CHAPTER 6 First contact management
Injury prevention
The causes of sports injuries are many and varied. Items such as technique failure, faulty sports equipment, poor physical fitness, inadequate warm-up and psychological factors can all act as co-factors. Taimela, Kujala and Osterman (1990) divided injury risk factors into intrinsic and extrinsic groups as shown in Table 6.1.
| Extrinsic |
| Intrinsic |
Adapted from Taimela, S., Kujala, U.M. and Osterman, K. (1990) Intrinsic risk factors and athletic injuries. Sports Medicine, 9(4), 205–215. With permission.
Warm-up
The subject of warm-up is dealt with in depth in Chapter 4. A general warm-up, intense enough to induce mild sweating without causing fatigue, is important for injury prevention. The general activity should be followed by a specific warm-up designed to produce a suitable arousal level in the athlete, and to rehearse any complex skills which will be used later in competition.
It is also important that vigorous exercise does not end abruptly, but slows gradually during a cool-down period. This period allows the cardiopulmonary system to return to resting levels without placing undue stress on the body. In addition, delayed onset muscle soreness (DOMS) may be reduced by flushing fresh blood into the muscles previously worked during exercise, and removing waste products. To achieve an increase in muscle perfusion, the activity must involve rhythmic muscle pumping actions of low intensity. The use of post-event massage in this context is described in Chapter 2.
Psychological factors
A variety of psychological factors may predispose an athlete to injury. Personality tests (Cattell 16PF) performed on footballers have shown that tender-minded players were more likely to be injured, and those who were reserved/detached or apprehensive to suffer more severe injuries (Jackson et al., 1978). Anxiety, and the unconscious attempt to cope with it, can cause abnormal behaviour in the athlete (Sanderson, 1981) and may also increase the likelihood of injury. Coping mechanisms for tension or anxiety can in some instances create a distortion of reality. An example is the overly tense athlete who simply denies that he/she is anxious, yet loses composure easily and in some cases actually becomes violent. Individuals of this type may harbour a sense of guilt which they try to reduce by self-punishment. A number of visible characteristics are displayed by the injury-prone athlete (Table 6.2).
Table 6.2 Psychological characteristics of injury-prone athletes
| Counter-phobia |
| Athletes attempt to counter anxiety by being overtly aggressive and fearless. They repeatedly test their indestructibility |
| Sign of masculinity |
| Athlete uses injury as a mark of courage. Needs ‘visible scars of battle’ to show manhood. Continues to play despite injury, but exaggerates pain to seek admiration |
| Masochism |
| Punish themselves for feelings of guilt, often about failure to reach their own unrealistic targets |
| Injury as a weapon |
| Tries to punish others, for example the young athlete who is forced to play by overzealous parents |
| Escape |
| The ‘training room athlete’ who fears competition because of feelings of inferiority, but cannot opt out for fear of isolation |
| Psychosomatic injury |
| No physical injury, or slight injury made worse by emotional factors |
Adapted from Sanderson, F.H. (1981) The psychology of the injury-prone athlete. In Sports Fitness and Sports Injuries (ed. T. Reilly). Faber and Faber, London. With permission.
Stressful events in a player’s life can also be a factor in injury. These can be measured as life change units (Table 6.3), and injured players tend to have significantly more of these in the period preceding injury (Kerr and Minden, 1988). One of the reasons for this increased risk is that the athlete’s attention may be affected, with life events hindering concentration. To perform well, an athlete must ‘let go’ and allow automatic or grooved motor actions to ‘flow’ freely. Stressful life events could lead to worry about performance which may prevent an athlete from letting go. In a study of gymnasts, those who had experienced recent stressful life events were four times more likely to be injured and the severity of injury was 4.5 times greater. The subjects in this study reported ‘lack of concentration’ and ‘thinking of other things’ as the major causes of their injuries (Kerr and Minden, 1988).
Table 6.3 Examples of life change units (LCUs)
| Positive | Negative |
|---|---|
| Marriage | Bereavement |
| Getting a better job | Redundancy |
| Passing an examination | Divorce |
Equipment and environment
Another aspect of ‘environment’ that warrants attention is the other players. Variability of young athletes grouped by chronological age rather than biological (physiological) age may be tremendous. This is especially true at the onset of puberty, where a relatively narrow age range of 2 years in a grouping of 9–11-year-olds will give a large size variation. It was these variations (at the time within the child labour market) which gave rise to the use of physiological age groupings based on pubic hair development (Crampton, 1908).
Table 6.4 shows the difference between age, size and a selection of performance variables in small and large youth ice hockey players in the same league. It is clearly a risk to have a 37 kg athlete able to produce an impact force of just over 1000 N competing against a 74 kg athlete capable of producing an (almost double) impact force of 1700 N.
Table 6.4 Age, size and performance variables of youth ice-hockey players
| Variable | Small (Mean) | Large (Mean) |
|---|---|---|
| Age (years) | 13.4 | 14.0 |
| Weight (kg) | 37.1 | 74.3 |
| Stature (cm) | 147.4 | 178.9 |
| Grip strength (kg) | 27.7 | 56.5 |
| Maximal speed (m/s) | 7.6 | 8.3 |
| Impact force (N) | 1010.0 | 1722.0 |
| Speed at impact (m/s) | 3.2 | 3.7 |
Adapted from Roy, M.A. et al. (1989) Body checking in Pee Wee hockey. Physician and Sportsmedicine, 17(3), 119–126. © The McGraw-Hill Companies.
Self-assessment of maturity can be made using secondary sex characteristics, including external genitalia and pubic hair in males, and breasts, pubic hair and menarche in females (Malina and Beunen, 1996). There is obviously a potential problem of under- and overestimation (by the athlete or others) to remain with peers or to gain a competitive advantage, but the possibility of random testing by medical staff should control this.
Rules
Alteration of rules in sport has been shown to have a positive effect on injury rate and intensity (Table 6.5). Changes in the rules in ice hockey, making the wearing of helmets compulsory, significantly reduced the number of head and eye injuries (Vinger, 1981). In American football, the banning of ‘spear tackles’ (hitting an opponent with the vertex of the head) has reduced the number of head and neck injuries (Torg, Truex and Quedenfield, 1979). In hockey, banning high sticking (lifting the stick above shoulder level) has reduced eye injuries (Tator and Edmonds, 1984); and in karate, banning round-house kicks in competition (a rapid kick aimed at the side of the head) has prevented injury (McLatchie, Davis and Caulley, 1980). Allowing free substitution (permitting injured players to be substituted immediately) in soccer has been shown to reduce injury (Jorgensen, 1989).
Table 6.5 Influence of rules in injury
Adapted from Jorgensen, U. (1989) Free substitution in soccer. Nitz, 3, 155–158.
Screening
Pre-season screening may involve tests of a number of measures (Table 6.6). Tests should be performed 6–8 weeks prior to competition to allow for the effects of training to take place. In addition, pre-event screening should be performed to assess a player’s suitability to compete.
Table 6.6 Examples of measures for pre-season screening
First aid
The unconscious athlete
Concussion
The first international conference on concussion in sport defined sports concussion as ‘a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces’ (Aubrey et al., 2002).
Concussion occurs when the brain is rapidly ‘shaken’, and the condition can be present even though the patient is still conscious. Often, the period of unconsciousness is so brief that it may go unnoticed, and there is only transient memory loss. This is frequently the case with contact injuries where an athlete collides with another and hits his or her head. Clinically concussion may occur from a direct blow to the head or from impulsive force which is transmitted to the head from other regions of the body. There is an impairment of neurological function which is short lived and resolves spontaneously. In sport concussion there is a functional disturbance rather than structural damage and as such neuroimaging is normal (McCrory et al., 2005).
Concussion classification and evaluation
The Glasgow Coma Scale (see below) is traditionally used to assess head injury. However, due to the mild nature of sport concussion this type of scale is no longer considered an appropriate evaluation measure for sport concussion (McCrory et al., 2005). A sport concussion assessment tool (SCAT) was developed at the International Conference on Concussion in Sport, Prague 2004, and updated at the Zurich Conference 2008 (McCrory et al., 2009). Two forms are available, the Pocket SCAT2 (Table 6.7) for general usage and the full SCAT2 for medical and health professionals.
For the full SCAT 2 (http://www.sportalliance.com/Images/Sport%20Safety/SCAT2.pdf) the medical or health professional assesses the patient over eight domains which are colour coded for ease. The scores obtained on these domains are put together to give an overall score, and normative data for this score are developed. The SCAT2 domains are:
The final section of the SCAT2 gives athlete information with recommendations for a graded return to play (see Table 6.8). Concussion injury advice is presented as a cut-off section to be given to the concussed athlete. The SCAT2 documents are available on several websites. The full version is available at http://bjsm.bmj.com/cgi/reprint/43/Suppl_1/i85. The pocket SCAT2 is available at http://www.sarugby.co.za/boksmart/pdf/PocketSCAT2%20final.pdf.
Table 6.8 Graded return to play following sport concussion
Modified from McCroy et al. (2009).
Multiple concussion incidents
The cumulative effects of concussion are important in sports such as boxing, steeplechase and football (Corsellis, 1974; Sortland, Tysvaer and Storli, 1989; McLatchie, 1993). EEG disturbances due to neuronal damage through repeated trauma are seen, especially where a series of EEGs are performed. In addition, neuropsychological performance is impaired, often in the presence of a normal CT scan (McLatchie, Brooks and Galbraith, 1987).
Failure to allow adequate recovery from a concussion incident may result in second impact syndrome (SIS), where a second blow to the head causes further swelling and bleeding. The second blow may be minor and may not appear sufficient to affect the brain. However, the two combined insults cause rapid and profuse swelling. Athletes usually develop respiratory failure and collapse. The mortality rate for this condition is as high as 50% (Cantu, 1998).
Because of the risk of persistent swelling or late bleeding, the return to sport should be delayed following multiple concussion. All athletes sustaining this type of injury should be given a head injury advice card (Table 6.9). Medical examination is essential where there is a failure to remember the event which gave the head injury however minor it may seem. All cases where consciousness has been lost for longer than 3 minutes warrant x-rays of the skull and cervical spine and/or neuroimaging (Buxton and Firth, 1999).
Table 6.9 Care of athletes who have sustained a head injury
Intracerebral lesions
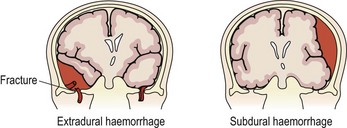
The danger from any head injury is an expanding intracranial lesion resulting from a torn blood vessel, causing epidural (extradural) haemorrhage, subarachnoid haemorrhage or subdural haematoma (Fig. 6.1), so assessment is vital.
These conditions are indicated by an alteration in consciousness (lucid state) and the signs and symptoms shown in Table 6.10. Normally, the intracranial pressure is 4–15 mmHg and an intracranial pressure of 40 mmHg will cause neurological impairment.
Table 6.10 Signs of an expanding intracranial lesion
After Magee (2002).
The Glasgow Coma Scale
The Glasgow Coma Scale (Teasdale and Jennett, 1974) is a series of tests that are given a numerical value which can then be used to objectify an athlete’s state of consciousness (Table 6.11). The scale also forms domain 3 of the SCAT2 evaluation. The first test relates to the eyes, and determines whether the athlete opens the eyes spontaneously or in response to sound (verbal command) or pain. Opening the eyes to verbal command merely means that the person has registered sound; it does not imply that they necessarily understand the command. The second test is of verbal response, and assesses the athlete’s reaction to simple questions such as ‘where are you’ or ‘what is your name’. The test assesses whether the athlete is aware of him/herself and the environment. The third test is of motor response. The maximum score is 6 if the athlete is able to perform actions correctly to verbal commands such as ‘move your arm’. If the athlete fails to respond, a painful stimulus is applied by the practitioner pressing their knuckles into the athlete’s sternum, or pressing the athlete’s fingers together around a pen. Painful stimuli to the face or palm of the hands should be avoided as these can give reflex eye closing and hand closing respectively (Magee, 2002). Where reflex responses alone result, flexion of the arms and hands together with adduction of the upper limb and extension of the lower limb with plantarflexion of the feet (decorticate posturing) indicates a lesion above the red nucleus. Extension of the arms with pronation of the forearm (decerebrate posturing) indicates a lesion of the brainstem. The time of the test should be noted and the test repeated every 15–30 minutes to note any degeneration of results.
Table 6.11 The Glasgow Coma Scale
| Function | Response | Score |
|---|---|---|
| Eye opening | Spontaneous eye opening | 4 |
| Eyes open to command | 3 | |
| Eyes open to pain | 2 | |
| No eye opening | 1 | |
| Verbal response | Coherent appropriate response | 5 |
| Coherent but inappropriate response | 4 | |
| Incoherent speech | 3 | |
| Non-speech noises (moans and groans) | 2 | |
| No vocalization | 1 | |
| Motor response | Obeys commands | 6 |
| Localizing purposeful response to pain | 5 | |
| Non-localizing purposeful withdrawal from pain | 4 | |
| Reflex flexion to pain (arm, decorticate posturing) | 3 | |
| Reflex extension to pain (arm, decerebrate posturing) | 2 | |
| No motor response | 1 | |
| Total score | 46 |
Diabetic coma
If the coma is due to hypoglycaemia, the response to sugar is usually rapid and the danger of secondary symptoms is averted. If hyperglycaemic coma is present, slightly more sugar will not harm the patient (Sperryn, 1985).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree