50 Hand and Wrist Pain
Patient Evaluation
Anatomy
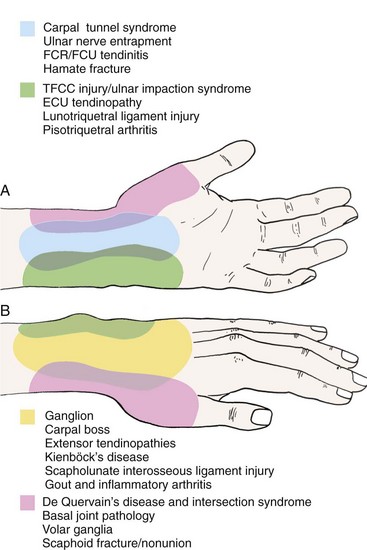
The complex anatomy of the hand and wrist involves many structures interacting in close proximity to one another. Several different diagnoses can manifest with similar symptom patterns despite varying pathologies. A precise knowledge of the anatomy of the hand and wrist often eliminates several diagnostic considerations on the basis of the physical examination alone. The history of the illness and the examination also help to narrow further investigation by enabling the physician to choose appropriate additional diagnostic tests better. Several common sites of pain in the hand and wrist and their corresponding leading diagnoses are illustrated in Figure 50-1. Pain in one location can have multiple etiologies depending on the patient profile and the history of the problem. A thorough review of the pertinent regional anatomy is important to help differentiate successfully the many possible causes of hand and wrist pain.
Physical Examination
Imaging Studies
If further detail of the bony anatomy is required, computed tomography (CT) is the best available tool today. The most common uses for CT in the hand and wrist include evaluation of intra-articular fractures of the distal radius and metacarpals, scaphoid fractures and nonunions, and intraosseous cysts or tumors.1,2
Advances in ultrasound and MRI technology have enhanced the ability to evaluate the soft tissue structures of the hand and wrist. Smaller ultrasound probes with higher resolution have made it possible to visualize and differentiate structures such as flexor tendons, ganglion cysts, and ligaments. Doppler ultrasound can help to differentiate vascular disorders of the hand. MRI technology is constantly improving and allowing for new uses in the hand and wrist. By altering the parameters of this test, information about anatomy and physiology can be obtained.3 Specific uses of these tests and others such as arthrography and bone scans are addressed with the diagnoses for which they are most useful.
Additional Diagnostic Tests
Neurodiagnostic Tests
Neurodiagnostic tests including nerve conduction studies and electromyography are useful in the diagnosis of suspected neurologic disorders of the upper extremity. Specifying the type and nature of examination required enhances the information gained by these studies. If a nerve compression syndrome such as carpal or cubital tunnel syndrome is suspected, nerve conduction studies may be sufficient without the added cost and patient discomfort of formal electromyography testing. Nerve conduction studies evaluate the speed of conduction of motor and sensory nerves across a set distance at a specific location and compare this with established normal values. A decrease in the speed of nerve conduction, as evidenced by an increase in the latency, is seen with localized nerve compression and is shown in several different nerves concomitantly in demyelinating diseases such as multiple sclerosis. When more severe nerve injuries are suspected or if there is clinical evidence of muscle weakness or atrophy, an electromyogram can be useful to delineate better the extent of the process or rule out a myopathic process.4
Injections and Aspirations
The use of injections and aspirations can be therapeutic and diagnostic. A so-called lidocaine challenge can be used to discriminate between different diagnoses when placed precisely in one joint or painful area. Corticosteroids can be given selectively in conjunction with the local anesthetic for more lasting relief and in some cases can be curative.5–11 Some of the most common sites for injection are the A1 pulley region of the finger for trigger finger, the carpal canal for carpal tunnel syndrome, and the first dorsal compartment of the wrist for de Quervain’s disease.
Aspiration of joints or other fluid collections such as ganglia can yield vital diagnostic information and can be therapeutic. If infection is suspected, aspiration should be used to obtain a sample of joint fluid for Gram stain, cell count, and culture. Diagnoses such as gout and pseudogout can be confirmed by crystal analysis under polarized light. Many ganglia and retinacular cysts can be treated temporarily or permanently with simple aspiration.12,13
Arthroscopy
Direct visualization of a joint via arthroscopy can be an invaluable diagnostic tool. Despite the increasing sensitivity of imaging techniques such as MRI, arthroscopy provides a dynamic evaluation that static imaging cannot provide.14 Since the first published report of a series of cases by Roth and colleagues in 1988,15 it has become the “gold standard” for evaluation of chronic wrist pain.16–18 With new surgical techniques being developed, surgeons often can proceed directly to the definitive treatment using arthroscopy entirely or in part.19–24
Common Etiologies for Hand and Wrist Pain
Wrist Pain: Palmar
Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is the most commonly diagnosed compression neuropathy in the upper extremity. It usually occurs as an isolated phenomenon, but symptoms of CTS can accompany many systemic diseases such as congestive heart failure, multiple myeloma, and tuberculosis.25–28 More commonly, CTS is associated with conditions such as pregnancy, diabetes, obesity, rheumatoid arthritis, and gout.29–39
The classic constellation of symptoms consists of nocturnal paresthesias in the affected digits; paresthesias or hypesthesias in the thumb, index, and long fingers; and weakness or clumsiness of the hand. Patients often complain of forearm and elbow pain that is aggravated by activities but is poorly localized and aching in nature. Occasionally, more proximal symptoms such as shoulder pain are the main presenting complaint.40 Past reports have indicated a 3 : 1 prevalence of CTS in women. Approximately half of patients are 40 to 60 years old, although CTS has occasionally been diagnosed in children.41,42
The diagnosis of CTS is usually clinical. Tinel’s sign, shown by radiating paresthesias in the median nerve distribution with gentle percussion over the volar wrist, indicates nerve irritation. Reproduction of symptoms with wrist flexion, as described by Phalen,43 and with the carpal compression test, as described by Durkan,44 has been shown to be more specific.45 Decreased sensibility and thenar atrophy are late signs seen in advanced median nerve entrapment. Bilateral electrodiagnostic tests, specifically nerve conduction velocity testing, should be used to confirm the diagnosis, particularly in patients claiming a compensable injury or in patients with atypical signs or symptoms. Prolonged motor and sensory latencies across the carpal canal confirm pathologic compression of the median nerve.46–48 In patients with classic clinical findings, a study found that CTS could be diagnosed with a high degree of accuracy on clinical grounds alone and that the addition of electrodiagnostic tests did not increase the accuracy.49 When attempting to differentiate CTS from more proximal nerve entrapments such as cervical root compression or thoracic outlet syndrome, the addition of electromyography of the cervical paraspinal muscles and proximal conduction tests (H reflex, f waves) can be useful.50
Conservative treatment for CTS consists of splinting of the wrist in neutral position and consideration of oral nonsteroidal anti-inflammatory drugs (NSAIDs) for pain control. Splinting should be used sparingly during the workday to prevent secondary muscle weakness and fatigue but is best prescribed to prevent provocative wrist positioning at night. The splint should not hold the wrist in extension beyond 10 degrees (Figure 50-2). Although splinting may be beneficial for relief of symptoms in cases of mild compression, its long-term effectiveness is limited.51 The use of vitamin B6 (100 to 200 mg/day) has been helpful in some cases, but its efficacy has not been confirmed in a randomized trial. The popularity of injections of corticosteroid in the treatment of CTS has waxed and waned over the last half century. Although it has been shown to be quite effective in the short term, the long-term efficacy is mixed.52–54 Also, injections have been associated with exacerbation of the condition and permanent median nerve injury if performed incorrectly.55,56 For these reasons, injections are most often indicated in cases when the condition is thought to be temporary such as with pregnancy or if surgery must be deferred because of a medical condition or major life event.
Surgical release is indicated for patients with confirmed CTS who have failed a course of conservative treatment. In patients who exhibit late findings of objective sensory loss or thenar atrophy, early surgery should be recommended. The incision for a modern carpal tunnel release is not more than 3 cm long and parallels the skin creases of the palm (Figure 50-3).
Ulnar Nerve Entrapment: Cubital Tunnel Syndrome
Electrodiagnostic studies can help to confirm the diagnosis and differentiate cubital tunnel syndrome from more distal compression of the ulnar nerve in Guyon’s canal (see later). If malalignment of the elbow is present or the patient relates a history of childhood trauma, radiographs should be obtained to rule out a supracondylar or epicondylar malunion. So-called tardy ulnar nerve palsy can develop years after a supracondylar fracture of the elbow.57
Ulnar Nerve Entrapment: Guyon’s Canal
In 1861 Guyon58 published a description of the contents of an anatomic canal at the wrist. The distal branches of the ulnar nerve and the ulnar artery pass through this space. As it exits the canal, the ulnar nerve divides into its sensory and motor branches. Compression of the nerve within or proximal to the canal usually manifests with a combination of sensory and motor symptoms in the ulnar nerve distribution. Patients complain of numbness and paresthesias of the palmar aspect of the ring and small fingers. Motor symptoms are usually described as a cramping weakness with grasping and pinching. As with median neuropathy, atrophy of the intrinsics and objective sensory loss are late findings.
In contrast to carpal tunnel syndrome, in which patients usually have an ill-defined onset of symptoms, ulnar nerve compression in the canal of Guyon is often of more acute onset. It can be associated with repeated blunt trauma,59–61 a fracture of the hamate or the metacarpal bases, or occasionally a fracture of the distal radius.62,63 Space-occupying lesions such as a ganglion, lipoma, or anomalous muscle can also cause compression.64–68 Because of the difference in etiology, this nerve entrapment syndrome is often not amenable to conservative treatment. If there is an anatomic lesion such as a fracture or a mass, this must be addressed. If repetitive blunt trauma is the cause, without associated fracture or arterial thrombosis, splinting and activity modification can alleviate the symptoms.
Flexor Carpi Radialis and Flexor Carpi Ulnaris Tendinitis
Similar to other tendinopathies around the wrist, irritation of the wrist flexors occurs with stress of the wrist in a particular position. Activities that require forced wrist flexion for prolonged periods or with repetition put patients at risk for inflammation around the flexor carpi radialis tendon69 or the flexor carpi ulnaris tendon or both. The condition manifests with tenderness along the course of the tendon, especially near its insertion. Wrist flexion against resistance with radial or ulnar deviation reproduces the symptoms. Treatment consists of splinting and rest, elimination of activities that cause pain, and oral NSAIDs. Injection of corticosteroid into the flexor carpi radialis or flexor carpi ulnaris sheath may be curative. Sharp pain, associated with an intense inflammatory localized reaction, is suggestive of calcific tendinitis and is most commonly seen around the flexor carpi ulnaris tendon.70,71 If calcific tendinitis is suspected, a plain radiograph can be useful in confirming the diagnosis but the calcification may not become apparent for 7 to 10 days after the onset of symptoms.
Hamate Fracture
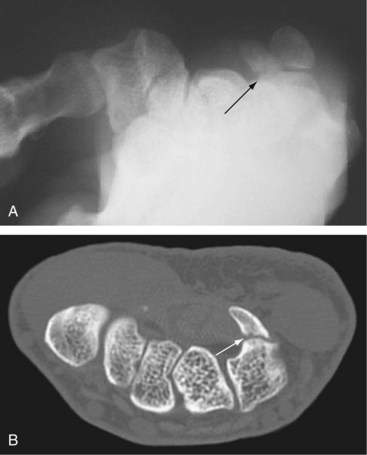
An uncommon and underdiagnosed etiology of palmar pain in young, active individuals is a fracture of the hook of the hamate. These fractures can occur from a fall on an extended wrist, a “dubbed” golf shot, or from forcefully striking a ball with a club or bat. Plain radiographs of the wrist are usually read as normal. The condition should be established and treated expeditiously because it may lead to ulnar nerve entrapment, ulnar artery thrombosis, or rupture of flexor tendons.72 Pain in the base of the palm overlying the hamate is the most common presenting symptom. Often, the pain is present only with the activity that caused the fracture such as driving a golf ball or swinging a bat. Because of the proximity of the ulnar nerve, patients also can have sensory and motor symptoms of distal ulnar neuropathy. Occasionally, in the acute setting, vascular complaints such as cold intolerance or frank ischemia from ulnar artery thrombosis can be the presenting condition.
A carpal tunnel view, obtained with the wrist in a hyperextended position, may show the fracture (Figure 50-4A). Alternatively, a selective CT scan through the hamate is a more accurate way to confirm the diagnosis (Figure 50-4B).73 If diagnosed within 2 to 3 weeks of injury, casting should be attempted to allow the fracture to heal.74 If this fails or if the fracture is diagnosed late, surgical treatment is indicated, and most authors favor excision of the hook followed by a gradual return to activities.75–78
Wrist Pain: Dorsal
Ganglion
Ganglia account for 50% to 70% of all soft tissue tumors of the hand and wrist. Of these, 60% to 70% occur around the dorsal wrist. These mucin-filled cysts usually arise from an adjacent joint capsule or tendon sheath. The most common site of origin is the scapholunate ligament, and the main body of the cyst may be located elsewhere on the dorsum of the wrist and attached to this ligament by a long pedicle. Although most ganglia occur as a well-circumscribed and obvious soft mass, some are subtler and are evident only with the wrist in marked volar flexion. As a result of their characteristic appearance, ganglia are not often misdiagnosed but should be differentiated from the less well-demarcated swelling of extensor tenosynovitis, lipomas, and other hand tumors. Plain radiographs are usually normal but occasionally show an intraosseous cyst or an osteoarthritic joint. Some ganglia may not be clinically apparent and are known as “occult” ganglia. Ultrasound and MRI have been shown to be useful in the diagnosis of these ganglia.79,80
Most conservative measures such as splinting and rest have only a temporary effect on ganglia. They tend to diminish in size with rest and enlarge with increased activity. Spontaneous rupture is common, and at one time attempting to rupture the cyst with a heavy object such as a large book was recommended as treatment. Aspiration can be performed but has mixed results because of the thick gelatinous nature of the fluid within the cyst. Even if adequate decompression of the cyst can be achieved, reaccumulation of the fluid usually occurs. Aspiration in conjunction with irrigation or injection of corticosteroids can be effective in alleviating the symptoms for varying periods of time.12,13,81
Occasionally, a ganglion can become so large that it can interfere with the function of the wrist by limiting the motion, especially in extension. Pressure of the mass on the terminal branches of the posterior interosseous nerve may be painful. Excision is generally curative but may result in short-term stiffness and some loss of terminal flexion secondary to surgical scarring. Occasionally, a patient desires excision of the cyst for cosmetic reasons. With proper excision, recurrence is less than 10%,82–84 but if the dissection is incomplete and fails to identify the origin of the cyst, recurrence rates can be 50%. Arthroscopic resection has been shown to be a safe and effective method of treating dorsal wrist ganglia.23,24
Carpal Boss
Often confused with a dorsal ganglion, the carpal boss is a bony, nonmobile prominence on the dorsum of the wrist. It is an osteoarthritic spur that forms at the second or third carpometacarpal joints.85 The boss is most evident with the wrist in volar flexion. Patients usually present with pain and localized tenderness over the prominence. The condition is twice as common in women as in men, and most patients are in their 20s to 30s. It is not unusual for a small ganglion to be associated with the boss. Radiographs are best taken with the hand and wrist in 30 to 40 degrees of supination and 20 to 30 degrees of ulnar deviation to put the bony prominence on profile (the “carpal boss view”).86 Conservative treatment consists of rest, immobilization, NSAIDs, and occasionally injection with corticosteroids. If persistently painful despite these measures, surgical excision of the boss may be necessary but is associated with a prolonged recovery and continued symptoms in a high percentage of patients.
Extensor Tendinopathies
Commonly, a patient may present with a rupture of the EPL without antecedent pain or swelling. There is a well-known association of EPL rupture with fractures of the distal radius that likely occurs owing to a relative “watershed zone” of vascular supply within its tight retinacular sheath. Tendon rupture most often occurs with minimally displaced or nondisplaced fractures and can occur several weeks or months after the original injury.87–90 Individuals with RA and systemic lupus erythematosus are especially prone to rupture of the EPL and other tendons.
Kienböck’s Disease
Kienböck’s disease is so named for Kienböck,91 who first described in 1910 what he postulated were avascular changes in the lunate. Nearly a century later, the cause of this disease remains unclear; it is likely multifactorial. Kienböck’s disease should be suspected when a young adult presents with pain and stiffness of the wrist and swelling and tenderness around the region of the dorsal lunate. There is an increased propensity of the disease among patients with an ulna that is anatomically shorter than the radius (so-called ulnar negative variance). Radiographs are needed to confirm and stage the process. Kienböck’s disease is staged by the degree of fragmentation and collapse of the lunate, associated osteoarthritis, and carpal collapse in a system originally proposed by Stahl.92 In this system, the earliest sign of the disease is a linear or compression fracture in the lunate. Later stages show sclerosis of the lunate, followed by lunate collapse and a loss of carpal height. In the final stage the carpus shows signs of diffuse osteoarthritis with complete collapse and fragmentation of the lunate (Figure 50-5). With the increased sensitivity of MRI, it is possible to identify avascular changes within the lunate before they become evident on plain radiographs. This is referred to as “stage zero” Kienböck’s disease.
The treatment for Kienböck’s disease is largely surgical. Depending on the stage of the disease and the postulated etiology, several surgical procedures have been described. In early stages of the disease, when there is little lunate collapse and no osteoarthritis, the goal of surgery is to “unload” the lunate by redistributing articular contact forces and allow it to revascularize.93–96 The most common procedure is a radial shortening osteotomy, performed to neutralize ulnar variance. In later stages, various intercarpal arthrodeses have been used to readjust and maintain carpal height and alignment.97–99 Microsurgical techniques have been used more recently to revascularize the lunate with promising early results.100
Scapholunate Interosseous Ligament Injury
The interosseous ligament between the scaphoid and the lunate is a stout structure, especially dorsally, and usually requires a significant force to cause disruption. The typical mechanism of injury is a fall onto the outstretched hand with the wrist extended. Early diagnosis is essential to prevent the late sequelae of carpal collapse. The key radiographic features of scapholunate dissociation (scapholunate interval widening) are shown in Figure 50-6. The anteroposterior view shows the scapholunate interval better than the posteroanterior view.101 Early surgical intervention is recommended with the goals of maintaining carpal alignment and preventing an otherwise inevitable progression to carpal collapse and degenerative arthritis.
Gout and Inflammatory Arthritis
All of the inflammatory arthritides including the crystal arthropathies can manifest as dorsal wrist pain. Approximately 25% of patients with a diagnosis of RA present initially with hand and wrist symptoms. The reader is referred to Chapters 94 to 96 for further details.
Wrist Pain: Ulnar
Triangular Fibrocartilage Complex Injury and Ulnocarpal Impaction Syndrome
One of the most complex and confusing areas of the wrist from a diagnostic standpoint is the articulation of the ulna with the carpus. The triangular fibrocartilage complex (TFCC), so named by Palmer and Werner,102 comprises the articular disk itself and the immediately surrounding ulnocarpal ligaments. It can be injured by a variety of acute and chronic mechanisms. Hyperpronation and hypersupination of the carpus during forceful activities are the usual causes of acute injuries, whereas repetitive pronation and supination more often cause attritional changes in the TFCC. Careful physical examination is important to determine the origin of the pain and to try to discover the maneuver or wrist position that most closely reproduces the symptoms.
The radius and ulna must remain congruent through a 190-degree arc.103 Limitation of motion and pain with pronation and supination are consistent with a tear of the supporting ligaments and resultant distal radioulnar joint (DRUJ) instability. If a sufficient portion of the stability has been lost, the ulna appears clinically dislocated or subluxated, and there is severe limitation of forearm rotation. Lateral radiographs of the wrist in neutral and full pronation and supination are not generally specific enough to confirm ulnar subluxation. To evaluate better the congruency of the DRUJ through its range of motion and to assess for subtle subluxations, CT can be performed on both wrists simultaneously in positions of neutral, full pronation, and full supination.104–107
Plain radiographs are most useful in determining ulnar variance and for ruling out fractures or arthritis as a cause of ulnar wrist pain. Because of the variable relationship of the radius and ulna depending on forearm rotation, it is important to take standardized films when measuring ulnar variance.108,109 A posteroanterior view of the wrist with the shoulder abducted to 90 degrees and the elbow flexed to 90 degrees shows the DRUJ in neutral forearm rotation and is easily reproducible (Figure 50-7). Because the ulna lengthens relative to the radius during power grip, a radiograph in the same position during maximal grip best shows impaction of the ulna on the carpus.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree