99 Clinical Features of Osteoarthritis
Osteoarthritis can be defined radiographically, clinically, or symptomatically.
Pain and functional limitations contribute substantially to disability in osteoarthritis.
Mortality is increased among individuals with osteoarthritis compared with the general population.
Osteoarthritis (OA), the most common form of arthritis, is found worldwide and is strongly associated with aging. It affected 27 million adults in the United States in 2005.1 OA of the knee and hip has significant functional impact due to effects on ambulation and mobility and is associated with considerable medical costs, accounting for 97% of the 455,000 total knee replacements and 83% of the 233,000 total hip replacements for arthritis in 2004.2 Given the aging of our society and the obesity epidemic, the burden of OA can only be expected to increase over the next 20 years.3
OA affects all of the structures in and around a joint and should be considered a failure of the total joint. Historically, the emphasis in OA research has been on cartilage degeneration, but more recent work has expanded this view to an improved understanding of the role of subchondral bone, synovium, ligaments/tendons, meniscus, muscle, and nerve tissues in the disease process.4,5 The late- or end-stage joint, clinically recognizable as OA, likely represents a final common pathway of many different factors including genetics, environment, and biomechanical contributors.
Epidemiology of Osteoarthritis
OA can be defined pathologically, radiographically, or clinically. The American College of Rheumatology (ACR) criteria for the classification of OA of the hand, hip, and knee are shown in Table 99-1.6–8 For the hand, only clinical criteria are used, with a sensitivity of 92% and specificity of 98%. For the hip, the sensitivity and specificity of the ACR criteria are estimated to be 91% and 89%, whereas for the knee they are 91% and 86%, respectively. Due to their high specificity, these criteria are most useful for differentiating OA from inflammatory arthropathy, but less so for differentiating early OA from healthy controls. Compared with radiographic definitions, the ACR criteria tend to underestimate prevalence of OA.9,10
Table 99-1 American College of Rheumatology Radiologic and Clinical Criteria for Osteoarthritis
| Hand8 |
1. Hand pain, aching, or stiffness on most days of prior mo 2. Hard tissue enlargement of ≥2 of 10 selected joints* 3. Fewer than 3 swollen MCP joints 4. Hard tissue enlargement of ≥2 DIP joints 5. Deformity of ≥2 of 10 selected joints* Diagnosis requires items 1-3 and either 4 or 5 *10 selected joints: DIP 2-3, PIP 2-3, and CMC 1 bilaterally |
| Knee: Clinical6 |
| Knee: Clinical and Radiographic |
| Hip: Clinical and Radiographic7 |
CMC, carpometacarpal; DIP, distal interphalangeal; ESR, erythrocyte sedimentation rate; MCP, metacarpophalangeal; PIP, proximal interphalangeal.
From Altman R, Asch E, Bloch D, et al: Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association, Arthritis Rheum 29(8):1039–1049, 1986; Altman R, Alarcon G, Appelrouth D, et al: The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip, Arthritis Rheum 34(5):505–514, 1991; and Altman R, Alarcon G, Appelrouth D, et al: The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand, Arthritis Rheum 33(11):1601–1610, 1990.
The presence of radiographic OA usually requires the presence of a definite osteophyte or joint space narrowing on plain radiographs, although magnetic resonance imaging (MRI)-based definitions are under development.11 Clinical OA is usually defined by abnormalities on physical examination consistent with OA such as nodal changes in the hands, limited and painful internal rotation of the hip, or crepitus with knee movement. Symptomatic OA is usually defined as pain, aching, or stiffness in a joint with radiographic OA. Definitions can vary according to joint site, frequency or intensity of symptoms, and time span over which symptoms are assessed.
Prevalence of Radiographic Osteoarthritis
Because of the multiple different definitions of OA, prevalence estimates vary. The first National Health and Nutrition Examination Survey (NHANES I) found that 12% of the U.S. population had clinically defined OA in at least one joint. A few population-based studies have estimated the prevalence of radiographic OA at the knee, recently reviewed by Lawrence and colleagues.1 Despite variations based on radiographic technique and participant age, these studies estimate that radiographic knee OA is present in 14% to 37% of U.S. adults and is more frequent in women.12–14 For radiographic hip OA, available estimates vary more widely, from less than 1% to 27%, depending on the population being studied.15 Radiographic hand OA is common, especially in older individuals, but it may not be symptomatic or functionally limiting. One large study found radiographic OA of at least one joint in 67% of women and 55% of men aged 55 years and older, with 28% having radiographic OA in at least two of three hand joint sites (distal or proximal interphalangeal or carpometacarpal).16 A recent review of radiographic findings in foot OA reported a prevalence of 12% to 35% for first metatarsophalangeal OA.17
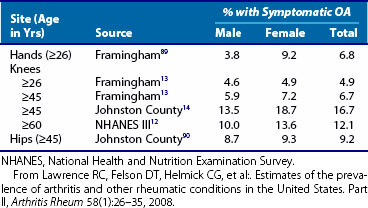
Prevalence of Symptomatic Osteoarthritis
A summary of prevalence estimates for symptomatic OA (symptoms in the presence of radiographic OA) at the hands, knees, and hips is presented in Table 99-2.1 On the basis of these findings, Lawrence and colleagues1 estimated that more than 9 million U.S. adults are affected by symptomatic knee OA and more than 13 million have symptomatic hand OA.
Primary and Secondary Osteoarthritis
Historically, osteoarthritis was considered to be “primary” in the absence of an injury history or other joint disease and “secondary” if a predisposing disorder was present (Table 99-3). However, as more and more local risk factors for OA have been identified (such as femoroacetabular impingement at the hip and malalignment at the knee) and a broader range of associated factors have been discovered (genetic, biomechanical, and environmental factors), the division between primary and secondary is less clear. Many individuals who develop secondary OA are likely predisposed to the condition with or without the identified inciting event; other individuals who have a disorder that is linked to secondary OA may not develop clinical OA. It may be most useful to think of OA as a common pathway through which an individual’s genetics, history of injury or other joint damage, mechanical factors, and psychosocial milieu act on the joint, in some cases leading to an “end-stage” or “failed” joint.
Table 99-3 Etiologies of Secondary Osteoarthritis
| Metabolic |
| Mechanical/Local Factors |
| Traumatic |
| Inflammatory |
ACL, anterior cruciate ligament.
Modified from Altman R, Asch E, Bloch D, et al: Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association, Arthritis Rheum 29(8):1039–1049, 1986.
Clinical Features
General Symptoms and Signs
OA most commonly affects the knees, hands, feet, hips, and spine. These joints may be symptomatic or may be affected only on radiographs. Individuals with OA generally describe pain in the joint(s) that is worse with activity, with limited morning stiffness (<30 minutes), and pain and stiffness with rest. This stiffness after inactivity, or “gelling” phenomenon, is often a main complaint, although morning stiffness is generally less severe and of shorter duration than that seen in systemic inflammatory arthropathies. Affected joints in OA often demonstrate bony enlargement and crepitus on examination, with concomitant reductions in range of motion. There may be soft tissue swelling or effusion, although these tend to be much less dramatic than in inflammatory arthritis. Pain complaints may be more or less than expected on the basis of structural damage.18,19 The effects of depression, disturbed sleep, and other psychosocial factors on the pain experience in OA are being increasingly recognized.20–23
Joint-Specific Symptoms and Signs: Knee
Knee OA is characterized by the insidious onset of pain with gelling and limited range of motion. Individuals with knee OA often describe pain and limitation with walking, transferring (as from seated to standing), and especially stair climbing. These complaints are often associated with a sensation of instability or “giving out” at the knee. A “locking” sensation at the knee can be a consequence of stiffness, loose bodies in the joint space, or meniscal lesions. Knees with OA often have demonstrable crepitus and bony enlargement. Pain may be elicited by palpation of the medial or lateral joint line, or both. Effusions, when present, are often cool and generally without redness. They can be associated with popliteal bursa enlargement (Baker’s cyst) when large. Associated pain over the anserine bursa, or even the greater trochanter, is often seen in knee OA and may be related to altered biomechanics.24 Appreciation of such soft tissue symptoms is important because these may be amenable to corticosteroid injections with subsequent pain relief.
Malalignment, most often varus, is often seen in severe disease but can be present even in fairly mild/early disease. Clinically evident varus thrust may be a risk factor for progression.25 Other signs of severe disease include flexion deformities or joint instability. Quadriceps weakness represents an early modifiable risk factor for knee OA progression, particularly in women,26,27 and in late stages of disease may be apparent as muscle atrophy.28,29 Alterations in proprioception and vibratory sense have been demonstrated in association with knee OA, although the relation of these factors to progression and pain is still unclear.30–32
Patellofemoral OA can strongly contribute to pain and disability at the knee but is often overlooked.33 OA of the patellofemoral joint is characterized by pain with ascending or descending stairs and is often located anteriorly. It can be seen in isolation or in association with tibiofemoral OA. The relation between patellofemoral OA and commonly seen patellofemoral pain disorders in younger individuals remains to be elucidated.34
Joint-Specific Symptoms and Signs: Hip
OA of the hip can present with groin pain, which is fairly specific35 but may be described more vaguely as pain in the thigh, buttock, low back, or even in the ipsilateral knee. Therefore it is important to assess for other causes of pain in the “hip” including spinal pain (lumbar disk degeneration, spinal stenosis, facet joint OA, sacroiliac pain); trochanteric bursitis; altered gait due to knee pathology; meralgia paresthetica (lateral femoral cutaneous nerve entrapment); thigh claudication from vascular causes; or even intrapelvic causes. It is also important to consider other causes of hip and groin pain such as occult femoral neck fracture or avascular necrosis. Persons affected by hip OA have limitations in walking, bending, and transferring, as well as stair climbing. Internal rotation of the affected hip is often limited and can be quite painful, even in early disease, often evident to the patient as difficulty putting on socks, tying shoes, or trimming toenails. Visible deformity, hip flexion contracture, or severe limitations of range of motion are indicators of more advanced disease, which may also be associated with shortening of the affected limb due to superior migration of the femoral head. In young individuals presenting with groin pain that is worsened by sitting, with pain and limitation when internally rotating and adducting the hip in the flexed position, femoroacetabular impingement is a consideration.36
Joint-Specific Symptoms and Signs: Hand
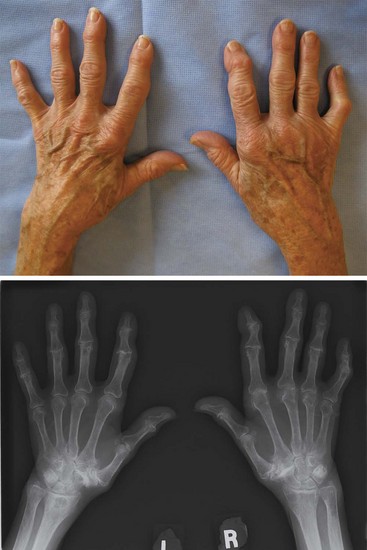
The hands often provide the first clue to a diagnosis of OA. Evident bony enlargement of the distal interphalangeal (DIP) joints, called Heberden’s nodes, and proximal interphalangeal (PIP) joints, called Bouchard’s nodes, can be appreciated (Figure 99-1). These nodes may be acutely inflamed with warmth and tenderness or may be bland, hard enlargements and are often more marked in the dominant hand. Some patients, most commonly elderly women, have erosive osteoarthritis characterized by episodic inflammation, pain, and swelling. It remains a matter of debate whether this type of OA is part of the continuum or is in itself a separate disease entity.37,38 OA involvement of the first carpometacarpal (CMC) joint is particularly problematic and can lead to significant pain, limitations in functionality of the hand, and reduced grip strength.39,40 CMC squaring, representing deformity of the joint due to osteophyte formation and joint space narrowing, can be seen on examination. Bilateral involvement of multiple joints, both within (multiple PIPs) and across (both DIPs and PIPs) joint groups, is frequent. Metacarpophalangeal joints are affected more commonly than previously recognized,41–43 although prominent involvement of these joints should prompt consideration of inflammatory arthropathies or secondary causes of OA such as hemochromatosis.44 Again, soft tissue findings such as deQuervain’s tenosynovitis should be considered because they are associated with hand OA, can mimic or aggravate symptoms, and are amenable to conservative management.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree