13
Ear, Nose, Throat, and Mouth
At the completion of this chapter the reader should be able to do the following:
1. Describe the basic anatomy of the ear, nose, mouth, and throat.
2. Perform a basic examination of the ear, nose, mouth, and throat, identifying normal and pathological conditions.
3. Properly use an otoscope to examine the ear and the nose.
4. Recognize common pathological conditions of the ear, nose, mouth, and throat, including signs and symptoms, differential assessment, and when to refer the patient to a physician.
5. Appreciate the common diagnostic tests and standard medical treatment for conditions of the ear, nose, mouth, and throat.
6. Identify the implications for participation in athletics with various conditions of the ear, nose, mouth, and throat.
Overview of Anatomy and Physiology
Ear
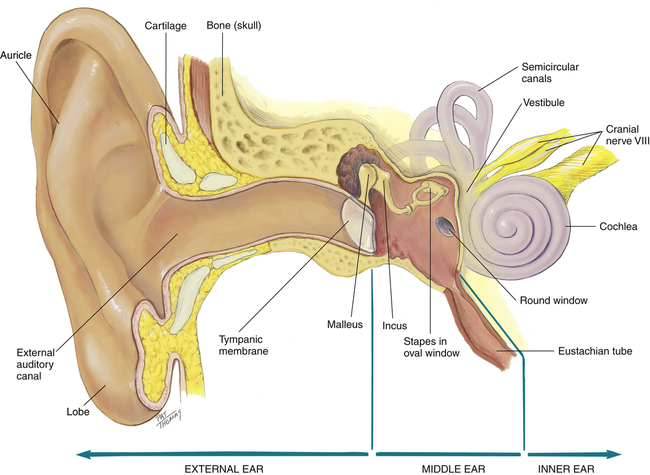
The ear serves two main functions: (1) to identify, locate, and interpret sound and (2) to maintain equilibrium. It consists of three distinct parts: the external, middle, and inner ears (Figure 13-1). The external ear consists of the pinna, or auricle; the external auditory canal; and the lateral surface of the tympanic membrane. The pinna has a cartilage framework that is covered in skin, whereas the ear lobe is fat covered in skin. The shape of the pinna is designed to gather or channel sound into the canal. The approximately 2.5 cm long canal is lined with epithelial cells, hairs, sebaceous glands, and ceruminous glands.1 The ceruminous glands function to produce cerumen, or ear wax, which lubricates the ear canal and tympanic membrane while serving as a protective barrier against foreign matter and bacteria. The outer third of the canal is flexible as it attaches to the pinna but is rigid for the last two thirds as it enters the skull.
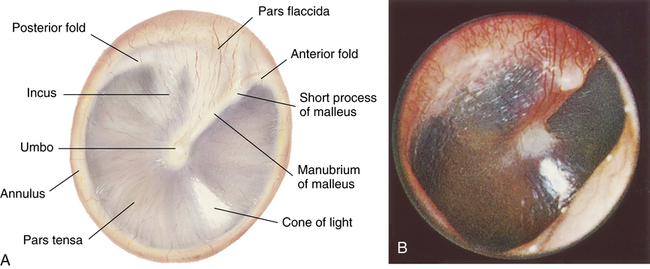
The external ear and the middle ear are separated by the tympanic membrane. The translucent tympanic membrane permits visualization of the middle ear, which is an air-filled cavity in the temporal bone that contains the ossicles: the malleus, incus, and stapes. These bones transmit vibrations from the tympanic membrane mechanically to the inner ear, where the mechanical vibrations are changed to electrical signals. The middle ear is connected to the nasopharynx by the eustachian tube. This passage opens briefly to equalize pressure within the inner ear that occurs with changes in atmospheric pressure caused by swallowing, sneezing, or yawning.2–4
The inner ear consists of the vestibule, semicircular canals, and cochlea. The cochlea encodes the previous mechanical vibrations as electrical impulses that are then sent to the eighth cranial nerve (i.e., vestibulocochlear). The vestibule is directly responsible for balance as the fluid in the semicircular canals shifts with head movement. Feedback from this movement is provided to the brain, assisting to maintain upright posture and balance.2
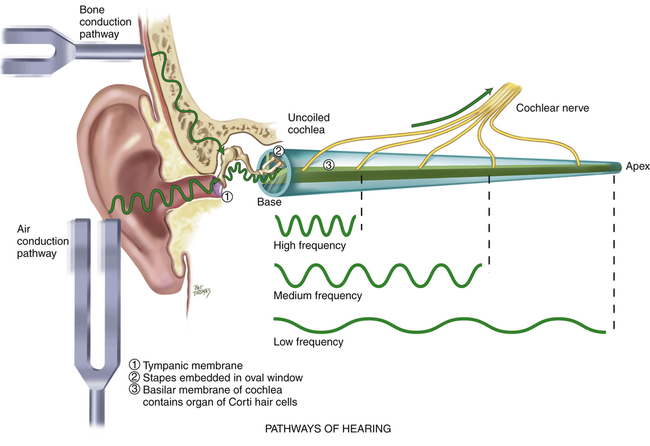
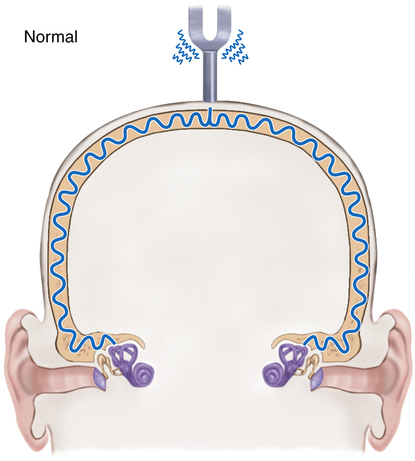
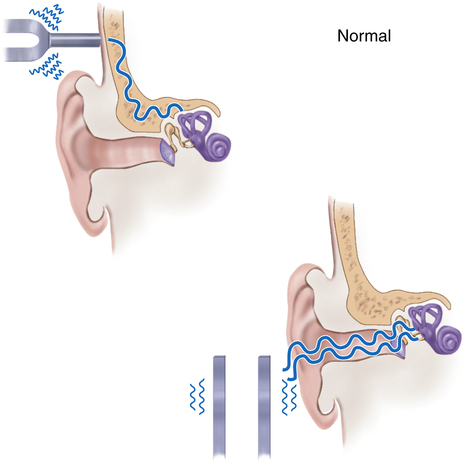
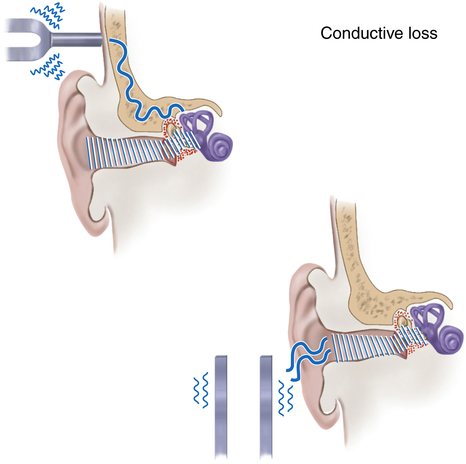
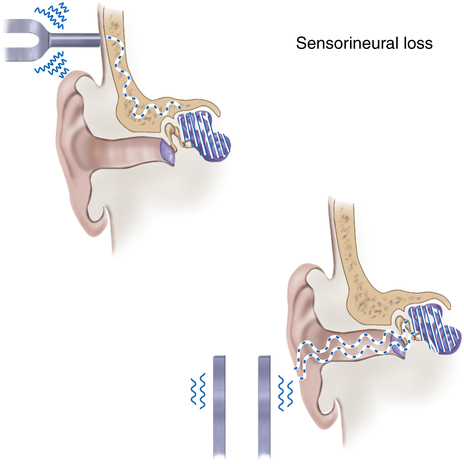
Hearing is an interpretation of sound waves received via an air conduction path. The most efficient and normal hearing pathway is through air conduction; however, bone also conducts sound, by transmitting the vibrations of the skull directly to the vestibulocochlear nerve (Box 13-1).
Nose and Nasopharynx
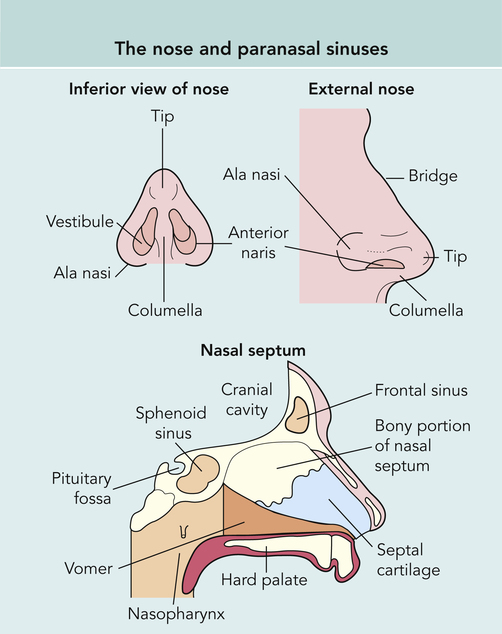
The external nose consists of bone in the proximal third of the nose and cartilage in the lower two thirds covered by skin. The nasal bones arise from extensions of the frontal and maxillary bones, forming the nasal bridge (Figure 13-2). The hard and soft palates form the floor of the nose, and the frontal and sphenoid bones form the roof. The external nose humidifies, filters, and warms inspired air and serves as a passageway for expired air.1,4,5
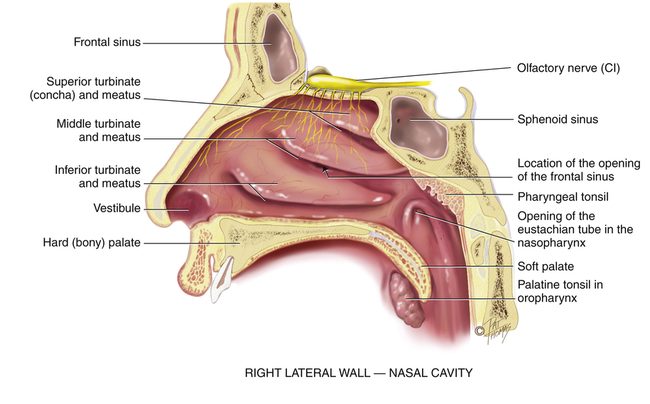
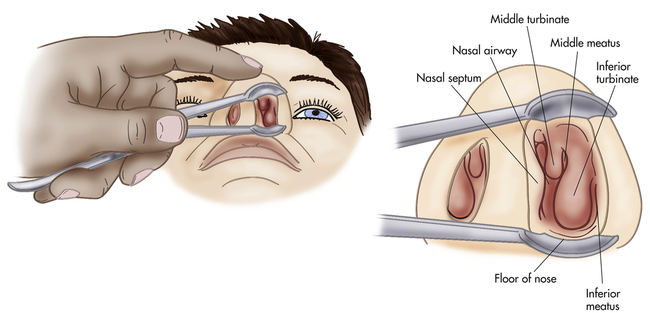
The internal nose is divided into two anterior cavities, or vestibules, by the septum. Air enters the nose through the nostrils and passes posteriorly to the nasopharynx through one of the choanae, separated by one of three turbinate bones. The cribriform plate that is part of the ethmoid bone on the roof of the nose houses the sensory endings of the olfactory nerve (i.e., cranial nerve I). A group of small fragile arteries and veins is located on the anterior superior portion of the septum. This group of arteries and veins is called Kiesselbach’s plexus and is often responsible for epistaxis.6,7 The adenoids lie on the posterior wall of the nasopharynx.
Three turbinate bones form the lateral walls of the nose. Covered by vascular mucous membrane, the turbinates separate the nose into a superior meatus, medial meatus, and inferior meatus (Figure 13-3). The turbinates help to increase the surface area for warming, filtering, and humidifying air.
The paranasal sinuses are air-filled spaces within the cranium.2,3 They are generally named for their location and drain into respective nasal cavities. The sinuses lighten the weight of the skull bones and serve as resonators for sound production. They also produce mucus from the membranes that line the cavities, which drains into the nasal cavity. Because the sinus openings are narrow and occlude easily, they are a common site for inflammation.
Mouth, Oropharynx, and Throat
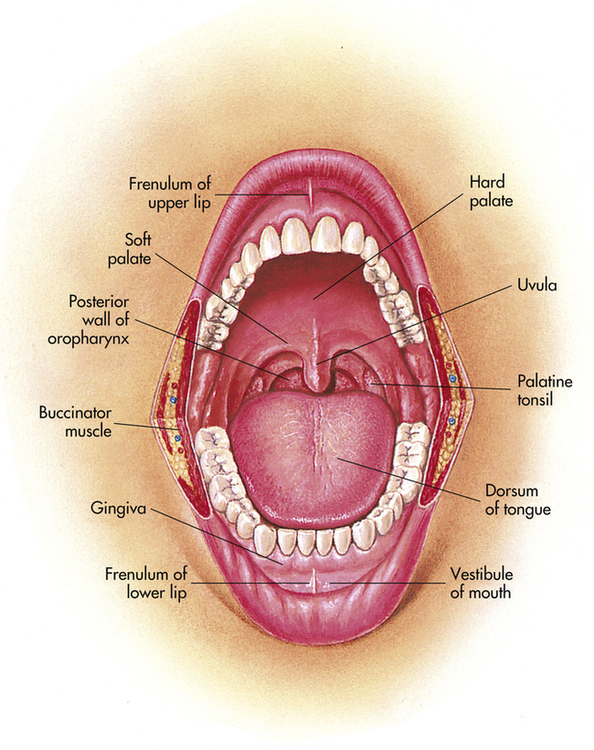
The oral cavity consists of the lips, cheeks, tongue, teeth, and salivary glands (Figure 13-4). It functions in several capacities, including serving as a passage for food as well as the initiation of digestion by mastication and salivary secretion. The mouth and oropharynx also serve to emit air for vocalization and expiration.
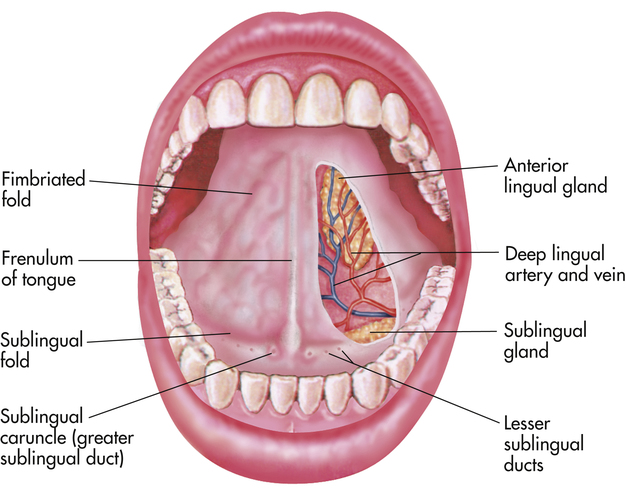
The oral cavity may be divided into the mouth and vestibule. The vestibule is the area between the buccal mucosa and the outer surface of the teeth and gums.1 The roof of the mouth, which is formed by the hard and soft palates, separates the oral cavity from the nasal cavity. The soft palate is muscular tissue covered by mucous membrane that plays an active role in swallowing and vocal resonance. The soft palate, the tonsillar pillars, tonsils, base of the tongue, and posterior pharyngeal walls make up the oropharynx. The tongue is a skeletal muscle covered by mucous membrane, which helps to form the floor of the mouth and is anchored to the floor of the mouth by the frenulum (Figure 13-5).1,4 Papillae cover the surface of the tongue to assist in movement of food. Taste buds are contained within the papillae, and allow people to taste what they are eating.4
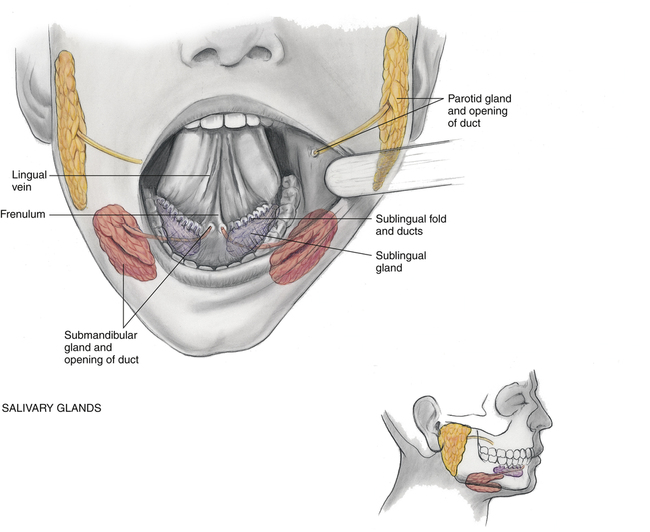
Three pairs of salivary glands are located in the mouth. The parotid, submandibular, and sublingual glands secrete saliva to moisten and lubricate food and to begin the digestion process (Figure 13-6). A parotid gland lies within each cheek, just anterior to the ear, and for each gland a duct, known as Stensen’s duct, extends to an opening on the buccal mucosa opposite the second molar.3 The submandibular glands lie beneath the left and right mandibles at the angle of the jaw. For each a duct runs to the floor of the mouth, with the opening on either side of the frenulum. The sublingual glands are the smallest of the three pairs and are located under the tongue.3,4
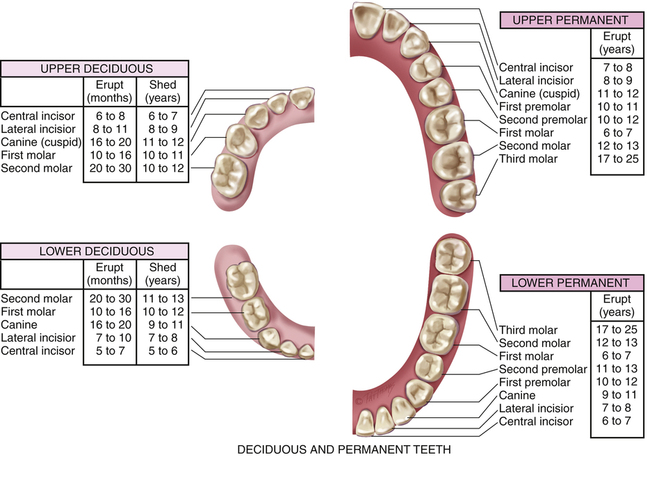
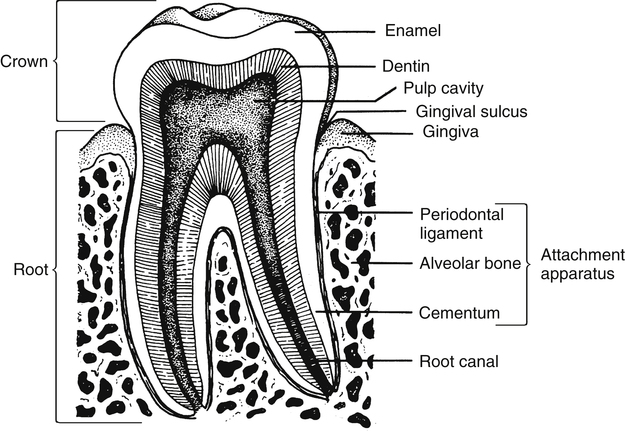
The teeth are embedded in the alveolar ridges and are protected by gingivae that cover the neck and roots of each tooth. Adults typically have 32 permanent teeth that are divided into upper and lower rows (Figure 13-7). Each tooth consists of enamel, dentin, and pulp. The enamel is an extremely hard surface that covers the dentin. The periodontal ligament that surrounds the root of the tooth helps keep the tooth stable. The pulp chamber contains the pulp, nerves, and blood vessels (Figure 13-8).1
The pharynx consists of the combined upper parts of the respiratory and digestive tracts: the nasopharynx, oropharynx, and laryngopharynx (see Figure 7-1).4 The larynx functions in respiration, prevents food and saliva from entering the respiratory tract, and produces sound. It is protected anteriorly by the thyroid cartilage and inferiorly by the cricoid cartilage.
Evaluation of the Ear, Nose, Mouth, and Throat
Examination of the Ear
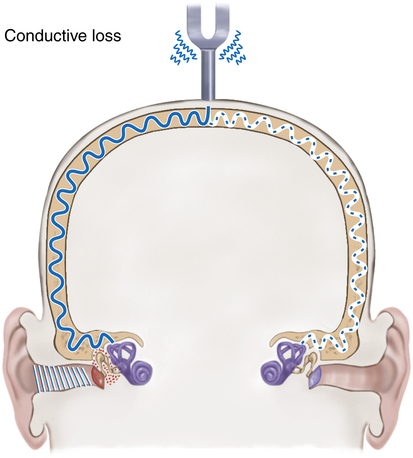
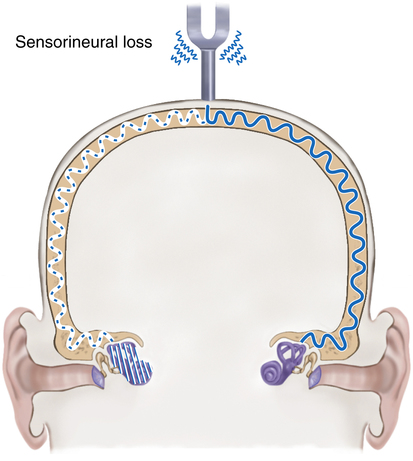
The clinician conducts a gross determination of hearing when it is anticipated that the patient’s ability to hear has been lost. The patient’s response to questions or directions may give a good indication of gross hearing ability. To distinguish between sensorineural and conductive hearing loss, the Weber and Rinne tests may be used (Box 13-2).
An otoscope with a disposal speculum is used to inspect the ear canal. Specula come in different sizes to conform to different-sized ears.5 The largest speculum that can be comfortably fit into the ear is used to allow the best view of the canal and the tympanic membrane. The otoscope is turned on by rotating the dial on top of the handle. The examiner asks the patient to tip the head slightly toward the opposite shoulder and to avoid moving during the examination.
Because the canal slopes inferiorly and forward toward the eye, the external auditory canal must be “straightened” from its S shape by pulling up and back on the pinna. Otitis externa is suspected if the patient experiences pain while the examiner is pulling on the pinna. The speculum is inserted gently and slightly down and forward approximately 0.5 inch into the ear canal. The examiner places a finger or side of the hand against the cheek to guard against inserting the speculum too far into the ear (Figure 13-9).
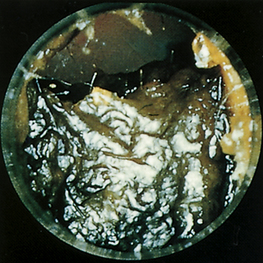
The canal lining is lubricated with cerumen that is secreted by the sebaceous glands in the distal one third of the canal. Cerumen often builds up in the external canal and may impair the patient’s hearing and make examination more difficult (Figure 13-10). The skin in the external auditory canal is examined and should be smooth and somewhat pink or “fleshy” colored. The examiner looks for and notes any scaling or increased redness in the canal as well as any discharge, lesions, or foreign bodies. A reddened canal with discharge signifies inflammation or infection.
To visualize the tympanic membrane the otoscope must be slowly moved in a circular direction as if looking at a large area through a small window. The tympanic membrane appears translucent and “pearly gray” in color. The translucent nature of a healthy tympanic membrane allows visualization of the middle ear cavity including the malleus. The tympanic membrane is concave because it is pulled in at the center, or umbo, by the malleus, allowing a light reflex to be visible when inspected with an otoscope (Figure 13-11). The light reflex occurs as a result of the otoscope’s light beam reflecting off the semitransparent tympanic membrane and can be seen as a wedge-shaped bright spot originating from the umbo. The tympanic membrane should be free from holes or breaks and should not be bulging or bloody. These signs may indicate a tympanic membrane puncture. Redness of and around the tympanic membrane indicates infection in the middle ear, whereas a white color may indicate pus behind the tympanic membrane (Table 13-1). A pneumatic otoscope (which can deliver a small puff of air to the tympanic membrane) may be used to confirm the flexibility of the tympanic membrane. A tympanic membrane that is bulging because of inflammation or infection will not be flaccid but rather is rigid when the puff of air strikes the membrane, and is indicative of otitis media.
TABLE 13-1
Abnormal Findings of the Tympanic Membrane
| Abnormal Finding | Possible Indication |
| Pink or red, bulging | Inflammation of the tympanic membrane |
| Bluish or dark color | Blood behind the tympanic membrane |
| White color | Pus behind the tympanic membrane |
| Perforations or scarring | Current or previous tympanic membrane rupture |
Examination of the Nose and Nasopharynx
Nasal disorders may present with local symptoms or may be a result of disorders from other structures, such as the paranasal sinuses. The major nontraumatic problems related to the nose are nasal obstruction, drainage, facial pain or headache, epistaxis, and change in smell or taste.7 A thorough history of symptoms will help the examiner determine the nature of the nasal disorder.
The examiner asks the patient about the onset and duration of the symptoms. In the case of nasal obstruction, it is important to determine whether trauma was involved or whether the nasal obstruction or congestion onset was insidious. It is also important to determine whether the obstruction is bilateral or unilateral and whether it is constant or intermittent. Assessment of inspiratory and expiratory airflow is done by occluding one nostril at a time while the patient inspires (Figure 13-12).
Unilateral obstruction may indicate an anatomical problem, such as a deviated septum or polyp, whereas bilateral obstruction could arise from a simple cold.7 If drainage is present, it is helpful to determine its characteristics. Is it unilateral or bilateral? Is it clear or discolored? Clear drainage suggests rhinitis, either allergic or nonallergic, whereas yellow, green, or brown drainage suggests bacterial or viral infection (Table 13-2). Straw-colored drainage occurring after a head injury could be cerebrospinal fluid (CSF) and an indicator of possible brain injury. If discharge is present, the examiner should wear gloves for the examination.
TABLE 13-2
Differential Diagnosis of Nasal Conditions With Drainage
| Nasal Drainage: Characterization | Other Symptoms | Most Likely Condition |
| Bilateral watery discharge | Usually associated with sneezing, watery eyes, and congestion | Allergic or nonallergic rhinitis |
| Bilateral purulent discharge | Associated with sinus or upper respiratory infection | Sinusitis (bacterial or viral) |
| Bloody discharge | Traumatic or dry nasal mucosa | Epistaxis |
Modified from Potter PA, Weilitz PB: Mosby’s pocket guide to health assessment, ed 6, St. Louis, 2007, Mosby.
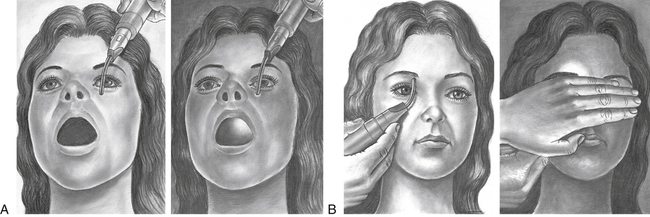
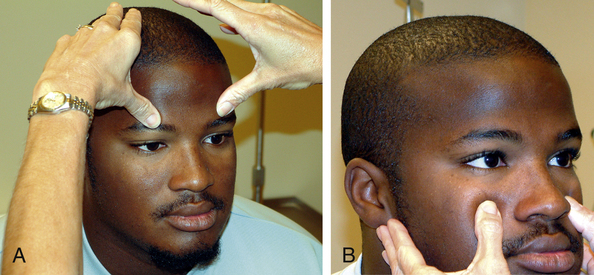
The examiner palpates the facial bones and the sinuses to determine any areas of tenderness, swelling, or deformity. The facial areas over the frontal sinus are palpated by the examiner positioning the thumb up and under the athlete’s eyebrow (Figure 13-13, A). The maxillary sinus is palpated by pressing with thumbs up under the zygomatic process (Figure 13-13, B). Healthy sinuses are not generally tender to the touch, and pain with palpation of the facial bones over the sinuses often indicates inflammation from infection or allergy.
Transillumination
The sinuses also may be transilluminated. This is often performed by the physician; however, the athletic trainer may elect to try the technique. Transillumination is done in a darkened room, using a penlight or an otoscope. The frontal sinus may be transilluminated by placing a light against the medial aspect of each supraorbital rim while looking for a slight red glow of light just above the eyebrow.1,5 An absence of a glow in the sinus indicates that the sinus contains secretions. Likewise, the maxillary sinus may be illuminated by placing the light lateral to the athlete’s nose beneath the medial aspect of the eye while asking the athlete to open the mouth. If the sinus is clear, the hard palate will be illuminated (Figure 13-14).
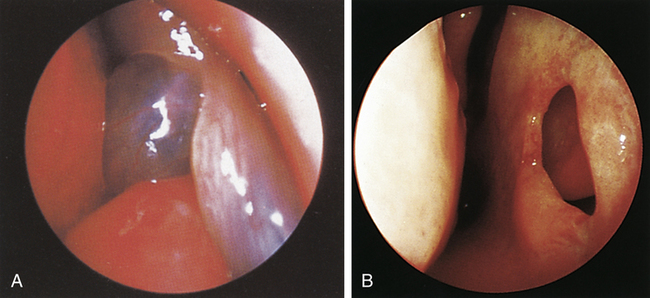
Speculum Examination
The septum may be visualized by tipping the speculum toward the midline (Figure 13-15). The septum is normally pink and glistening and should be thicker anteriorly. The examiner checks for any discoloration, perforations, bleeding, or crusting and notes differences such as polyps (Figure 13-16, A), holes (Figure 13-16, B), swelling, or abnormal coloring.3,5 The septum should be straight and positioned close to the midline. To determine the position of the septum, it is best to compare sides bilaterally, ensuring that the space between the lateral wall of the nose and the septum is the same in both nostrils.
After determining the integrity of the septum, the vestibule and the turbinates can be visualized with the patient’s head fairly erect. The examiner tilts the patient’s head backward to see the middle meatus and middle turbinates. (Figure 13-17)The turbinates should be pink, moist, and free of any lesions or discoloration.
Examination of the Mouth and Throat
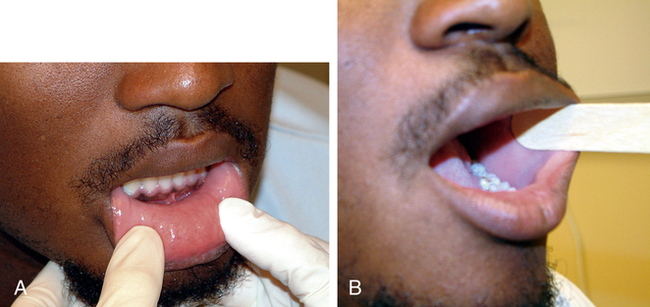
The assessment of the mouth and oropharynx starts with inspection of the face, head, and neck. The face, ears, and neck are observed, noting any asymmetry or changes on the skin. The neck is palpated, with the examiner paying special attention to the hyoid bone, thyroid and cricoid cartilages, and the thyroid gland. Special attention should be paid to the size of the various glands in the face and neck including the parotid glands in the cheeks over the mandible, the submandibular glands that lie beneath the mandible at the “angle” of the jaw, and the thyroid gland. During palpation, the examiner should also note swelling or tenderness of the lymph nodes in the neck and along the jaw. Examination continues with evaluation of the lips with the mouth both open and closed, noting the texture, color, and any surface abnormalities (Figure 13-18, A).
The examiner asks the athlete to open the mouth to visually examine the labial mucosa as well as the maxillary and mandibular vestibules and notes the color and texture as well as any swelling of the mucosa or gingivae. The buccal mucosa is examined, extending from the labial commissure back to the anterior tonsillar pillar. A tongue depressor or gloved finger may be used to pull the buccal mucosa away from the teeth (Figure 13-18, B). The examiner notes pigmentation, color, texture, mobility, and other abnormalities of the mucosa.
the right maxillary posterior gingivae and alveolar ridge and then moving around the arch to the left posterior area.1,5 The inspection continues with the left mandibular posterior gingivae and alveolar ridge and moves around the arch to the right posterior area. The examiner looks for any abnormal lesions, especially white or dark pigmented areas. Stensen’s duct, the opening of the parotid gland, will look like a small dimple opposite the upper second molar.
With the patient’s tongue at rest and mouth partially open, the dorsum of the tongue is inspected for any swelling, ulceration, coating, or variation in size, color, or texture. The examiner visualizes the papillary pattern on the surface of the tongue, asks the athlete to stick out the tongue, and notes any abnormality of mobility or positioning. Then the tip of the tongue is grasped with a piece of gauze to assist in its full protrusion and to aid in examination of the more posterior aspects of the tongue’s lateral borders (Figure 13-19). The ventral surface of the tongue is examined along with the floor of the mouth.

Pathological Conditions of the Ear
Hearing Loss
Hearing loss may include the inability to hear a specific pitch or the inability to detect any sound. It is estimated that 10% to 15% of the population has some degree of hearing impairment.7 The inability to detect any sound is referred to as deafness. The most efficient and normal hearing pathway is through air conduction; however, bone also conducts sound (see Box 13-1). In bone conduction of sound, the vibrations of the skull are transmitted directly to the vestibulocochlear nerve (i.e., cranial nerve VIII).1,3,8
Hearing loss may be divided into conductive hearing loss and sensorineural hearing loss. In conductive hearing loss, the sound conduction pathway is blocked and sound does not pass through the external and middle ear to reach the inner ear, resulting in a loss of hearing. It is considered a mechanical dysfunction because the person is able to hear if the sound is amplified enough. A buildup of impacted wax, injury, foreign body, or infection in the external ear can cause conductive loss. Otitis media, sinus infections, small or blocked eustachian tubes, and allergies can also cause conductive loss.8
Sensorineural loss is more serious and involves the inner ear, where sensory receptors convert sound waves into neural impulses that are transmitted to the brain for translation. Most people who are born deaf have this type of loss. Causes of this type of loss are generally idiopathic. Other identified causes include hereditary factors, meningitis, measles, scarlet fever, mumps, and encephalitis. Hearing loss caused by gradual nerve degeneration, known as presbycusis, often occurs with aging and may cause the person to be unable to understand words. Simple amplification of sound will not increase the ability to hear if sensorineural hearing loss is present.3 Balance problems may also accompany this type of loss. A combination of both conductive and sensorineural hearing loss in the same ear is called a mixed hearing loss. If hearing impairment is suspected, the athlete should be referred as soon as possible for proper diagnosis and treatment. Treatment depends on the cause of the hearing loss.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree