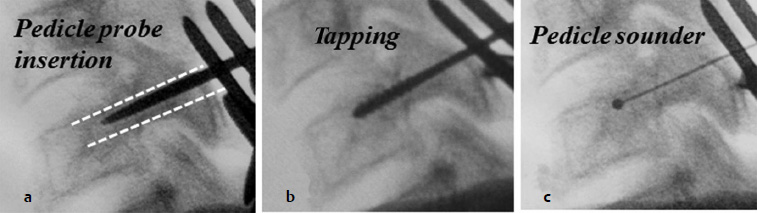
3 Despite the increasing acceptance among spine surgeons of the use of pedicle screws in the lumbar and thoracic spine, screw insertion into the cervical pedicle has been considered too risky for the surrounding neurovascular structures, except at C2 and C7. Leconte1 first reported C2 pedicle screw insertion for osteosynthesis of the C2 hangman fracture, and Roy-Camille et al2 documented screw insertion into C7 pedicles. However, there had been no report of pedicle screw insertion through C3 to C6 until 1994, with Abumi et al’s3 description of the techniques and their report of 13 cases of pedicle screw fixation for traumatic lesions of the lower cervical spine, and with Jeanneret et al’s4 report of three cases of osteosynthesis of a separation fracture of the articular mass in the middle cervical spine. Biomechanical studies have demonstrated the superior stabilizing effect of pedicle screw fixation over other internal fixation procedures in the cervical spine.5,6 The biomechanical studies of Johnston et al7 and Ito et al8 demonstrated that cervical pedicle screws entail a significantly lower rate of loosening at the bone–screw interface and greater strength in fatigue testing. However, even for surgeons who are experienced with the placement of cervical pedicle screws, neurovascular complications, including injury to the vertebral artery and nerve root, cannot be completely eliminated (Table 3.1).9–12 The screw malposition rate by the freehand technique in patients with complicated anatomic conditions such as rheumatoid arthritis or severe spondylosis is especially high. In recent years, modified screw insertion techniques, guiding devices, and computer navigation systems have been developed and have improved the accuracy of screw insertion.13–16 Pedicle screw fixation is a powerful tool for stabilization of unstable motion segments caused by injuries or by nontraumatic lesions including metastatic tumor, rheumatoid arthritis, and destructive spondyloarthropathy. This procedure is especially beneficial in several settings in which laminae or lateral masses may be inadequate for anchor placement due to previous resection of the posterior elements or marked osteoporosis. In addition, rigid fixation with cervical pedicle screws provides excellent correction capability to restore the physiological sagittal alignment of the cervical spine. Furthermore, it can be utilized as the cervical anchor for occipitocervical reconstruction.17,18 Degenerative cervical spine with segmental instability requiring posterior decompression also can be managed by simultaneous decompression and stabilization using pedicle screw fixation.19 It is recommended that the surgeon stand at the head of the patient, to ensure symmetrical insertion of the right and left screws. The assistant surgeon usually stands on the left side of the patient. The C-arm monitor is placed at the left side of the patient near the pelvis to provide the leading surgeon with a good view. The patient is placed prone on a four-post frame using a horseshoe-type headrest or three-point pin fixation device. The shoulders are pulled caudally by a heavy bandage for intraoperative lateral fluoroscopic imaging of the lower cervical spine. The cranial end of the bandage must be applied on the acromion to obtain sufficient pulling force. A skin incision, longer than required for a standard spinous process wiring, is made. The cranially adjacent lamina of the most cranially fixed vertebra should entirely be exposed, taking care to protect the cranial facet joint capsule. The paravertebral muscles are dissected laterally to expose the lateral margins of the articular masses completely for exact determination of the screw insertion point. The points of screw insertion at the lateral mass from C3 through C7 are slightly laterally to the center of the articular mass and close to the inferior margin of the inferior articular process of the cranially adjacent vertebra. Surgeons must carefully evaluate preoperative computed tomography (CT) images before screw insertion to check the shape and the size of the pedicle and lateral mass in each vertebra and in each individual. The cranial margin of the lamina of C2 is the landmark for the point of screw insertion for C2. To confirm the screw insertion points in C2, a Penfield retractor can be inserted into the spinal canal along the cranial margin of the C2 lamina to the medial surface of the pedicle of C2. The angle of the C2 pedicle axis to the sagittal plane is 15 to 25 degrees in the transverse plane. The lateral margin of the articular mass of the cervical spine has a notch approximately at the same level of the pedicle. Precisely, the pedicles are located slightly below the lateral vertebral notch at C2, at C3 to C6, and at, or slightly above, the notch at C7 (Fig. 3.1). The points of the screw starting at the C3 through C7 pedicles are slightly laterally to the center of the articular mass and close to the inferior margin of the inferior articular process of the cranially adjacent vertebra. Confirmation of the screw starting point for C7 using lateral C-arm projection may be disturbed by the shoulder girdle in many patients. For these patients, a small laminotomy at the cranial margin of the C7 lamina is helpful to see and touch the pedicle directly through the laminotomy portion. A craniocaudal orientation of the screw insertion point can be confirmed by a lateral image intensifier. The authors usually create a funnel-shaped hole at the screw insertion point using a high-speed bur with a diamond tip. The direction of the pedicle’s anatomic axis in the transverse plane varies from a minimum at the C2 pedicle to a maximum at the C5 pedicle. However, after resection of the outer surface of the articular mass to create a hole with a funnel-like shape down to the entrance of the pedicle with a high-speed bur, surgeons can have a wider range of freedom for determining the screw insertion angle from the entrance of the pedicle cavity (Fig. 3.2). Therefore, after creating a funnel-like hole, a screw can be inserted by a smaller oblique angle than the angle of the true anatomic axis of the pedicle. The authors usually insert screws with angle of 25 to 45 degrees from the sagittal plane for the pedicle from C3 to C7. A thin, specially designed pedicle probe, a tap, and screws are inserted into the pedicle under the guidance of lateral C-arm image to confirm the direction and insertion depth. The authors recommend confirming the proper creation of the screw insertion path with a cervical pedicle sounder with a small ball tip after probing and tapping (Fig. 3.3). Fig. 3.1 Pedicle screw starting points in the cervical spine. The cranial margin of the lamina of C2 can be the landmark for the point of screw penetration for C2 (* sign). To confirm the screw insertion points in C2, a small spatula can be inserted into the spinal canal along the cranial margin of the C2 lamina to the medial surface of the pedicle of C2. The lateral margin of the articular mass of the cervical spine has a notch (white arrows). The screw starting points are located approximately below the lateral vertebral notch at C2, at C3-C6, and at, or slightly above, the notch at C7. The screw starting points (* signs) are 2 to 4 mm medially from the notch. VA, vertebral artery. The angle of screw insertion in the sagittal plane should be parallel to the upper end plate for the pedicles of C5 through C7, and a slightly cephalad direction in C2 through C4, based on the anatomic angle of the pedicle in the sagittal plane. A drill bit should not be used for making holes for screw placement. When the neurocentral junction in the cervical spine close to the base of the pedicle in the vertebral body is too hard to pass a pedicle probe, the junction can be gently perforated with a Kirschner wire or a high-speed diamond bur with its smallest tip; the tip of the wire or bur must not go deeper but only make the path for a pedicle probe to enter the vertebral body. Cervical pedicles without a medullary canal because of sclerotic changes or an extremely small diameter are not suited for pedicle screw insertion because of the high possibility of screw malposition. In patients with marked degenerative changes in the lateral mass of the cervical spine, the location of the starting point of the pedicle screw is difficult to determine. In such cases, the insertion point for the pedicle screw can be visualized after resecting the proliferated lateral mass using a high-speed bur. Fig. 3.2 Direction of the cervical pedicle screw. The black broken line indicates the anatomic axis of the pedicle. Point A on the right (Rt) side of the lateral mass is the screw insertion point. The screw can be inserted between the two black arrows. After resection of the outer portion of the lateral mass toward the entrance of the pedicle cavity as a funnel-like shape using a high-speed bur (shaded portion on the left [Lt] side of the pedicle and vertebral body), the starting point of the screw approach is at the entrance of the pedicle cavity (point B), and the surgeon obtains more freedom in determining the screw insertion angle.
Indications and Techniques of Cervical Pedicle Screws C3-7 for Degenerative Conditions
 Introduction
Introduction
 Indication and Contraindication
Indication and Contraindication
 Surgical Procedures
Surgical Procedures
Positioning and Exposure
Screw Placement
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree