Distal radius and ulnar fractures
INTRODUCTION
Fracture of the distal radius is the most common fracture encountered by orthopaedic trauma surgeons. There are around 120,000 fractures per year in the United Kingdom and 607,000 annually in the United States1,2 with a peak in incidence in the older patient, particularly in females. Recently there has been more interest in the outcome of treatment in the older patient as awareness of the possible impact on the patient’s independence has increased. Although Abraham Colles is famously associated with stating that if a distal radius fracture malunited it would ‘at some remote period again enjoy perfect freedom in all its motions, and be completely exempt from pain’, in the same publication he also stated that if a fracture was allowed to malunite ‘the patient is doomed to endure for many months considerable lameness and stiffness of the limb, accompanied by severe pain on attempting to bend the hand and fingers’. He clearly appreciated the possible impact of a poorly treated fracture on function. Correction of the displacement in a distal radius fracture is aimed at improving the ability of the patient to complete tasks requiring some strength in the hand and wrist which may have little impact on the functional ability of the frail elderly patient. Careful judgement must be employed in making treatment decisions in these cases. This chapter aims to inform the orthopaedic trauma surgeon making treatment decisions in the older patient.
CLASSIFICATION
Before deciding the appropriate management for an elderly patient with a distal radius fracture it is important to understand the range of fracture types which can occur. Many classification systems have been proposed for fractures of the distal radius and ulna over the years, the majority of which are morphological and consider in varying degrees the presence or absence of displacement, comminution and articular involvement. The simplest and probably clinically most used is differentiation between intra- and extra-articular fractures and the presence or absence of comminution. For research purposes the most commonly used is the AO/OTA classification system.
The AO/OTA system (Figure 26.1) is an alphanumeric classification and has 27 different subgroups. Three different types (A, extra-articular; B, partial articular; C, complete articular) are divided into nine main groups and 27 different subtypes depending on comminution and direction of displacement. The system is not used frequently in clinical practice because of its complexity but is commonly used for research purposes.
Although classification systems are widely used for distal radius fractures, their reliability has not been established. At best inter- or intraobserver reliability has been demonstrated for the AO/OTA system3 when only type A, B or C is considered. Undue reliance should not be placed on classification systems especially when considering treatment and prognosis. For research purposes it is preferable to classify distal radius fractures by consensus amongst authors.
EPIDEMIOLOGY
Fracture of the distal radius is the most common fracture encountered by the orthopaedic trauma surgeon. It accounts for around 17.5% of all fractures and recent reports of its annual incidence range from 20.6 to 27 per 100,000/year.4,5,6 and 7 In all studies, the incidence in females is higher than in males by a factor of two to three with a type A age/gender distribution.8
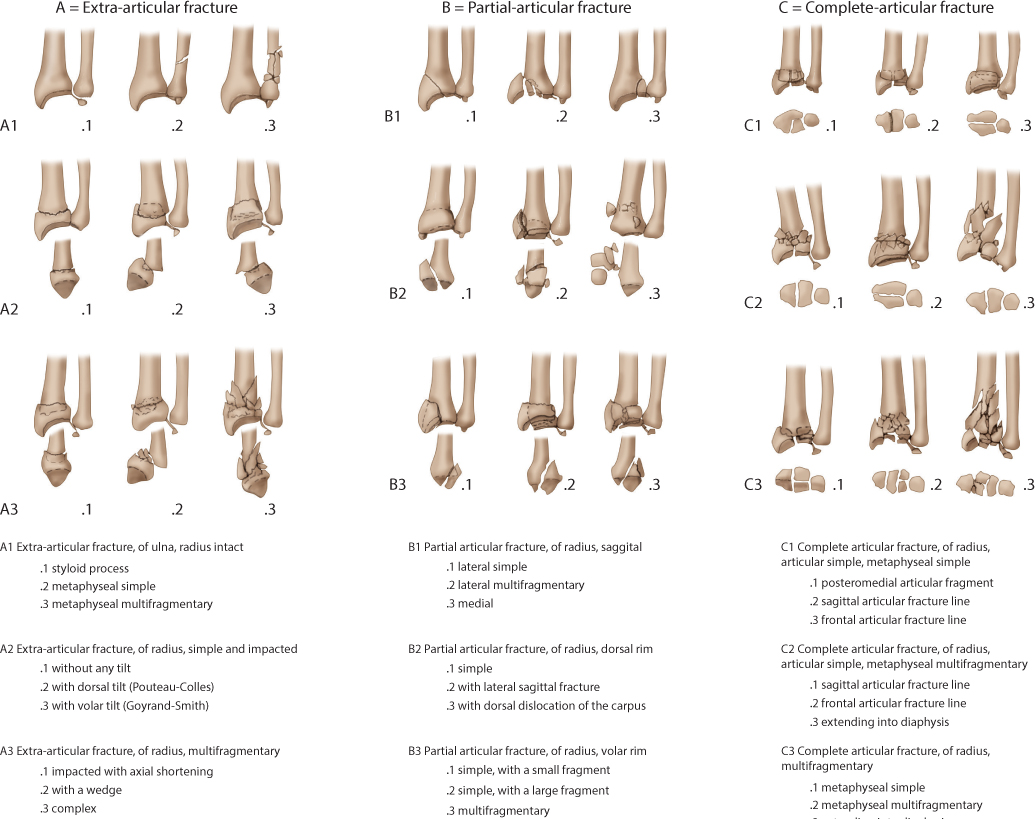
Figure 26.1 The AO/OTA classification of fractures of the distal radius.
There are no publications specifically detailing the epidemiology of distal radius fractures in the elderly. In Edinburgh a study of all distal radius fractures presenting in a 1-year period between July 2007 and June 2008 was undertaken. A total of 1124 fractures were identified, 508 (45%) of which were in patients aged 65 years or over. Of these 508 patients, 441 (86.8%) were female and 67 (13.2%) were male. The median age was 77 years, ranging from 65 years to 98 years. The median age was 78 years for females and 75 years for men. The annual age- and gender-related incidence is shown in Figure 26.2 and demonstrates an increasing incidence for women with age peaking at 125/10,000 of the population in the 85–89-year-old age group. The incidence is much lower for men and shows a modest peak at the same age of 33.7/10,000 of the population.
These figures are consistent with other data.7,9 One of these studies also showed a rising incidence of distal radius fractures in older patients over a 19-year period. Data from Edinburgh show an increase in the incidence of distal radius fractures over a 17-year period, mainly attributable to an increase in incidence in both younger and older men and in women over 75 years of age. It is of interest, however, that the percentage of patients who were independent for the activities of daily living increased significantly over the period, confirming that although getting older, individuals were also getting fitter.5
Of the 508 fractures, 448 (88%) were caused by a fall from standing height, while 28 were caused by higher energy injury, with small numbers of other causes. Extra-articular fractures (OTA/AO type A) accounted for 62%, complete intra-articular fractures (type C) for 23.8% and partial articular fractures (type B) for 14.2% of the total. Overall, 70% of fractures had metaphyseal comminution and 68% were displaced at presentation. Although the vast majority of fractures in older patients occur in lower energy injury, they have a high prevalence of comminuted, displaced fractures. Along with the evidence of increasing incidence in older patients, this suggests that there will be an increasing burden on orthopaedic trauma services in the years to come.
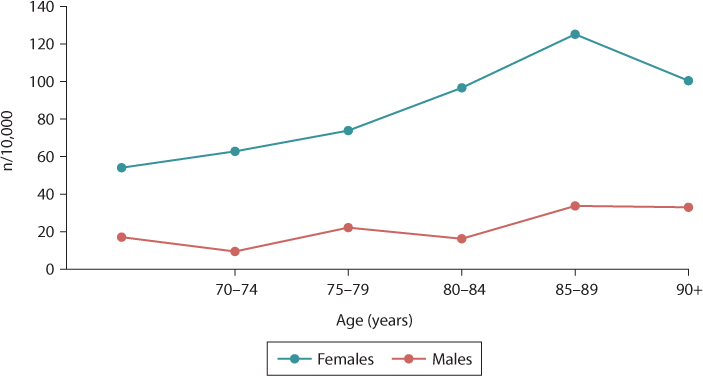
Figure 26.2 The annual age and gender related incidence of distal radius fractures in patients aged 65 years or over.
RISK FACTORS
Reported lifetime risks of distal radius fractures from the age of 50 onwards range from 12% to 52.7% for women10,11 and from 2.4% to 6.2% for men.10,12 The wide range, particularly in women, may be real but could also be a result of differences in the methods of ascertainment of the fractures.
Low bone mineral density (BMD) is an important predictor of future fracture risk but there is also evidence that increasing falls, especially with aging, are a significant risk factor.13,14 The risk of distal radius fracture increases with the higher the level of activity15 implying that individuals who sustain distal radius fractures are in the fitter cohort of older people.
ASSESSMENT
Assessment of a patient with a distal radius fractures is particularly important in the elderly patient as treatment decisions are often complex and have to consider many factors. These include assessment of the clinical and radiological aspects of the fracture and of the patient’s general state of fitness. The latter may require multidisciplinary input from care of the elderly physicians and anaesthetic staff (see Chapters 3 and 4)
Clinical assessment of the fracture
The history of injury is usually straightforward with the patient or carers reporting a fall onto the outstretched hand or occasionally a higher energy injury. Pain and swelling around the wrist are invariable features and where there is displacement a deformity can be seen. Specific questioning should exclude any median or ulnar nerve injury and the presence of pain elsewhere in the arm which may indicate an ipsilateral injury.
Radiological assessment
Posteroanterior (PA), lateral and oblique X-ray views are required and there is usually little doubt about the diagnosis.
PA views allow assessment of:
Radial length/ulnar variance (Figure 26.3b)
Extent of metaphyseal comminution
Ulnar styloid fracture location (tip/waist/base)
Presence, orientation and displacement of articular fractures.
Lateral views allow assessment of:
Dorsal/palmar tilt (Figure 26.3a)
Extent of metaphyseal comminution
Carpal alignment (Figure 26.3c)
Displacement of the volar cortex
Position of the distal radioulnar joint (DRUJ)
Presence, orientation and displacement of articular fractures.
It is important to appreciate that significant discrepancy regarding intra- and interobserver reliability has been demonstrated in the measurement of standard radiographic criteria. For extra-articular fractures the mean standard deviation between surgeons was 3.2 degrees for radial angle, 3.6 degrees for conventional lateral palmar tilt and 2.1 degrees for 15 degrees of lateral palmar tilt.16
Assessment of outcome
Outcome measures for distal radius fracture may use either a combination of objective and subjective factors including pain, range of motion, grip strength, ability to undertake the activities of daily living and radiological measurements or patient related outcome measurements (PROMS). The most frequently used physician based scores for distal radius fractures are the Mayo wrist score,17 the Gartland and Werley score18 and the Green and O’Brien19 score. None have been examined to determine their reliability, responsiveness or validity and although these measurements are theoretically objective the effort applied can be influenced by the patient’s psychological state.20
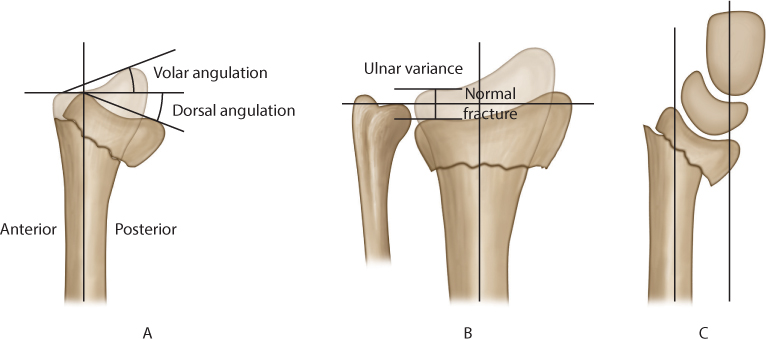
Figure 26.3 (a) A lateral diagram of the distal radius showing measurement of dorsal and volar angulation. (b) A diagrammatic representation of a posteroanterior (PA) view showing measurement of ulnar variance. (c) Assessment of carpal alignment. The perpendicular line down the radius does not intersect within the area of the carpus with a perpendicular line drawn along the long axis of the capitate indicating carpal malalignment.
There have been a number of PROMS developed ranging from generic measures assessing the impact of injury on the patient’s health and well-being (e.g. Short Form 36 [SF36], Sickness Impact Profile [SIP]) to more specific measures of outcome focused on the wrist itself. The latter include the Disability of Arm, Shoulder and Hand (DASH) score which is a 30 item disability/symptom score from zero (no disability) to 100 (severe disability). The normal DASH score is less than 15. The Patient Related Wrist Evaluation (PRWE) is also in frequent use and is specific to the wrist rather than the whole upper extremity.
TREATMENT
The main treatment options for fracture of the distal radius in the elderly are non-operative management, external fixation or internal fixation using either closed reduction (CRIF) or open reduction (ORIF). The decision as to which to use in the elderly is based on the demands which the individual places on their hand and wrist, the mental and physical state of the patient and the type of fracture. To allow an informed decision it is useful to be able to predict the likely outcome of treatment.
Prediction of instability
As many distal radius fractures are treated non-operatively in the elderly it is important to be able to predict the radiological outcome of such treatment. If operative treatment is being considered then a knowledge of the likely radiological outcome will also inform that decision.
Several factors have been associated with redisplacement following closed manipulation of a distal radius fracture.
AGE
Increasing age results in increasing metaphyseal instability of a distal radius fracture. Patients over 80 years of age with a displaced fracture of the distal radius are three times more likely to have instability than those under 30 years of age. This is even more striking in patients with minimally or undisplaced fractures when the risk of instability increases tenfold in older patients.21 It is important to be vigilant for later redisplacement in fractures in elderly patients with osteopenic bones.
INITIAL FRACTURE DISPLACEMENT
The greater the degree of initial displacement (particularly radial shortening), the more energy has been imparted to the fracture resulting in a higher likelihood that closed treatment will be unsuccessful.21
METAPHYSEAL COMMINUTION
The presence of a metaphyseal defect or comminution as evidenced by either plain radiographs or computerized tomography increases the chance of instability.21,22
DISPLACEMENT FOLLOWING CLOSED TREATMENT
Displacement following closed treatment is a predictor of instability as repeat manipulation is unlikely to result in a successful radiographic outcome.23,24
In a study of the natural history of over 3500 distal radius fractures, Mackenney and his co-authors21 reported the independently significant predictors of early instability (redisplacement before 2 weeks), late instability (redisplacement between 2 weeks and fracture union) and malunion for both undisplaced and displaced fractures. Mathematical formulae were constructed to give a percentage chance of redisplacement or malunion for individual patients. The authors gave an example of an independent 85-year-old woman with a dorsally displaced fracture of the distal radius with metaphyseal comminution and a positive ulnar variance of 2 mm. The calculated probability of malunion is 82%. Clinical application of these formulae is likely to allow informed decision-making when considering the appropriate treatment for an elderly patient, encourage early treatment in appropriate cases and reduce the prevalence of malunion.
Prediction of function
The aim of treatment of a distal radius fracture is to restore normal function of the wrist and hand and it is critical that treatment has a realistic chance of achieving that goal. There are many influences on function, including age, psychological state and anatomical position, and it is important to achieve a balance between them to achieve the maximum possible function. With increasing age as demands upon the wrist become less, the symptoms from a malunion are likely to reduce and the importance of normal anatomy declines.
There is as yet no consensus on how patients should be treated as the definition of an elderly patient is not clear. Physiological and actual age may vary greatly but the surgeon usually makes a judgement on a subjective impression. The use of more objective measures available in the geriatric and epidemiological literature such as the Physical Activity Scale of the Elderly (PASE) score may be of value.
Lessening demands may account for reports of malunion of the distal radius in older people being compatible with good function. In 74 older patients with distal radius fractures treated non-operatively, 71% had at least one unacceptable radiographic deformity but at review 6 months after fracture the authors reported that self-reported disability was low and patient satisfaction high despite a mean DASH score of 24 and a patient dissatisfaction rate of 28%. Mean DASH scores were higher if the radiological deformity was outside the acceptable range but this was not statistically significant.25 In another study, 25 low demand patients over 60 years of age were treated non-operatively. Overall, 32% of patients had fair or poor radiographic results but only 12% had fair or poor functional outcomes. The authors concluded that non-operative treatment yields satisfactory results in low demand patients.26 No relationship between anatomy and function was found in a group of 74 older patients with conservatively managed distal radius fractures 6 months after injury although only 59% of patients were satisfied with the outcome.27 Grewal and MacDermid found that the relative risk of a poor outcome with malalignment of the distal radius showed a decreasing trend with increasing age.28 Functional outcome in malunited fractures in the super-elderly (defined as those aged 80 years or over) was compared with a similar group without malunion. No differences in functional outcome were found, even in those living independently.29
In contrast to these studies, Brogren and her co-authors30 examined 143 patients 1 year after distal radius fracture and classified them into three groups: no malunion, single malunion (either dorsal tilt of 10 degrees or positive ulnar variance) and combined malunion (both dorsal tilt of 10 degrees and positive ulnar variance). The average age was 65 years, younger than that in some of the previously quoted studies. With regression analysis the relative risk of higher disability was 2.5 with single malunion and 3.7 with a combined malunion. There was no difference in these results when adjusted for age or gender. The authors concluded that malunion with a dorsal angle greater than 10 degrees or a positive ulnar variance leads to higher arm related disability after distal radius fracture, regardless of age or gender.
The individual measures of anatomical reduction have also been examined in an attempt to clarify which are important in restoring function. Correction of ulnar variance appears to be important in restoration of grip strength and DRUJ function.23,30,31 Loss of the normal palmar tilt may also have a deleterious effect on function causing worsening incongruence of the DRUJ, increased tightness of the interosseous membrane and limited rotation. In addition, loss of the normal palmar tilt positions the carpus in a dorsal collapse alignment. A number of studies have implicated residual dorsal tilt in poorer grip strength and DRUJ function.30,32 Resultant carpal malalignment (Figure 26.4) has been implicated as the strongest negative influence on function and prognosis.23,33,34
Articular damage may be influenced by the initial insult to the articular cartilage and the effects of residual incongruity and its end result is degenerative change. The relationship between the three and their influence on function remains uncertain, especially in the older patient. This is illustrated by the difficulty in demonstrating consistent relationships between articular incongruity, osteoarthrosis and significant functional compromise. In 1986 Knirk and Jupiter correlated patient outcome with residual intra-articular incongruity. They found a 91% prevalence of radiographically apparent arthrosis with any measurable intra-articular step-off and a 100% prevalence with over 2 mm of articular step-off. However, only one patient with bilateral fractures had to stop working as a direct result of the injuries and 61% reported an excellent or good outcome.35 Long-term reviews of younger patients have failed to show a significant relationship between radiological degenerative change and functional outcome36 so it is unlikely that residual articular malalignment will have a significant impact on function for the older patient.

Figure 26.4 A lateral view of a distal radius fracture. Perpendicular lines down the long axes of the radius and the capitate do not intersect within the area of the carpus. The carpus is therefore malaligned.
In treatment of the elderly patient where biological and chronological age may vary significantly, it is difficult to know whether age, level of comorbidity and pre-injury function or a combination of those is the most important factor in deciding whether there will be benefit in correcting the anatomical position. At present we cannot predict the outcome of a distal radius fracture with any degree of confidence but can only recommend levels of displacement which can be accepted in the fit, active and fully functioning patient regardless of age (Table 26.1). These should not be applied to the frail elderly patient when it may be preferable to accept a malunion. These levels are more stringent than those recommended by the American Academy of Orthopedic Surgeons (AAOS) as the AAOS publication does not consider the effect of carpal malalignment. If the carpus is malaligned and the dorsal tilt is beyond neutral then correction should be undertaken. Some dorsal tilt can be accepted if the carpus is aligned.37 Palmar tilt can be accepted provided the carpus is aligned.
Non-operative treatment
Non-operative treatment remains the most common treatment method for fractures of the distal radius and consists of plaster or splint management with or without closed reduction. Rates of non-operative treatment are probably around 70%38 in the UK and vary from 60% to 96% with geographic location in the United States.1,39 Rates of non-operative treatment have been shown to increase with increasing age and comorbidities.39,40 Non-operative treatment is also less likely to be employed by hand surgeons compared to orthopaedic trauma surgeons.1,40
Trends in the use of non-operative treatment of distal radius fractures have changed over the years. In the 1950s just over 95% of distal radius fractures were treated non-operatively in the United States41 in comparison to as few as 60% in some areas of the United States in this millennium.39 Recent evidence shows an increase from 3% to 16% in the use of ORIF and an accompanying decrease from 82% to 70% in non-operative management in the elderly since 2000,1 a change attributed to the introduction of locking plates despite a lack of evidence showing clear benefit.
INDICATIONS FOR NON-OPERATIVE TREATMENT
Non-operative treatment is indicated for undisplaced stable fractures or displaced fractures which are stable after reduction. Stability after reduction may be assessed by observation over time or by predictive algorithms.21
Manipulative reduction is indicated where the radiological position falls outside acceptable limits (Table 26.1) and non-operative treatment is predicted to be successful, that is, if the fracture is likely to be stable. It is also used when there is an impending complication which may be averted by early reduction even if further treatment may be necessary. In some situations manipulative treatment is not necessary. These include fracture with a high risk of instability where more definitive primary treatment should be used. Manipulative reduction should not be used where the fracture is displaced and unstable but the patient is not considered suitable for surgical treatment, for example in a low demand or very elderly patient. In a series of 59 low demand patient who had undergone manipulative reduction and who had a mean age of 82 years, 53 patients ultimately had a malunion. The authors concluded that primary reduction was ineffective in elderly frail patients and recommend that it should only be performed where there is a specific indication such as median nerve symptoms.42
TECHNIQUE OF MANIPULATIVE REDUCTION
Reduction of a displaced distal radius fracture requires adequate analgesia or pain relief, which can be achieved by haematoma block, regional or general anaesthesia or intravenous sedation although the latter two should be avoided if possible in the elderly. In a number of comparative studies there is a consensus that Bier’s block is a safe, effective and practical procedure and superior to haematoma block.43,44
Table 26.1 The radiological limits beyond which reduction is advised
Radiological measurement | Recommended limits |
Positive ulnar variance (mm) | 2–3 |
Carpal malalignment | None |
Dorsal tilt | Neutral if carpus malaligned <10° if carpus aligned |
Palmar tilt | No limit if carpus aligned |
Gap or step in joint (mm) | 2 |
Reduction of distal radius fractures is usually straightforward, with longitudinal traction disengaging the fracture and direct pressure or wrist flexion restoring volar tilt. Care must be taken in the elderly as excessive traction may produce shearing of the skin. Excessive wrist flexion, the Cotton-Loder position, should be avoided as it increases carpal tunnel pressures and therefore the risk of acute carpal tunnel syndrome (CTS).
CAST IMMOBILIZATION
Once the reduction manoeuvres have been performed, a plaster cast is applied. There are a number of controversies around the use of plaster casts including the type of cast, the use of bracing, the position of immobilization and the length of time required in cast.
Type of cast
The initial cast is usually a back slab or sugar tong splint which is completed when swelling has reduced. It is important to allow free finger movement within a cast by ensuring that the cast ends proximal to the metacarpophalangeal joints.
Although it has been suggested that holding the forearm in supination prevents redisplacement from the deforming force of brachioradialis, randomized studies have shown no benefit of above elbow immobilization compared to forearm casts in maintaining the fracture reduction45,46 with some showing a disadvantage because of long-term rotational contracture with above elbow casts.47 No advantage has been demonstrated by the use of braces rather than casts.
Position of immobilization
Extreme positions of the wrist should be avoided. Slight flexion and ulnar deviation is commonly used but neutral or even dorsiflexed positions do not seem to affect the final radiological position. It is likely that fracture and patient factors rather than the wrist position determine the stability of a distal radius fracture.21
Length of time in cast
Undisplaced fractures need a very limited or no immobilization time with some evidence that functional recovery is faster than when conventional cast immobilization is used.48 If immobilization is used, removable wrist splints may be more acceptable to the older patient than a cast. In displaced fractures, which have required manipulative reduction, the accepted length of time in a cast is 5–6 weeks. However in a randomized controlled trial (RCT), no significant anatomical differences but less pain was reported in patients over 60 years of age whose casts were retained for 3 rather than 5 weeks.49
Radiological and clinical review following fracture reduction should be undertaken at regular intervals. All fractures should be reviewed at 1 week as even minimally displaced fractures which have not required initial reduction may displace (Figure 26.5). Instability more than 2 weeks after reduction has been reported in almost half of cases21 indicating that fracture review should also be undertaken at 2 and 3 weeks after injury.
OUTCOME OF NON-OPERATIVE MANAGEMENT
The majority of reports of outcomes after non-operative treatment are in cohorts of older patients. In a review of the outcome of non-operative management in 66 patients, Foldhazy and his co-authors reported a high rate of radiological deformity with a mean dorsal angle of 13 degrees in patients less than 60 years of age and 18 degrees in the older patients at 9–13 years after injury. Overall, 52 cases were rated as excellent or good according to the modified Green and O’Brien score. The authors noted a slower recovery in older patients and concluded that some patients with non-operatively treated distal radius fractures still experience some impairment a decade after injury.50 In other reports concentrating on older patients significant numbers of malunited fractures are found.25,26 and 27,51 Function does not return to normal with mean DASH scores of 15.7 to 2425,51,52 and patient satisfaction ranging from 59% to 92%.25,27,51
Operative treatment
The decision to treat the elderly patient with surgery is a complex one and should be based primarily on the functional ability of the patient pre-injury and the requirements after surgery. The main effect of correcting the anatomical position of the distal radius is to restore the ability to perform the activities of daily living which require strength and endurance. It therefore follows that if the individual no longer requires to perform these activities then surgery will not improve their quality of life. The discussion on operative treatment in this chapter assumes that the patient is active and performing these activities.
There are a number of methods of operative treatment available for distal radius fractures including closed reduction and percutaneous pinning, ORIF, different types of external fixation or combinations of each type of treatment. Once the decision is made that a patient is a suitable candidate for surgery the choice of the treatment type should be guided by the fracture type and the relative outcomes of the treatment methods.
Around 60% of distal radius fractures are extra-articular and almost one-half are likely to have metaphyseal instability. One-third are articular fractures but fewer than 5% are complex articular fractures. A small proportion are volar displaced fractures including volar shearing fractures. For the purposes of making decisions about surgical treatment, four groups should be considered: metaphyseal unstable, extra or minimal articular fractures, displaced articular fractures and volar displaced fractures.
METAPHYSEAL UNSTABLE, EXTRA OR MINIMAL ARTICULAR FRACTURES
These are the most common fractures requiring surgical treatment in the older patient. Metaphyseal instability may be predicted or actual. A minimal articular fracture is one which has an articular component and which does not require articular reduction (Figure 26.6). In active older patients with these fractures, reduction and stabilization is indicated to maximize the chance of good recovery. Metaphyseal unstable fractures can be stabilized by closed reduction and percutaneous pinning, ORIF or external fixation. Closed re-manipulation and plaster management was popular a number of years ago but has been shown to be ineffective by a number of authors.23,24,53 This practice should be abandoned in favour of more stable fixation techniques.

Figure 26.5 (a) An anteroposterior (AP) view and (b) a lateral view of a minimally displaced distal radius fracture in a fit 72-year-old woman. There is loss of the normal volar tilt but no dorsal angulation and the carpus is aligned. (c,d) The fracture was treated in a cast without manipulation. At 1 week after injury the fracture has collapsed into dorsal angulation with a malaligned carpus. (e,f) The fracture has been rereduced and held with a non-bridging external fixator.
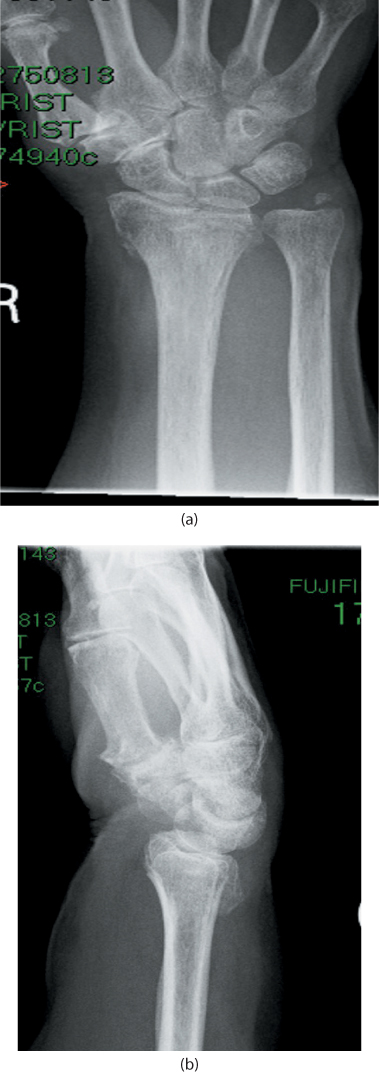
Figure 26.6 A metaphyseal displaced fracture with an undisplaced vertical fracture extending into the radiocarpal joint. During treatment this fracture will behave as an extra-articular fracture.
Percutaneous pinning
Percutaneous pinning of fractures of the distal radius is an appealing technique as it is minimally invasive. It has been widely used for the treatment of unstable extra-articular or minimal articular distal radius fractures as well as for intra-articular fractures.
There are three basic constructs for percutaneous pinning:
Distal radius pinning where pins are placed across the fracture in the distal radius. These may be only radial styloid pins or may also include a pin from the dorsal ulnar aspect to the volar aspect of the radius.
Ulnar radial pinning where the pins are placed from the radius across the ulna.
Intra-focal pinning or the Kapandji technique where the pins are inserted into the fracture, used as reduction tools and then driven into the proximal radius (Figure 26.7).
Whichever technique is used it is important to avoid damage to the dorsal sensory branch of the radial nerve or tendons which are close to the insertion points of both radial styloid and dorsal ulnar wires by using open pin placement techniques. Pins may be left protruding from the skin for ease of removal but a small RCT demonstrated lower pin track infection rates in wires buried below the skin.54 This has the disadvantage of requiring a further minor procedure to remove the wires. Most authors recommend a short arm cast for up to 6 weeks after percutaneous pinning. An RCT of 60 patients compared 1 and 6 weeks in a cast after percutaneous pinning and found no differences between the groups. However only 24 patients had metaphyseal comminution so the likelihood is that the majority were stable fractures.55
Despite a number of comparative studies, no differences between the different types of percutaneous pinning have been demonstrated although the results are difficult to interpret as many of the fractures had no comminution and are therefore unlikely to have been unstable.56,57
Complications of percutaneous pinning
The most common complication of percutaneous pinning is damage to the superficial branch of the radial nerve which occurs in up to 15% of cases55,56 and may occur after pin removal.55,56 Placement of the pins should be done under direct visualization using small skin incisions and blunt dissection down to bone. Care should be taken when removing buried pins that the incisions are large enough to ensure protection of the nerve.
Pin track infection is a frequently ignored complication of percutaneous pinning and is often poorly defined. It is important to differentiate between minor and major pin track infections. Major pin track infection occurs when further surgery is required to eradicate the problem or the pins have to be removed early. The majority of pin track infections are minor after percutaneous pinning with rates recorded from 1.7% to 70%.54,55 and 56,58,59 Major pin track infection occurs rarely with most authors reporting none. Burial of pins subcutaneously may contribute to avoidance of pin track infection, especially if the pins are in place for prolonged periods.54
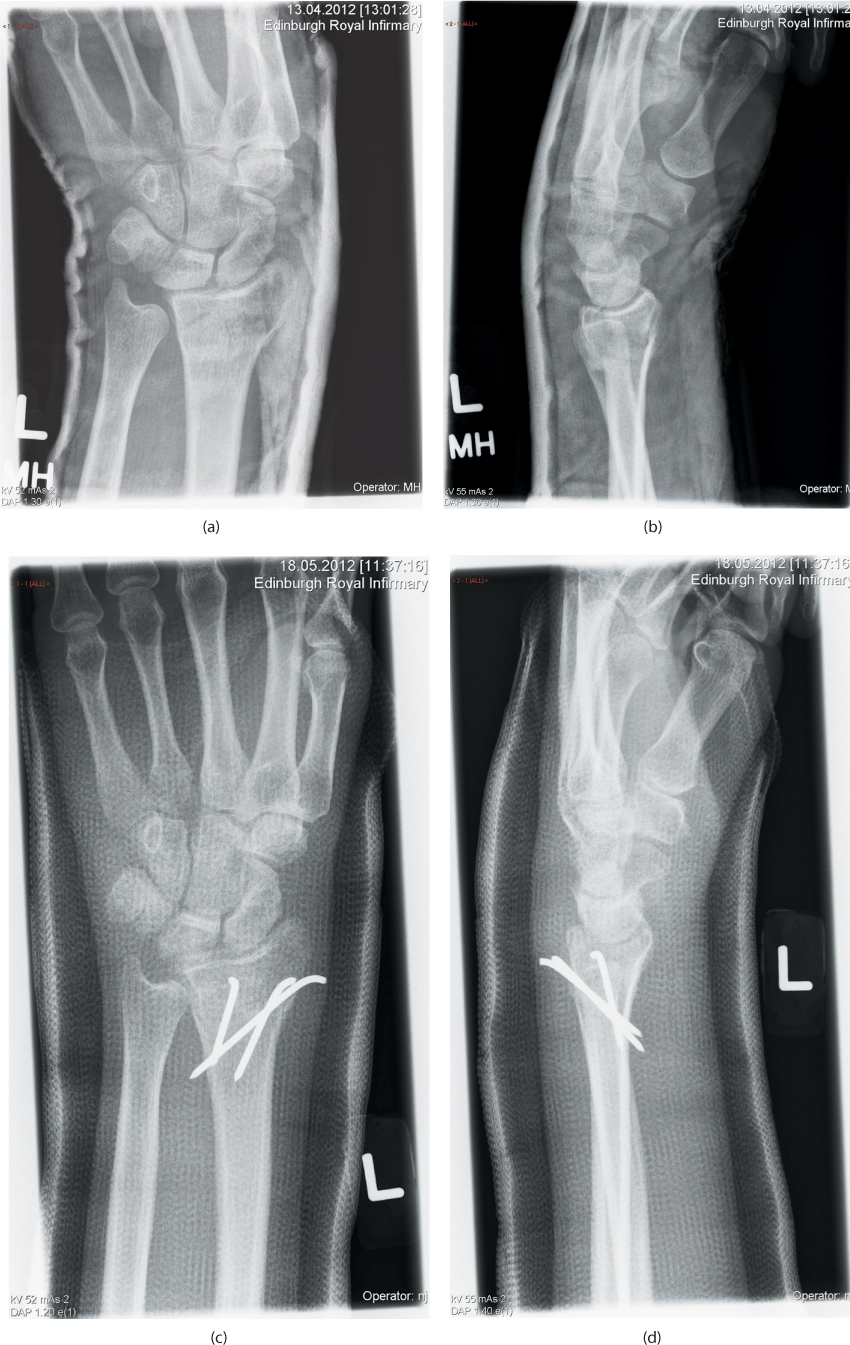
Figure 26.7 An unstable fracture of the distal radius treated with three pins inserted through the fracture site using the Kapandji technique.
External fixation
There are two different methods of external fixation: bridging or spanning fixation and non-bridging or non-spanning fixation. For bridging external fixation pins are placed in the second metacarpal and the radial shaft thus bridging the radiocarpal, intercarpal and carpometacarpal joints (Figure 26.8). This technique depends on ligamentotaxis and may be static, dynamic (allowing some wrist movement) or augmented (with internal fixation, bone graft or bone substitute or a fifth pin in the distal fragment). For non-bridging external fixation pins are placed in the distal fragment of the fracture and in the radial shaft allowing direct fixation of the fracture without immobilizing any joints (Figure 26.9).
Bridging external fixation
The most common indication for bridging external fixation is actual or predicted instability in the dorsally displaced extra-articular or minimal articular fracture of the distal radius, especially where the distal fragment is too small to accommodate pins for non-bridging fractures and open injuries.
Two pins are inserted in the second metacarpal by hand after predrilling at about 45 degrees to the frontal plane. Pins should be placed through open incisions and engage both cortices. The proximal pins are placed in the mid lateral position in the radial diaphysis in the plane between the brachioradialis muscle and superficial radial nerve and the extensor carpi radialis tendons. The pins are then connected by a bar and clamps. The fracture is reduced with the fixator in position and the clamps are then tightened. Care must be taken not to over-distract the wrist as this may increase the load required to generate metacarpophalangeal joint flexion and result in hand stiffness. Release of pin tracks may be required at the end of the procedure to eliminate tension on the skin which may lead to pin track infection. Physiotherapy may be required if hand stiffness develops. The fixator can usually be removed at 5–6 weeks after application. Anaesthesia is not required for removal.
Non-bridging external fixation
Indications for non-bridging external fixation are similar to those for bridging external fixation but there must be sufficient space (1 cm of intact volar cortex) in the distal fragment to site the pins. The technique can also be used for displaced articular fractures if there is sufficient space for pins once the joint surface has been reduced and fixed. Non-bridging external fixation can also be used for distal radial osteotomy for dorsal malunion.
Two distal pins are placed from dorsal to volar, although some fixators use radial sided pins. Fluoroscopy is essential. The pins are placed midway between the fracture and the radiocarpal joint, parallel to the joint surface on the lateral view (Figure 26.9) and on either side of Lister’s tubercle and the extensor pollicis longus (EPL) tendon and should penetrate the volar cortex. Open pin placement and careful retraction will protect the extensor tendons. The forearm is then rotated to confirm free rotation and images are obtained to exclude penetration of the distal radioulnar or radiocarpal joint. Two proximal pins are then placed in the radius proximal to the fracture in a similar fashion to that used for bridging external fixation except that their position is usually more dorsal to volar than mid-lateral. The fracture is reduced by using the distal pins as a ‘joystick’ to control the position of the distal fragment (Figure 26.9b). Care should be taken to avoid over-reduction where there is volar comminution. As the distal pins move with the reduction, they should move into the centre of correctly placed skin incisions but each pin track should be released if there is any residual tension.
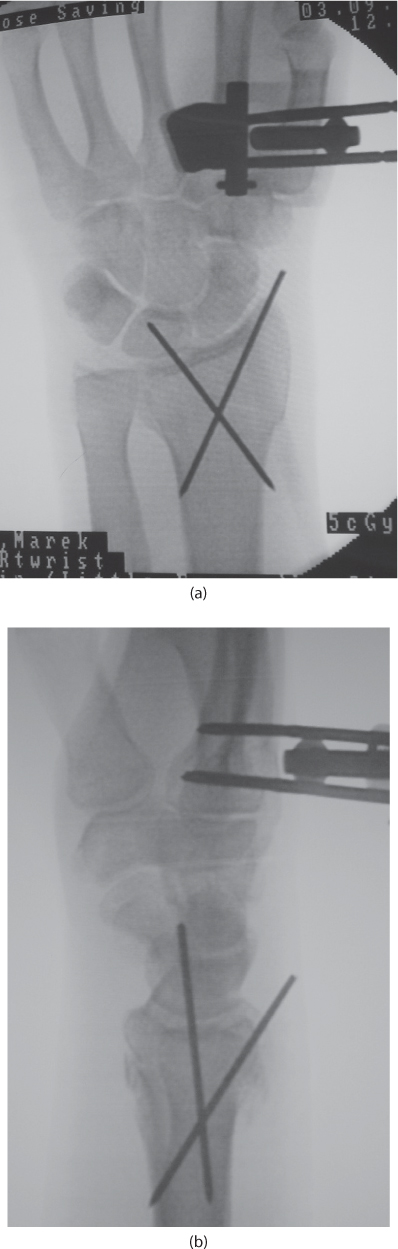
Figure 26.8 An unstable distal radius fracture treated with bridging external fixation. The fixation has been augmented with percutaneous pins. PA (a) and lateral (b) views of and unstable distal radius fracture treated with bridging external fixation. The fixation has been augmented with percutaneous pins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








